- Visibility 50 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijceo.2025.013
-
CrossMark
- Citation
Clinicoepidemiological study of penetrating ocular injuries and factors affecting visual outcome
Introduction
Ocular trauma is a term used to encompass physical or chemical injuries to the eye or eye socket. This commonly occurs through eye scratching or exposure to toxic chemicals, while more severe injuries can result from major traumas.[1] It is a significant factor contributing to visual impairment, with the WHO reporting that approximately 55 million people worldwide experience serious ocular trauma, leading to limitations in their daily activities.[2] The treatment cost for ocular trauma is high, visual outcomes are predominantly poor.
Based on the data from the National Sample Survey Organization in 1991, prevalence of trauma-related visual impairment was 3.5% in rural areas and 3.2% in urban areas.[3] The lack of awareness about this issue hampers preventive efforts in addressing it.[2] The potential loss of person-days of work associated with treating the consequences of trauma can be enormous.[4] Eye injuries can have negative effects, such as vision loss and physical deformity, which can isolate the affected individuals socially and create psychological and physical barriers. In fact, a significant proportion of reported eye injuries come from job-related incidents, violence, and games.[5]
Ocular trauma remains a preventable cause of visual impairment, but its impact on patients and their families is significant, encompassing socioeconomic, physical, emotional, and vocational aspects. Males in economically productive age groups are more susceptible to ocular trauma, leading to the loss of livelihood for breadwinners in many cases, thereby affecting the entire family's socioeconomic status.[6] Therefore, it is crucial to emphasize information about protective gear and its significance while implementing suitable measures for the physical, mental, social, and vocational rehabilitation of patients with the assistance of the National Program for Control of Blindness.
Ocular trauma can be categorized into open globe and closed globe injuries.[7] Therefore, the Ocular Trauma Society of India has proposed an India Eye Injury Registry which would enable standardization and evaluation protocols, facilitate data collection for the epidemiology of ocular trauma cases and their treatment outcomes, propose clinical trials, and disseminate essential information.[8]
This particular study aimed to examine the epidemiological characteristics of open globe ocular injuries (OGIs).[9] Thus, this study was conducted to assess the factors and clinic-epidemiological profile in such cases and correlate them with the visual prognosis at a tertiary care hospital in Bhopal (M.P.).
Materials and Methods
The present study was conducted in the Department of Ophthalmology at Gandhi Medical College, Bhopal. Detailed history of patients was taken and socioeconomic status (modified Kuppuswamy classification), date and time of injury, time laps between injury and hospital attendance, mode, nature and object causing injury, time and place of primary repair and preventive measures used at time of injury.
Distant visual acuity was recorded by Snellen’s chart in literate people and Land lot's broken ring of E type chart in preschool and illiterate people, projection of rays was also recorded in all quadrants. Starting from condition of face, forehead and adnexa was noted.
Anterior segment examination was done by torch light and slit lamp which included examination of conjunctiva, cornea, sclera, anterior chamber, iris, pupil, lens for subluxation, dislocation, capsular breach, fragmentation, cataract and vitreous prolapse in AC and wound.
Examination of posterior segment was done by Direct ophthalmoscopy, Indirect ophthalmoscopy, slit lamp, Biomicroscopy which included examination of vitreous, and retina. Plain X-ray AP and lateral views for evaluate injured eye and orbit to assess intraocular and extra ocular injuries and fractures. USG B-scan for presence/absence of eye wall wounds, IOFBs (whether these are radiolucent or opaque), also about the exact localization of the intraocular foreign body, lens/IOL dislocation, posterior capsular breach, vitreous incarceration into a wound, post operatively for condition of posterior segment.
Careful assessment was done with ultrasonography of eye for open globe injury. All cases were treated by appropriate surgery and during surgery true extent of wound and any intraoperative complications were noted. Condition of eye on discharge was also recorded.
The patients were followed up for minimum 6 months and all the cases were studied in accordance with eye trauma terminology system and ocular trauma classification group. OTS was assigned according to BETTS classification. Patients were divided into six groups for final visual acuity assessment. Patient were also divided as per WHO blindness and visual impairment classification. Further the cases were also grouped as per their type of injury for ease of evaluation and comparison.
Results
[Table 1] llustrates the distribution of epidemiological and etiological factors. The majority of participants (66%)were in working age groups (16-64 years). The study reveals a higher prevalence of ocular injury among the working age group (66%), likely due to their increased likelihood of sustaining open globe injuries at their workplaces or during outdoor activities. Penetrating ocular injuries showed a male preponderance (78%). Geographically, most of the participants hailed from rural areas 54.0%, while urban areas have 46%.
Educational status distribution exhibited a bimodal pattern, with 28% of participants with open globe ocular injury being illiterate, and 28% educated up to 12th standard. Only 14% of the participants were graduates. Notably, 86% of the study participants had an education level lower than or up to high school, indicating a higher occurrence of ocular injury among subjects with lower educational status.
Socio-economic status, revealed that the majority of participants belonged to upper lower class (50.0%). Only 2% of the participants were from Upper Class, while 6% were classified as Upper Middle Class. The study observed that 68% of cases were associated with lower class, suggesting a higher prevalence of open globe injuries within the lower socioeconomic class.
For etiological factors, distribution of participants based on the location of ocular injury indicates that over 90% experienced penetrating injuries outside their homes. These injuries were primarily attributed to workplace-related incidents (50%). Injuries occurred on roadsides or during outdoor activities (44%). Only 6% of the injuries were observed to occurred within domestic settings.
Etiology of injury, the most prevalent injury was projectile metal pieces (38%) resulting from workplace trauma. Following this, animal horns/bites 14%, while injuries caused by projectile stone/brick pieces, vegetative matter/wooden twigs/wooden pieces, and glass pieces each constituted 12%. Assault-related injuries were 8% of ocular trauma, and 4% by road traffic accidents (RTA).
[Table 2] provides the clinical profile of the participants. The majority of injuries were unilateral (94%), with the left eye being mostly affected (52%). Only 6% of cases had bilateral eye involvement, and these were primarily caused by blast injuries and windshield injuries. Among open globe injuries, a significant portion (58.5%) was of a penetrating nature, resulting from projectile metal, wooden, or glass pieces. Globe rupture due to blunt trauma from animal horns, bricks, stones, or assault by hand or elbow was observed in 28.3% of cases. In 9.43% of participants, penetrating injuries with retained intraocular foreign bodies (IOFB), and these injuries were attributed to blast injury or iron particles. Perforating and mixed types of injuries were relatively rare (1.8%).
The distribution of participants based on visual acuity at presentation, a significant number (almost 80%) had a substantial reduction in vision (<6/60), and vision loss in 28% of all open globe injuries. In terms of zone-wise distribution in open globe injuries, the majority were in Zone I (49%), followed by Zone II (34%). Zone I injuries are exposed to the external environment, which explains their prevalence in cases of penetrating or perforating injuries. Zone III injuries (17%) were less common and were mostly associated with globe rupture or blunt trauma. When considering the distribution according to the Ocular Trauma Score (OTS), most open globe injury with OTS was 3 (34%). Approximately 50% presented with a very low OTS score of <-2, indicating severe and extensive ocular damage with visual loss.
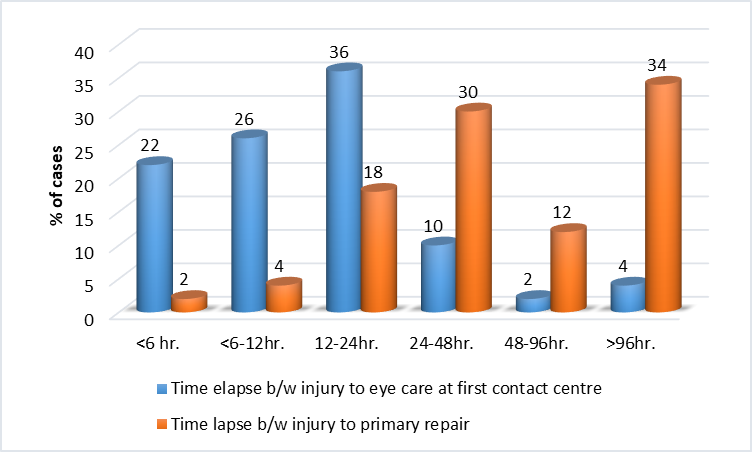
[Figure 1] illustrates the time elapsed between ocular injuries and the initiation of eye care at the first contact center. A significant number of patients (84%) reached the first contact center within 24 hours of the injury, and these were individuals who had access to nearby hospitals Only 24% of cases underwent repair within 24 hours because the majority of patients were referred cases, leading to their arrival at the tertiary care center after the crucial initial 24-hour period, which is essential for the outcome and surgical repair to be planned accordingly. Since some of these cases were infected, the surgical repair was done under antibiotic coverage, causing delays in the primary repair process.
[Table 3] presents the ocular examination of the participants. Bony orbital injuries were 3.8% who suffered >2 orbital wall fractures. These were seen in injuries caused by animal bites and swords. As penetrating injuries are typically caused by flying projectile objects, bony orbital injuries are not very common. Lid laceration was found in less cases (5.7%), and only one case experiencing tissue loss (1.9%).
The most common finding of conjunctiva was sub-conjunctival haemorrhage (37.7%). Of all participants, 51% had an intact cornea, while 49% had corneal lacerations. Among corneal lacerations, 24.5% had lacerations of <5 mm and 24.5% involved the pupillary area.
Full-thickness scleral wounds were observed in 50.9% of cases. The anterior chamber content was normal in 15%. The most commonly observed condition was hyphema (43.3%), followed by foreign body (FB)7.5%, lens involvement 3.80%, and fibrin membrane in 3.80% of cases.
The anterior chamber depth was shallow in 30.18% of cases. Iris tissue incarceration in the laceration wound was observed 32%, while iridodialysis was observed in a single case. Pupil evaluation was not possible in 53.24% of cases, sphincter tears were observed in 5.70% of cases.
Traumatic cataracts were observed in 28.3%, capsular breach in 5.66%, and anterior dislocation of the lens in 3.80% of cases. Fundus evaluation was non-commentable in 81.13%, pre-retinal hemorrhage with retinal detachment in 1.90% of cases, superficial retinal hemorrhage in 1.90%, and faint red glow/disc with faintly visible blood vessels in 7.54% of cases. Non-commentable fundus conditions were attributed to corneal tears, scleral tears extending into the cornea, hyphema, iris tissue incarceration in the lacerated wound, and traumatic cataracts.
The cases that underwent surgical repair, primary repair was performed in 75.4% of cases. In 7.5% of cases, primary repair involved lens extraction with aphakia. Secondary posterior chamber intraocular lens (PCIOL) implantation was performed in 7.5% of cases, while secondary lens aspiration with anterior vitrectomy and PCIOL implantation was done in 3.8% of cases.
B-scan findings in the revealed that 72% of the patients had normal B-scans. Vitreous hemorrhage was observed in 11.6%, while retained intraocular foreign body (RIOFB) and endophthalmitis were each observed in 6.9% of cases. Retinal detachment was detected in 2.3% of cases.
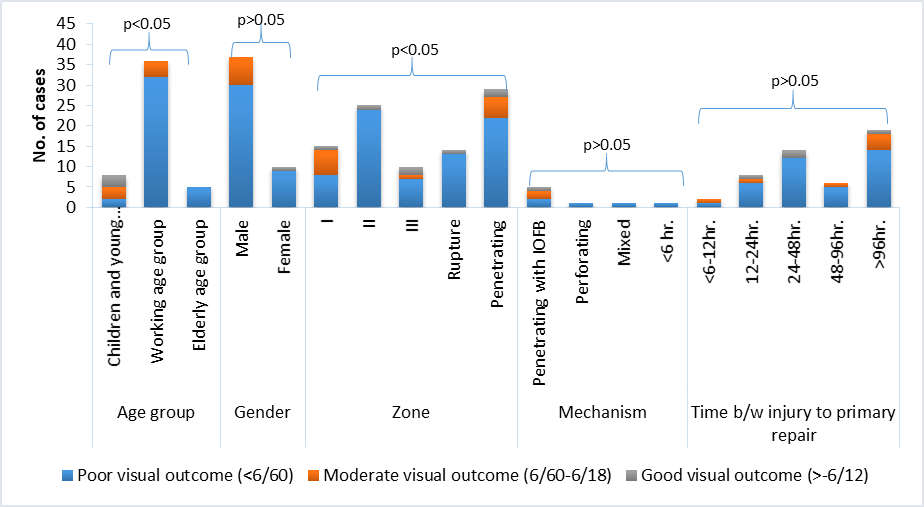
[Figure 2] displays the final visual outcome of the study participants with penetrating ocular injuries. Poor final visual outcomes were most commonly observed in working-age groups (32, 82.1%) and zone II injuries (24, 61.5%). However, no significant association was observed between gender, mechanism of injury, and time lapse between injury and primary repair with the final visual outcome.
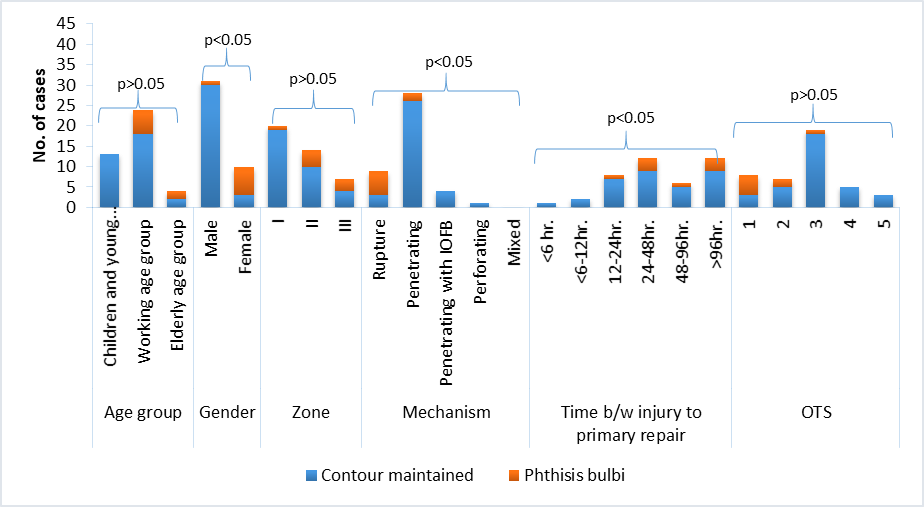
[Figure 3] shows the final structural outcome of the participants with penetrating ocular injuries. Poor final structural outcomes (phthisis bulbi) were more prevalent in female patients (7, 87.5%), type I injuries comprising 75%, and cases with a time lapse between injury and primary repair of over 24 hours (7, 87.5%), showing statistical significance (p-value <0.05). However, no significant association was observed between age group, zone of injury, and the Ocular Trauma Score (OTS). The association with females may be misleading, as it was observed that out of the 7 females who developed phthisis, 6 of them had type 1 injuries.
|
|
Variable |
No. of cases |
Percentage (%) |
|
|
Epidemiological factors |
|
Children and young adolescents |
12 |
24 |
|
Age (years) |
Working age groups |
33 |
66 |
|
|
|
Elderly age group |
5 |
10 |
|
|
Gender |
Male |
39 |
78 |
|
|
|
Female |
11 |
22 |
|
|
Area of residence |
Urban |
23 |
46 |
|
|
|
Rural |
27 |
54 |
|
|
|
Illiterate |
14 |
28 |
|
|
|
Primary school |
7 |
14 |
|
|
Educational status |
Middle school |
8 |
16 |
|
|
|
High school |
14 |
28 |
|
|
|
Graduate/PG |
7 |
14 |
|
|
|
Lower class |
9 |
18 |
|
|
|
Upper lower class |
25 |
50 |
|
|
Socioeconomic status |
Lower middle class |
11 |
22 |
|
|
|
Upper middle class |
3 |
6 |
|
|
|
Upper class |
2 |
4 |
|
|
Etiological factors |
|
Work place (Occupation Related) |
25 |
50 |
|
Place of injury |
Home (Domestic) |
3 |
6 |
|
|
|
During outdoor activities/roadside |
22 |
44 |
|
|
|
Wooden & Vegetative matter |
6 |
12 |
|
|
|
Glass & ceramic |
6 |
12 |
|
|
|
Metal pieces |
Metal particles |
17 |
34% |
|
Aetiology |
|
Blast injury |
2 |
4% |
|
|
Road accident |
2 |
4 |
|
|
|
Animal Bite & Horn |
7 |
14 |
|
|
|
Physical assault |
4 |
8 |
|
|
|
Stone & bricks |
6 |
12 |
|
|
|
Variable |
No. of cases |
Percentage (%) |
|
Laterality |
Unilateral |
Right eye |
21 |
42.0% |
|
Left eye |
26 |
52.0% |
||
|
|
Bilateral |
3 |
6.0% |
|
|
|
Rupture |
15 |
28.3% |
|
|
|
Penetrating |
31 |
58.5% |
|
|
Mechanism / Type of Injury |
Penetrating with IOFB |
5 |
9.43% |
|
|
|
Perforating |
1 |
1.8% |
|
|
|
Mixed |
1 |
1.8% |
|
|
|
No PL |
15 |
28.3% |
|
|
|
PL + - HM+ |
17 |
32.0% |
|
|
Grade of injury on presenting visual acuity |
CF close to Face PR -5/60(1.08) |
10 |
18.8% |
|
|
|
6/60-6/18(1.0-0.48) |
5 |
9.4% |
|
|
|
≥6/12(0.3) |
4 |
7.5% |
|
|
|
Uncooperative |
2 |
3.7% |
|
|
|
I |
26 |
49.0% |
|
|
|
II |
18 |
33.9% |
|
|
|
III |
9 |
17.0% |
|
|
|
OTS |
|
|
|
|
Zone of injury |
1 |
16 |
30.18% |
|
|
|
2 |
10 |
18.9% |
|
|
|
3 |
18 |
34% |
|
|
|
4 |
6 |
11.3% |
|
|
|
5 |
3 |
5.7% |
|
Variable |
No. of cases |
Percentage (%) |
||
|
|
Single orbital wall fracture |
0 |
0.00 |
|
|
Bony orbital |
2 orbital walls fracture |
0 |
0.00 |
|
|
Injury |
>2 orbital walls fracture |
2 |
3.80 |
|
|
Lids |
Lid laceration without tissue loss |
3 |
5.70 |
|
|
|
Lid laceration with tissue loss |
1 |
1.90 |
|
|
Conjunctiva |
Subconjunctival Haemorrhage |
20 |
37.70 |
|
|
|
Intact |
27 |
50.94 |
|
|
|
Corneal laceration |
26 |
49.00 |
|
|
|
Corneal laceration <5 mm |
13 |
24.50 |
|
|
Cornea |
Corneal laceration >5 mm |
13 |
24.50 |
|
|
|
Pupillary area involving corneal laceration |
13 |
24.50 |
|
|
|
Non-pupillary involving corneal laceration |
13 |
24.50 |
|
|
Sclera |
Intact |
26 |
49.00 |
|
|
|
Laceration |
27 |
50.94 |
|
|
|
Depth |
Normal |
11 |
20.75 |
|
Shallow |
16 |
30.18 |
||
|
|
|
Deep |
1 |
1.90 |
|
|
Content |
Normal |
8 |
15.00 |
|
Hyphema |
23 |
43.39 |
||
|
Lens |
2 |
3.80 |
||
|
Anterior chamber |
|
Foreign body |
4 |
7.50 |
|
|
|
Vitreous |
0 |
0.00 |
|
|
|
Fibrin membrane |
2 |
3.80 |
|
|
Non commentable |
5 |
9.40 |
|
|
Iris |
Iris tissue incarceration in the laceration wound |
17 |
32.00 |
|
|
|
Iridodialysis |
1 |
1.90 |
|
|
|
Non commentable |
24 |
53.24 |
|
|
|
Normal |
2 |
3.80 |
|
|
Pupil |
APD/RAPD |
0 |
0.00 |
|
|
|
Sphincter tear |
3 |
5.70 |
|
|
|
Traumatic Cataract |
15 |
28.30 |
|
|
Lens |
Lens dislocation |
2 |
3.80 |
|
|
|
Lens Subluxation |
0 |
0.00 |
|
|
|
Capsular breach |
3 |
5.66 |
|
|
|
Non commentable |
43 |
81.13 |
|
|
|
Vitreous haemorrhage |
0 |
0.00 |
|
|
Fundus (on presentation) |
Normal |
4 |
7.54 |
|
|
|
Preretinal haemorrhage with RD |
1 |
1.90 |
|
|
|
Superficial haemorrhage |
1 |
1.90 |
|
|
|
Faint red glow/disc and blood vessels faintly visible |
4 |
7.54 |
Discussion
Ocular traumatic injuries are a significant cause of visual impairment, leading to substantial social and economic burdens that impact the quality of life, particularly in young individuals.[10] This study focused on investigating the epidemiology and etiological factors of penetrating ocular injuries, including associated risk factors, within a sample of the central Indian population.
The majority of participants with Open Globe injuries were males (78%). Our study findings were consistent with several studies, including those conducted by Parmar et al,[11] Nirmalan et al.,[12] Vats et al.,[13] Agrawal et al.,[14] Gogate et al. [12], Katiyar et al,[15] Pranjna et al.,[16] Chaudhary et al.,[17] Wagh and Tidake,[18] where they also reported a predominance of male. For instance, Jain and Soni reported a male-to-female ratio of 2.2:1,[19] while Casson et al. found 4:1,[20] and Iqbal et al. stated a male-to-female ratio of 4.92:1.[21]
Among the participants, 66% fell within the working age group, 24% were children and young adolescents, and only 10% were of the elderly age group. Similar distributions were noted by Parmar et al.,[11] Desai also observed the highest incidence in the age group of 21-30 years,[22] and Vasu et al. found that most patients were between 16 and 45 years of age,[23] whereas Singh et al study indicated that the majority of ocular trauma cases were under 14 years of age.[24]
In our study, the distribution between patients from urban and rural areas was almost similar, with a slightly higher proportion of rural patients (54%). Similar findings were also observed by Narang et al.,[25] Desai et al.[22] In contrast, Singh et al. found that only 36.1% of cases were from rural areas.[24] Similarly, Shoja and Miratishi found that 60% of children with ocular trauma resided in urban areas.[26]
In our study, we noticed a bimodal distribution in educational levels: 28% with open globe ocular trauma were illiterate, while 28% had education up to the 12th standard. Additionally, 14% of the participants had completed education till primary school, and 16% had education up to middle school. Only 14% of the participants were graduates. As a result of poor literacy and awareness, participants were not wearing any protective gear at the time of their injuries. A.K. Khan also observed a similar pattern of the subjects being illiterate and having no formal education.[27] Similar findings were also found by Huabin Luo.[28]
In our study, Modified Kuppuswamy Scale was used for socio-economic status (SES), we determined that half of participants belonged to Upper Lower Class, 18% were Lower Class, and 22% were Lower Middle Class. Only 2% of the study participants were Upper Class, and 6% to Upper Middle Class. Similar findings were observed by Gogate et al.[29]
In our study, we observed that 50% of patients with open globe ocular trauma experienced their injuries at their workplace. On the other hand, 44% of the participants suffered ocular trauma due to RTA or other causes, while only 6% of the participants sustained injuries at home. Vasu et al. they reported that only 33.3% of the injuries were related to occupational hazards.[23] Narang et al., in their study found that the majority of injuries occurred during outdoor sports.[25] Similarly, Sahu et al. reported that 50% of participants experienced eye trauma while working at home.[30] Maurya et al. also found non-occupational injury as the most common cause.[31] On the other hand, Ababneh et al. identified RTA as the most common cause of ocular trauma (60.7%).[32] Park et al. observed similar findings.[33]
In our study, the majority of open globe injuries were of a penetrating nature (58.5%). Rupture of the globe were in 28.3% cases, while 9.43% had penetrating injuries with an intraocular foreign body (IOFB). Perforating and mixed types of injuries were only 1.8%. Narang et al. in their analysis found that the majority of injuries were Type B.[25] Tripathy et al.[34] also found similar result. However, Chaudhary et al., observed blunt trauma cases to be slightly more common at 51.6% than penetrating injuries.[17]
In our study, we found that metal pieces were the most common mode of injury (38%). This was followed by injuries caused by animal bites and horns i.e. 14% of the cases. Physical assault was 8%, while RTA were responsible for 4% of the cases.
Occupation-related injuries were major cause of ocular trauma in our study, with injuries from metal pieces, glass, work instruments, stones, and bricks were 62% of the causative factors of trauma. Similar findings were reported by Vasu et al., where they stated 37.5% of the injuries were caused by sickles and sticks, and 12.5% were due to bull gore injuries. In the iron and steel industry, 63.15% were suffered by lathe machines and 36.84% by grinding machines.[23]
Maurya et al. reported non-occupational injuries as the most common cause (82.3%). Assault accounted for 17.2% of the injuries, and domestic accidents for 15.2%, while mechanical injuries were caused mainly by wooden objects (24.9%), metallic objects (20.9%), stones (16.7%), balls (6.0%), and glass (3.7%).[31] Wagh and Tidake also observed that RTA was the most common cause of trauma, i.e. 56.67%.[18]
In our study, majority of patients (36.0%) visited the first contact center within 12-24 hours after the injuries. 86% of the participants sought medical attention at a first contact centre within one day. Additionally, 10% of the cases sought medical help within 24-48 hours, 2% within 48-96 hours, while 4% visited after 96 hours. Regarding the time elapsed between injuries and primary repair, we found that in the majority of cases (34%), the repair was done more than 96 hours after the injury. In 30% of cases, the repair was conducted within 24-48 hours, and in 12% of cases, it was done within 48-96 hours. Only 2% of cases received primary repair within less than 6 hours. This delay in treatment could be attributed to factors such as the distance of the center from the site of injury, time spent during referral to a higher center, and poor healthcare-seeking behavior of the patients, among other reasons.
Similar findings were observed by Narang et al., where they reported that 45.83% of patients presented within 24 hours of trauma, 18.06% between 24-72 hours, and 30.56% beyond 72 hours of trauma.[25] Similarly, Alem et al. also observed that the majority of patients (97.02%) presenting with ocular trauma were intervened after 12 hours from the time of trauma, with only 1.29% of the total patients being treated within 6 hours.[35]
Maurya et al. also observed that in 60.7% of cases, the time elapsed at presentation was > 1-24 hours, in 24.4% of cases, it was <1 hour, and 14.4% received treatment the next day after 24 hours.[31] Similarly, Gogate et al. found that the delay between trauma and the time of presentation to the hospital ranged from the same day to 12 years after the injury, with a median of 4 days.[29]
We noticed that the majority, 49% of the participants, experienced ocular trauma in Zone I. Zone II accounted for 33.9% of the injuries, while Zone III represented only 17%. Pure corneal injuries were observed in 49%, corneo-scleral injuries in 28.3%, and pure scleral injuries in 22.7%. Similar findings were reported by Narang et al. on pediatric cases of open globe injury, where 63.89% had sustained Zone I injury.[25] In the retrospective record-based study by Tripathy et al., they found closed globe injuries in 116 eyes and open globe injuries in 29 eyes. The most common type in closed globe injuries was Type A: contusion (79%) in Zone I (72%), while in open globe injuries, the most common type was Type B or penetrating (48%) in Zone II (38%).[34] Conversely, Alem et al. observed that closed and open globe injuries occurred with almost equal frequency.[35] In another study by Kwon et al., the highest incidence rates were observed in hyphema, followed by blunt ocular injuries, and then open globe injuries, respectively.[36]
In the majority of open globe injury cases, had Ocular Trauma Score (OTS) of 3 (34%) and least score 5 (5.7%). Approximately 50% of the patients had a very low OTS score of <2, indicating severe and extensive ocular damage with visual loss. The Ocular Trauma Score was instrumental in categorizing all the cases in our study. Similarly, Sii et al. also reported that increasing injury severity was associated with worse presenting visual acuity according to the BETT system (p=0.006).[37] In another study by Park et al. found that both the BETTS and OTS were good predictors of final visual acuity (VA).[33] However, Malik et al. pointed out that 70% of all ocular traumas could not be categorized by BETTS, as the classification does not include superficial eye, adnexal lid, lacrimal, or orbital injuries.[38]
We found that the final visual outcome of the majority of participants with penetrating ocular injuries was significantly associated with their age and the zone of injury. Poor visual outcomes were particularly prevalent in the working age groups (82.1%) and zone II injuries (61.5%). In study conducted by Agrawal et al. concluded that after four months of treatment, 65.9% of participants achieved better visual acuity (VA). Correlation analysis revealed that age, preoperative VA, mode of injury, and time lag between injury and surgery were significantly associated with the final VA at the univariate level. However, in the multivariate analysis using binary logistic regression, only age, mode of injury, and the time lag between injury and surgery were found to be significantly associated.[14] Gogate et al. also found that visual outcome (≥6/18) depended on the type of surgery, gender, and type of injury, with sharp trauma and open globe injury showing poorer outcomes in univariate analysis.[29] Vasu et al. observed that a fair visual outcome was seen in 11.4% of cases, while the majority (82.9%) of patients had a poor visual outcome, and none of them were using protective eyewear at the time of injury. Moreover, 42.85% had no perception of light.[23]
Our study revealed that gender, mechanism of injury, and the time elapsed between injury and primary repair were significant factors associated with the final structural outcome. In contrast, Vasu et al. reported that 45.71% of patients developed phthisis bulbi, 7.14% had macular scars, and one patient developed endophthalmitis and underwent evisceration six months after the ocular trauma.[23] Jung et al. also observed that 7.7% of patients progressed to phthisis bulbi, resulting in globe loss.[39]
Conclusion
In conclusion, our study found age of the study participants and zone of injury to be significant factors associated with the visual outcome of the patients. Meanwhile, gender, mechanism of injury of the ocular trauma, and the time elapsed between injury and primary repair were significant factors associated with the final structural outcome. To reduce ocular injuries, regular campaigns should be conducted to raise awareness about the importance of using protective eye gear. Implementing legislation to hold employers accountable for providing protective equipment to their employees is crucial. The National Programme for Control of Blindness (NPCB) should include provisions for the physical, mental, social, and vocational rehabilitation of patients affected by ocular trauma.
Source of Funding
None.
Conflict of Interest
None.
References
- A Garg, AS Patel, L Al-Aswad, GL Legault, DB Moore, M Shah. Ocular Trauma: Acute Evaluation, Cataract, Glaucoma. 2023. [Google Scholar]
- AD Négrel, B Thylefors. The global impact of eye injuries. Ophthalmic Epidemiol 1998. [Google Scholar]
- K Jha. Ocular trauma has fallen on our blind spot. J Clin Ophthalmol Res 2016. [Google Scholar]
- S Krishnaiah, PK Nirmalan, BR Shamanna, M Srinivas, GN Rao, R Thomas. Ocular trauma in a rural population of southern India: the Andhra Pradesh Eye Disease Study. Ophthalmology 2006. [Google Scholar]
- RP Maurya, A Kumar, VP Singh. Pattern of pediatric ocular trauma in a Eastern Uttar Pradesh. Indian J Clin Exp Ophthalmol 2017. [Google Scholar]
- A Dawood. A Brief Overview of Occular Trauma. Arch Trauma Res 2014. [Google Scholar]
- F Kuhn. Strategic Thinking in Ocular Traumatology. Ocular Traumatology . [Google Scholar]
- S Natarajan. Ocular trauma, an evolving sub specialty. Indian J Ophthalmol 2013. [Google Scholar]
- S Duke-Elder. . System of ophthalmology 1958. [Google Scholar]
- ED Costa, TM Gomes, TA Mendes, MA Campos, RH Bertrand, LM Pinto. Epidemiological profile and visual outcome of ocular trauma in a referral center in northeastern Brazil. Rev Bras Oftalmol 2019. [Google Scholar]
- IP Parmar, RC Nagpal, S Sunandan. Pattern of ocular injuries in Haryana. Indian J Ophthalmol 1985. [Google Scholar]
- PK Nirmalan, J Katz, JM Tielsch, AL Robin, RD Thulasiraj, R Krishnadas. Ocular trauma in a rural south Indian population: the Aravind Comprehensive Eye Survey. Ophthalmology 2004. [Google Scholar]
- S Vats, GVS Murthy, M Chandra, SK Gupta, P Vashist, M Gogoi. Epidemiological study of ocular trauma in an urban slum population in Delhi, India. Indian J Ophthalmol 2008. [Google Scholar]
- R Agrawal, G Rao, R Naigaonkar, X Ou, S Desai. Prognostic factors for vision outcome after surgical repair of open globe injuries. Indian J Ophthalmol 2011. [Google Scholar]
- V Katiyar, S Bangwal, SK Gupta, V Singh, K Mugdha, P Kishore. Ocular trauma in Indian pediatric population. J Clin Ophthalmol Res 2016. [Google Scholar]
- M Prajna, A Saxena, A Balasubramanian. Health-seeking behavior and the initial economic impact of patients with open globe injuries seeking treatment in a tertiary care center in India. Indian J Ophthalmol 2021. [Google Scholar]
- A Chaudhary, R Singh, SP Singh. Prognostic value of Ocular Trauma Score and pediatric Penetrating Ocular Trauma Score in predicting the visual prognosis following ocular injury. Rom J Ophthalmol 2022. [Google Scholar]
- V Wagh, P Tidake. Clinical Study and Profile of Ocular Trauma: Findings From a Rural Hospital in Central India. Cureus 2022. [Google Scholar]
- BS Jain, SR Soni. Ocular injuries: an analytical study in a teaching general hospital. Indian J Ophthalmol 1987. [Google Scholar]
- R J Casson, JC Walker, HS Newland. Four-year review of open eye injuries at the Royal Adelaide Hospital. Clin Exp Ophthalmol 2002. [Google Scholar]
- U Iqbal, IQ Malik, H Iqbal. Epidemiology of Ocular Trauma in a Tertiary Hospital Setting. Pakistan J Ophthalmol 2019. [Google Scholar]
- P Desai, CJ Macewen, P Baines, DC Minassian. Epidemiology and implications of ocular trauma admitted to hospital in Scotland. J Epidemiol Community Health 1996. [Google Scholar]
- U Vasu, A Vasnaik, RR Battu, M Kurian, S George. Occupational open globe injuries. Indian J Ophthalmol 2001. [Google Scholar]
- DV Singh, YR Sharma, RV Azad, D Talwar, Rajpal. Profile of ocular trauma at tertiary eye centre. JK Sci 2005. [Google Scholar]
- S Narang, V Gupta, P Simalandhi, A Gupta, S Raj, MR Dogra. Paediatric Open Globe Injuries. Visual Outcome and Risk Factors for Endophthalmitis. Indian J Ophthalmol 2004. [Google Scholar]
- MR Shoja, AM Miratashi. Pediatric Ocular Trauma. Acta Med Iran 2006. [Google Scholar]
- AK Khan. Ocular injury: Prevalence in different rural population of Bangladesh. Bangladesh Med Res Counc Bull 2013. [Google Scholar]
- H Luo, GLA Beckles, X Fang, JE Crews, JB Saaddine, X Zhang. Socioeconomic Status and Lifetime Risk for Workplace Eye Injury Reported by a US Population Aged 50 Years and Over. Ophthalmic Epidemiol 2012. [Google Scholar]
- P Gogate, M Sahasrabudhe, M Shah, S Patil, A Kulkarni. Causes, epidemiology, and long-term outcome of traumatic cataracts in children in rural India. Indian J Ophthalmol 2012. [Google Scholar]
- B Wadwekar, AK Mishra, P Sahu, E Sanjana, M Manikandan. Burden of ocular trauma and its effect on vision: A community-based cross-sectional study in the coastal population of South India. J Curr Res Sci Med 2021. [Google Scholar]
- RP Maurya, T Srivastav, VP Singh, CP Mishra, A Al-Mujaini. The epidemiology of ocular trauma in Northern India: A teaching hospital study. Oman J Ophthalmol 2019. [Google Scholar]
- LT Ababneh, H Mohidat, H Abdelnabi, MF Kana'an, NA Tashtush, OS El-Mulki. Hospital-based ocular trauma: Factors, treatment, and impact outcome. Clin Ophthalmol 2019. [Google Scholar]
- J Park, SC Yang, HY Choi. Epidemiology and Clinical Patterns of Ocular Trauma at a Level 1 Trauma Center in Korea. J Korean Med Sci 2021. [Google Scholar]
- K Tripathy, R Chawla, P Venkatesh, R Vohra, YR Sharma. Clinical profile of medicolegal cases presenting to the eye casualty in a tertiary care center in India. Indian J Ophthalmol 2016. [Google Scholar]
- KD Alem, DD Arega, ST Weldegiorgis, BG Agaje, EG Tigneh. Profile of ocular trauma in patients presenting to the department of ophthalmology at Hawassa University: Retrospective study. PLoS One 2019. [Google Scholar]
- JW Kwon, MY Choi, JM Bae. Incidence and seasonality of major ocular trauma: a nationwide population-based study. Sci Rep 2020. [Google Scholar]
- F Sii, RJ Barry, J Abbott, RJ Blanch, CJ MacEwen, P Shah. The UK paediatric ocular trauma study 2 (POTS2): Demographics and mechanisms of injuries. Clin Ophthalmol 2018. [Google Scholar]
- AH Malik, AA Shah, I Ahmad, BA Shah. Ocular Injuries in Patients of Zygomatico-Complex (ZMC) Fractures. J Maxillofac Oral Surg 2017. [Google Scholar]
- HC Jung, SY Lee, CK Yoon, UC Park, JW Heo, EK Lee. Intraocular Foreign Body: Diagnostic Protocols and Treatment Strategies in Ocular Trauma Patients. J Clin Med 2021. [Google Scholar]
