- Visibility 354 Views
- Downloads 36 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2025.019
-
CrossMark
- Citation
Prevalence of dry eye disease among medical students in a tertiary care center: A cross sectional study
Abstract
Background: Dry eye disease is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface, it is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface. Aim is to estimate the prevalence of Dry eye disease (DED) among medical students.
Materials and Methods: In this prospective, cross-sectional study, after getting informed consent 100 medical students were evaluated using the Ocular Surface Disease Index (OSDI) questionnaire, average daily screen time and routine ophthalmological examination, Schirmer's test, and tear film break-up time (TBUT) as a screening method for identifying DED. The Data thus collected is entered in Microsoft excel sheet & analyzed using SPSS 20.0 version. Descriptive statistics were applied to summarize the demographic data, comparisons between categorical variables analyzed using Fisher's exact test.
Result: The prevalence of DED among study participants was 43%, with 30% of students having mild DED. There is a significant association between screen time and DED (p<0.05).
Conclusion: The prevalence of DED among medical students is rising as a result of an increase in screen usage.
Introduction
Dry eye disease is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface, it is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.[1] Patients with DED have a reduced quality of life since it makes them more painful, depletes their energy, and makes it harder for them to read and drive, during other tasks as well.[2] All of these things reduce the patients ability to function well in their daily lives and at work.[3]
As little as two hours a day of continuous use of digital devices can cause an array of vision-related problems, including "digital eye strain," according to the American Optometric Association.[4] Depending on the criteria, age, sex, and population under study, the total prevalence of DED can range from 5% to 50%. In a similar studies, additional research have indicated that 3–34% of adult people worldwide suffer from dry eye disease.[5] Asian population often have higher prevalence rates than Caucasian ones, and the prevalence rates increase with age.[6] Early preventative efforts are essential for reducing the burden of DED, considering that it is one of the ocular problems that can potentially be prevented.[4], [7] However a large number of studies have been carried out to explore the nature of DED, very few have attempted to investigate the features of DED among healthcare workers.[8], [9]
Therefore, this study aims to address this gap by investigating the prevalence of DED among medical students, who represent a subset of healthcare professionals in training. By analyzing dry eye parameters and their correlation with average screen time, we seek to elucidate the impact of digital device usage on ocular health in this population. Through a comprehensive examination of these factors, we aim to contribute valuable insights towards the development of effective preventive measures and interventions to alleviate the burden of DED among medical students and, by extension, healthcare professionals.
Materials and Methods
It was a prospective cross-sectional study conducted for a period of 6 months, i.e., from June 2023 to November 2023, on medical students who gave informed consent and fulfilled the inclusion and exclusion criteria. The study was conducted at the Department of Ophthalmology, Alluri Sita Ramaraju Academy of Medical Sciences, Eluru, Andhra Pradesh. The initiation of the study was preceded by obtaining permission from higher authorities and clearance from the Institutional Ethics Committee.
Inclusion criteria
Medical students who are willing to participate are included.
Exclusion criteria
The medical students with Glaucoma, Strabismus, Severe Trauma, contact lens wearers, seborrheic dermatitis, Sjogren syndrome, diabetes mellitus, spring catarrh, undergone refractive surgery for vision correction and Other ocular or eyelid surgeries that may affect the ocular surface health are excluded. The enrolled subjects are classified into two groups based on screen time less than 4 hours and more than 4 hours
The study has been conducted by using questionnaire with two sections:
Demographic data with pre-existing medical conditions and average daily screen time.
Dry eye questionnaire using the ocular surface disease index (OSDI).
All students underwent routine ophthalmological examination along with Schirmer test and tear film break-up time (TBUT) as a screening tool for detecting dry eye disease
Tear film break up time (TBUT): An impregnated fluorescein strip moistened with normal saline is instilled into lower fornix, then patient is asked to blink several times and observed under cobalt blue filter in slit lamp. Breakup time less than 10 sec is considered abnormal. Test is repeated three times and average calculated.
Schirmer’s test: It measures the amount of wetting of Whatman 41 filter paper, according to wetting of the Schirmer strip, five millimeters of the Schirmer strip were folded and kept at the junction of lateral one third and medial two third of the lower eye lids with the eyes open. After five minutes, the strip was removed and the wetting of the strip was measured. Dry eye was graded as normal when the reading was more than 15 mm.
Mild dry eye is 11 - 15 mm
Moderate dry eye is 5 - 10 mm
Severe dry eye is less than 5 mm.
OSDI questionnaire: The 12 questions in the OSDI questionnaire evaluate the following three primary domains of ocular surface disorders in dry eyes are Five questions about the symptoms of chronic dry eye disease 4 about the poor visual performance caused by dry eyes, and 3 about how severe the symptoms were in specific scenarios last week. Overall scores (ranging from 0 to 100) were calculated and categorised into 3 groups. Normal (score 0–12), Mild Symptoms (score 13–22), Moderate Symptoms (score 23–32), and Severe Symptoms (score 33–100).
The data was collected by self-administered method.
Statistical analysis
The collected data was entered in Microsoft Excel 2010 and analysed using SPSS 20.0 version. The results were presented in the form of tables and charts. Descriptive statistics were used to summarise the demographic data, and Fisher's exact test was used for comparisons between categorical variables. A P-value <0.05 is considered to be statistically significant.
Results
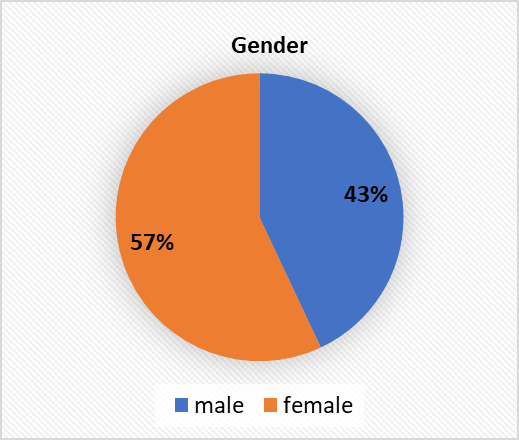
Among the 100 students 43 were females and 57 were females.
|
|
Minimum value |
Maximum value |
Mean ± SD |
|
Age |
19 |
26 |
21.88 ± 1.51 |
|
SCHIRMER |
7 |
25 |
16.66 ± 4.51 |
|
TBUT |
2 |
21 |
12.01 ± 4.86 |
|
OSDI |
4 |
58 |
17.61 ± 13.591 |
[Table 1] shows the descriptive statistics, with the mean age group of study participants being 21.88 ± 1.51, the mean Schirmer value being 16.66 ± 4.51, the mean TBUT value being 12.01± 4.86, and the mean OSDI being 17.61 ± 13.591.
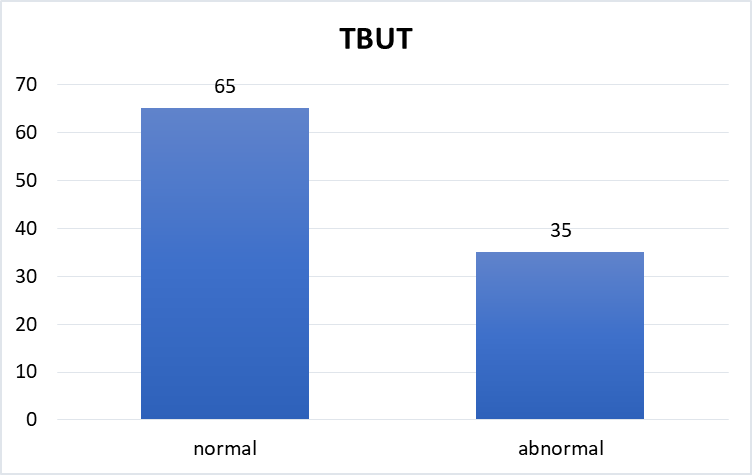
[Figure 1] shows that 35 students had abnormal TBUT less than 10 seconds, while 65 students had normal TBUT.
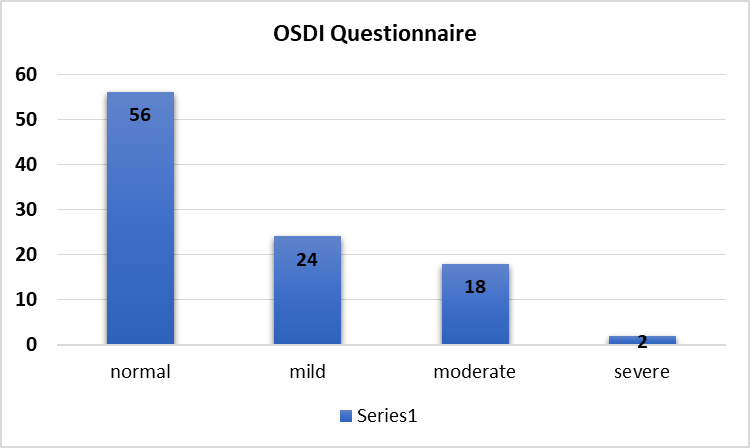
[Figure 3] shows that out of 100 study participants, 56 had normal scores, 24 had mild DED, 18 had moderate DED, and 2 had severe DED.
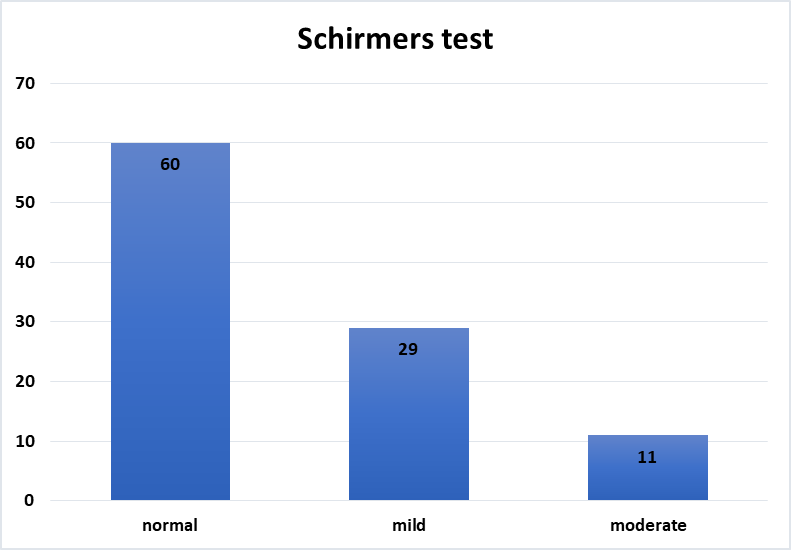
[Figure 4] shows that, according to the schirmers test, 60 students have a normal value, 29 have mild DED, and 11 have moderate DED.
|
Dry Eye Parameters |
Average Screen Time |
Fisher’s Exact Test |
Degree of freedom |
p value |
||
|
≥ 4 hours |
< 4 hours |
|||||
|
OSDI (score) |
Normal |
0 |
56 |
82.35 |
3 |
0.01 |
|
Mild |
20 |
4 |
||||
|
Moderate |
18 |
0 |
||||
|
Severe |
2 |
0 |
||||
|
Total |
40 |
60 |
||||
|
Schirmer’s (value) |
Normal |
0 |
60 |
100.00 |
2 |
0.01 |
|
Mild |
29 |
0 |
||||
|
Moderate |
11 |
0 |
||||
|
Total |
40 |
60 |
||||
|
TBUT (sec) |
Normal |
5 |
60 |
92.00 |
1 |
0.01 |
|
Abnormal |
35 |
0 |
||||
|
Total |
40 |
60 |
A total of 100 students 40 students had an average screen time of ≥ 4 hours, whereas 60 students had an average screen time of <4 hours. Among the 60 students whose average screen time is less than 4 hours, 60 had a normal TBUT and SCHIRMERS value, whereas in OSDI, 56 had a normal score and 4 had a mild DED. In group ≥ 4 hours, according to OSDI, 20 had mild DED, 18 had moderate DED, and 2 had severe DED. Whereas in TBUT, 5 had normal and 35 had abnormal less than 10 sec, according to the schirmers value 29 have mild DED, and 11 have moderate DED. There is a significant association between dry eye parameters and screen time, as the p value is < 0.05.
Discussion
Medical students represent a distinct demographic characterized by rigorous academic demands, long hours of study, and high levels of psychological stress. The demanding nature of medical education often compels students to adopt coping mechanisms, including increased use of electronic devices for study, research, and communication. While these devices facilitate learning and productivity, excessive screen time may inadvertently contribute to the development of ocular health issues, including dry eye disease (DED).
Our study, conducted among medical students, revealed a notable prevalence of symptomatic DED, with 44% of participants reporting symptoms consistent with the condition. This finding underscores the significant impact of prolonged screen exposure and lifestyle factors inherent to medical education on ocular health. Notably, when comparing our results to previous epidemiological surveys on DED, we employed the Ocular Surface Disease Index (OSDI) questionnaire to assess the severity of the disease. Our analysis revealed a spectrum of disease severity among participants, with 2% classified as having severe DED, 18% with moderate DED, and 24% with mild DED.
Our study's findings resonate with existing research endeavors investigating the prevalence of dry eye disease (DED) across various demographics, particularly within the realm of medical education. Yuvashree et al. conducted a study indicating a prevalence of DED at 56.8%, shedding light on the substantial burden of the condition within this cohort.[4] Similarly, Bahkir et al. observed a prevalence rate of 56.5%, with a notable higher incidence among female participants, underlining the gender-related disparities in DED prevalence.[10] These collective findings underscore the widespread nature of DED and emphasize the necessity for targeted interventions to alleviate this prevalent ocular health concern.
In parallel with our investigation, Lin et al. also delved into the prevalence of DED among student populations, reporting a prevalence rate of 60%.[11] Additionally, they utilized the Ocular Surface Disease Index (OSDI) scale to grade the severity of DED, revealing approximately 40% of students classified as having mild DED. According to a study done by Yang I et al. on medical students, severe dry eyes (OSDI score 33) were found in 27.8 percent of cases, compared to 44 percent in our study, and they also used keratography, ocular surface staining, the Schirmer test, and the OSDI score to identify DED.[6]
Similar to our study findings, a study by Logaraj et al. concluded that 70 percent of medical students had DED and there was a strong association between DED and increased screen use.[12] A study by Iqbal et al. found that up to 68% of students who used electronics for more than three hours a day had symptoms of dryness and developed the DED, which is also similar to the findings of our study.[13] According to a study conducted by Patel et al. there is a positive and significant correlation between the stability of the precorneal tear film and increased screen time.[14]
Symptomatic DED was common among medical students, as found in previous studies by Hyon et al. Increased levels of psychological stress was associated with increased risk of DED.[8]
In 2014, Moon et al. evaluated the association between children's smart phone use and symptoms of dry eye in South Korea, and they observed that both symptoms and signs subsided after four weeks of reducing on screen time. Additionally, they observed that exposure to the outdoors prevented against dry eye disease, that offers us all more justification to get outside almost after a year of excessive indoor time.[15] The most important advice we can give our students with dry eye symptoms is to be mindful of their use of electronic devices and to seek out alternative modalities for working, learning, and socializing when possible.
Conclusion
The prevalence of DED among medical students is rising as a result of an increase in screen usage. Awareness about prevention of digital eye strain should be enforced in medical students to bring these adverse effects to a minimum level.
Source of Funding
None.
Conflict of Interest
None.
Acknowledgment
I hereby thank the participants for their active participation in this study.
References
- Craig J, Nichols K, Akpek E, Caffery B, Dua H, Joo C. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15(3):276-83. [Google Scholar]
- Uchino M, Schaumberg D. Dry Eye Disease: Impact on Quality of Life and Vision. Curr Ophthalmol Rep. 2013;1(2):51-7. [Google Scholar]
- Abu-Ismail L, Abuawwad M, Taha M, Khamees A, Ismail D, Sanwar M. Prevalence of Dry Eye Disease Among Medical Students and Its Association with Sleep Habits, Use of Electronic Devices and Caffeine Consumption: A Cross-Sectional Questionnaire. Clin Ophthalmol. 2023;17:1013-23. [Google Scholar]
- Yuvashree, Indhu C, Bhuvaneswari K. Prevalence of Symptomatic Dry Eye Disease Among Undergraduate Medical Students After Covid 19 Pandemic In A Tertiary Care Hospital Kanchipuram- A Cr0ss Sectional Study. J Pharm Negat Results. 2018. [Google Scholar] [Crossref]
- Stapleton F, Alves M, Bunya V, Jalbert I, Lekhanont K, Malet F. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15(3):334-65. [Google Scholar]
- Yang I, Wakamatsu T, Sacho I, Fazzi J, DeAquino A, Ayub G. Prevalence and associated risk factors for dry eye disease among Brazilian undergraduate students. PLoS One. 2021;16(11). [Google Scholar]
- Donthineni P, Shanbhag S, Basu S. An Evidence-Based Strategic Approach to Prevention and Treatment of Dry Eye Disease, a Modern Global Epidemic. Healthcare (Basel). 2021;9(1). [Google Scholar]
- Hyon J, Yang H, Han S. Dry Eye Symptoms May Have Association With Psychological Stress in Medical Students. Eye Contact Lens. 2019;45(5):310-4. [Google Scholar]
- Hyon J, Yang H, Han S. Association between Dry Eye Disease and Psychological Stress among Paramedical Workers in Korea. Sci Rep. 2019;9. [Google Scholar]
- Bahkir F, Grandee S. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J Ophthalmol. 2020;68(11):2378-83. [Google Scholar]
- Lin F, Cai Y, Fei X, Wang Y, Zhou M, Liu Y. Prevalence of dry eye disease among Chinese high school students during the COVID-19 outbreak. BMC Ophthalmol. 2022;22(1). [Google Scholar]
- Logaraj M, Madhupriya V, Hegde S. Computer vision syndrome and associated factors among medical and engineering students in chennai. Ann Med Health Sci Res. 2014;4(2):179-85. [Google Scholar]
- Iqbal M, El-Massry A, Elagouz M, Elzembely H. Computer vision syndrome survey among the medical students in Sohag University Hospital. Ophthalmol Res Int J. 2018;8:1-8. [Google Scholar]
- Patel S, Henderson R, Bradley L, Galloway B, Hunter L. Effect of visual display unit use on blink rate and tear stability. Optom Vis Sci. 1991;68(11):888-92. [Google Scholar]
- Moon J, Kim K, Moon N. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: A case control study. BMC Ophthalmol. 2016;16(1). [Google Scholar]
How to Cite This Article
Vancouver
Radhika K, Pradeep P. Prevalence of dry eye disease among medical students in a tertiary care center: A cross sectional study [Internet]. Indian J Clin Exp Ophthalmol. 2025 [cited 2025 Sep 23];11(1):111-115. Available from: https://doi.org/10.18231/j.ijceo.2025.019
APA
Radhika, K., Pradeep, P. (2025). Prevalence of dry eye disease among medical students in a tertiary care center: A cross sectional study. Indian J Clin Exp Ophthalmol, 11(1), 111-115. https://doi.org/10.18231/j.ijceo.2025.019
MLA
Radhika, Kasilanka, Pradeep, Pakalapati. "Prevalence of dry eye disease among medical students in a tertiary care center: A cross sectional study." Indian J Clin Exp Ophthalmol, vol. 11, no. 1, 2025, pp. 111-115. https://doi.org/10.18231/j.ijceo.2025.019
Chicago
Radhika, K., Pradeep, P.. "Prevalence of dry eye disease among medical students in a tertiary care center: A cross sectional study." Indian J Clin Exp Ophthalmol 11, no. 1 (2025): 111-115. https://doi.org/10.18231/j.ijceo.2025.019
