- Visibility 659 Views
- Downloads 51 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2024.002
-
CrossMark
- Citation
Therapeutic potential of vitamin supplements in dry eye disease: A comprehensive review
Abstract
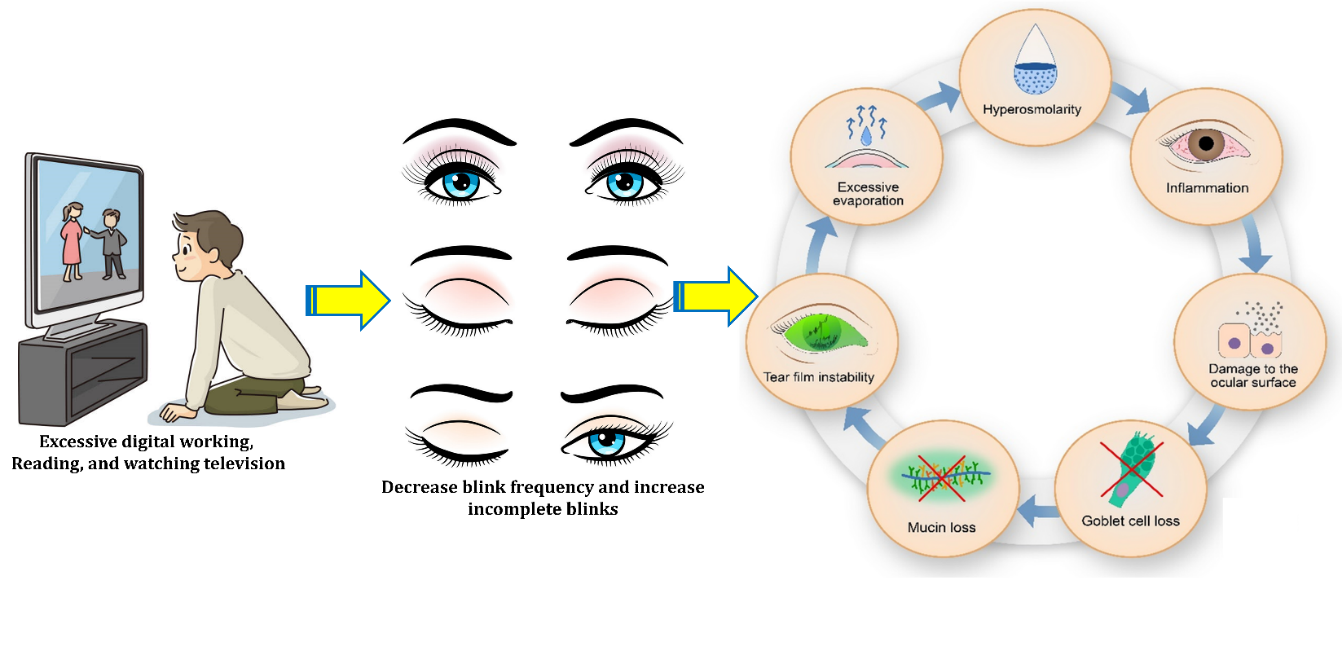
Dry eye disease (DED) stands as a widespread global health issue that impacts people's quality of life, productivity at work, and financial stability significantly. It is identified by either a decrease in tear production, heightened evaporation of tears, or the presence of low-quality tears. These factors collectively contribute to inflammation, damage to the surface of the eye, and unusual perception of pain. The development of DED involving instability in the tear film, increased tear fluid concentration (hyperosmolarity), and inflammation. This cycle tends to sustain itself. Conventional treatments like artificial tear replacements and corticosteroids have proven to be ineffective in addressing this condition. Alongside conventional anti-inflammatory medications, nutrients that possess both anti-inflammatory and antioxidant properties have gained attention as potential DED treatments. Emerging data shows a connection between vitamin deficiencies and a significant DED risk, highlighting the role of vitamins in ocular health. Evidence supports that vitamins may interrupt the vicious cycle of DED pathogenesis and ameliorate inflammation. The review explores the efficacy of vitamins like vitamin A, vitamin D, vitamin C, and vitamin E in mitigating the Complications of DED. The findings suggest that vitamin supplementation holds promise as a complementary approach to managing DED.
Introduction
A complicated ocular surface illness known as dry eye disease (DED) is characterised by the breakdown of the equilibrium of the tear film. This condition ranks among the most prevalent ophthalmic ailments globally, afflicting 10% to 50% of the population.[1] DED is identifiable by a spectrum of uncomfortable ocular symptoms, including blurred vision, ocular discomfort, pain, gritty sensations, redness, and a persistent feeling of foreign objects within the eye. Daily tasks including travelling, working, reading, and seeing television, and even utilising digital gadgets might be severely hampered by these symptoms. As a result, DED has become a serious public health issue that has a negative impact on productivity, quality of life, and places a heavy financial burden on society.[2] The pathogenesis of DED is a multifaceted process, encompassing various factors that disrupting the unstable balance between the eye's surface and tear film.[3] Several key pathways contribute to the development and progression of DED are discussed below.
Tear film instability and hyperosmolarity
The major contributing factor to the pathogenesis of DED is the fragility of the tear film and resulting hyperosmolarity. When tears fail to maintain their stability and become hyperosmotic, the ocular surface becomes compromised. This triggers a cascade of events that promote inflammation and activate the innate immune response, thereby setting the stage for a self-perpetuating cycle of ocular surface inflammation and damage.[4]
Inflammation and ocular damage
Ocular surface damage, often initiated by tear film instability, leads to inflammation. The presence of higher levels of inflammatory cytokines, matrix metalloproteinases (MMPs), and chemokines in the tear film of DED patients has clinical value since they help with DED diagnosis and severity grading.[5]
Immune response
The ocular surface deploys a sophisticated immune response mechanism to shield against environmental challenges. In DED, this immune response can become dysregulated, resulting in the activation of immune cells, differentiation of mature T cells, and secretion of proinflammatory factors that sustain the immune response.[6]
Neurosensory abnormality
An additional contributory factor in the development of DED is neurosensory abnormality. Disruptions in neurosensory function on the ocular surface is major contributing factor in development of the disease.[7]
Tear film composition
The tear film is a complex mixture of water, electrolytes, mucins, proteins, and lipids, all of which play pivotal roles in DED pathogenesis. Tear film change is often caused by corneal desiccation, which weakens mucin anchoring to the ocular surface and causes tear film instability. The corneal surface becomes hydrophobic in the absence of mucins, rejecting the aqueous elements of the tear film. This further destabilizes the tear film, increasing tear evaporation and osmolarity, and thus initiating the characteristic inflammatory cascade observed in DED.[8]
Due to the multifactorial nature of DED pathogenesis, effective therapeutic strategies aim to break the relentless cycle of inflammation on the ocular surface. Anti-inflammatory medications such as corticosteroids, cyclosporine A, lifitegrast, autologous serum, and doxycycline have been used to treat the signs and symptoms of dry eyes.[9] Additionally, therapeutic approaches aimed at enhancing immune response and by regulating the inflammatory processes. Furthermore, current research has shown the crucial function of vitamins in preserving ocular surface homeostasis, highlighting their potential defence against DED. Vitamin B is necessary for maintaining the nerve system on the surface of the eye,[10] while the growth, differentiation, and proliferation of corneal and conjunctival epithelial cells depend on vitamin A. The immune-modulating, anti-inflammatory, and antioxidative properties of vitamin C are crucial for maintaining regular physiological processes, while vitamin E offers anti-oxidative protection to the ocular surface, vitamin D is essential in controlling immunological responses and inflammation on the ocular surface.[11] Research has also shown a link between vitamin deficiencies and a higher risk of DED, indicating that vitamin supplementation may help those with deficiencies reduce their signs and symptoms of dry eyes.
In this comprehensive review, our primary goal is to offer a thorough examination of the potential connection between deficiencies in vitamins and DED. Furthermore, we endeavor to investigate the effectiveness of vitamin supplementation as a feasible therapeutic strategy in addressing this prevalent eye condition.
Vitamin A and DED
Vitamin A encompasses a group of micronutrients abundantly found in our diet. Retinol, a preformed type of vitamin A with the molecular formula C20H30O, is predominantly that are present in items made from animals.[13] Meanwhile, carotenoid precursors, including four terpenes consist total of 40 carbon atoms, are prevalent in plant-based foods and constitute most of the provitamin- A sources. Vitamin A holds a pivotal role in preserving a healthy ocular surface and preventing DED by influencing the proliferation and differentiation of the epithelial cells covering the eye's surface.[14]
The significance of vitamin A in causing the synthesis of eicosanoids in the human cornea and conjunctiva has been established by in vitro investigations. This in turn induces the production of the mucin gene MUC16 by activating genes related to secretory phospholipase A (2) group IIA. The development of MUC16, a hydrophilic, membrane-bound mucin, is influenced by the rise in MUC16. This mucin forms a protective shield on the corneal and conjunctival epithelium, safeguarding it against dryness and preventing keratinization, which is crucial in warding off DED.[15] Recent research shows that vitamin A shows crucial a role in the healing of corneal wounds by reducing cell death and facilitating the regeneration of injured epithelial regions and corneal epithelial cells. Additionally, vitamin A is known to enhance tear production and improve the quality of the tear film, thus aiding in the management of DED.[16] Topical vitamin A prevented ocular surface damage in a rabbit model of glaucoma induced on by protracted glaucoma treatment, showed similar effectiveness to topical cyclosporine in mitigating adverse changes to the ocular surface.[17]
It is important to highlight that vitamin A deficiency poses a significant global public health concern, particularly in regions with poor nutritional access or absorption issues. Long-term vitamin A deficiency particularly in impoverished nations, may result in blindness. Furthermore, the loss of goblet cells brought on by a vitamin A deficit might cause DED, which in turn, results in a deficiency of mucin and corneal epitheliopathy. Over time, severe deficiency may lead to the transformation and keratinization of corneal and conjunctival epithelial cells, potentially resulting in conditions such as keratomalacia or corneal ulceration.[18] Both oral and parenteral systemic administration of vitamin A have been found to be beneficial in improving ocular surface damage and DED. In addition, it has been shown that short-term oral vitamin A intake improves the quality of tears. High-dose systemic vitamin A treatment improved corneal epitheliopathy and enhanced goblet cell density in those with xerophthalmia.[19] Vitamin A supplementation may help treat systemic vitamin insufficiency, which can cause mucin shortage owing to the loss of conjunctival goblet cells. This will enhance goblet cell density and improve mucin levels on the ocular surface.[20]
Topical application of vitamin A has also shown promise in the treatment of DED. Studies have indicated that topical vitamin A may effectively reverse conjunctival keratinization.[21] Moreover, vitamin A ointments have been found to enhance visual acuity, alleviate dry eye symptoms, reduce rose Bengal staining scores, and increase Schirmer scores. Interestingly, vitamin A ointment has even reversed conjunctival squamous metaplasia. When compared to a moisture chamber, vitamin A ointment has demonstrated greater effectiveness in preventing ocular surface damage, particularly in intensive care unit patients. According to research, vitamin A emulsion may improve Schirmer scores and tear break-up time (TBUT), indicating that it may be effective in treating DED.[22] Both vitamin A palmitate and cyclosporine A 0.05% eye drops have been successful in reducing Schirmer scores, TBUT, impaired vision, and goblet cell density in instances of DED brought on by extended use of prostaglandin analogue anti-glaucoma drugs. According to another research, using vitamin A palmitate gel following strabismus surgery promoted the growth of conjunctival goblet cells and enhanced symptoms of dry eye, as well as Schirmer and fluorescein staining scores, TBUT, and fluorescein staining scores. The use of different forms and doses of topical vitamin A in these investigations, however, makes more study necessary to create the ideal topical formulation.[23], [24]
Vitamin A is crucial for visual pigments and ocular surface integrity, and is used to treat various diseases. Dry eye disease can result from vitamin A deficiency, with mild changes causing conjunctival changes and severe ones causing xerophthalmia. A healthy diet can help manage these diseases. Oral vitamin A supplements are more effective than commercially available lubricants for managing eye dryness. Topical vitamin A can regulate corneal epithelial cell proliferation and support tear production. Preservative-free vitamin A drops are more effective than other eye drops. Vitamin A supplementation for two months improves visual acuity and eliminates excessive tearing.[25]
Evidence Linking DED and Vitamin D
Vitamin D comprises a class of fat-soluble secosteroids that are present in limited food sources and can also be naturally synthesized within the skin. Its primary role involves enhancing the absorption of calcium in the digestive tract and maintaining appropriate levels of calcium and phosphate in the bloodstream to support typical bone mineralization and overall bone health. Vitamin D, whether produced internally following exposure to sunlight or acquired through dietary sources and supplements, remains biologically inactive and necessitates two enzymatic hydroxylation processes for activation. At present, the concentration of 25(OH)D in the bloodstream serves as the principal indicator of one's vitamin D status, reflecting the combined contributions from endogenous production and dietary intake through foods and supplements.[26], [27]
Definitive thresholds for serum concentrations indicating a deficiency in 25(OH)D have not been firmly established. However, the Food and Nutrition Board (FNB) of the National Academies of Sciences, Engineering, and Medicine (NASEM) has provided guidance on this matter. According to their recommendations, individuals with serum 25(OH)D levels below 30 nmol/L should be considered at risk of vitamin D deficiency, while those falling within the range of 30 to 50 nmol/L should be cautioned about potential inadequacy.[28] Generally, concentrations exceeding 50 nmol/L are regarded as sufficient for most people. In cases where serum 25(OH)D levels are less than 30 nmol/L, vitamin D deficiency is a concern, and individuals within the 30 to 50 nmol/L range should be alerted to potential inadequacy. The Endocrine Society guidelines advocate an intake of 10,000 IU per day or even higher for specific instances involving malabsorption syndromes.[29]
The Institute of Medicine has recommended a daily vitamin D intake of 4000 IU for individuals in good health. However, this level of intake may prove inadequate when considering the possible non-calcemic functions of vitamin D. Moreover, it may fall short in cases where vitamin D therapy is required due to specific medical conditions. In such pathological situations, the Endocrine Society's guidelines suggest a daily intake of 10,000 IU or potentially higher, particularly when dealing with malabsorption syndromes.[30] Vitamin D deficiency has been linked to a range of medical conditions, including, mental health issues, cancer, type 2 diabetes, musculoskeletal disorders, hypertension, immune disorders, autoimmune disorders, and eye disorders.[31] Consequently, vitamin D may be prescribed to address its deficiency in individuals dealing with these health concerns. Immunohistochemical research has shown the presence of the vitamin D receptor in human eyes, indicating that several types of eye cells can metabolize and activate vitamin D. These results, together with other data, clearly imply that vitamin D participates in the cellular physiology of the eyes and is probably essential for preserving ocular health.[32]
DED is a prevalent global public health concern, impacting not only visual function but also daily life, workplace productivity, and overall patient well-being. The prevalence of DED among individuals aged 40 and older varies widely, ranging from 5% to 50%, with older women being more susceptible to DED-related symptoms.[33] Risk factors for DED encompass advancing age, female gender, specific medications, underlying medical conditions, and environmental influences. Environmental variables include air pollution, exposure to smoking, and dry, windy weather that accelerates the evaporation of tears. Extended screen time, prolonged contact lens use, and refractive eye surgery are all factors that may cause abnormal blinking patterns, which can also contribute to the development of DED. Additionally, the use of several medicines, such as blood pressure medications, decongestants, antihistamines, and antidepressants, is connected to decreased tear production.[34], [35]
Local factors such as eyelid abnormalities, dysfunction of the meibomian glands, blepharitis, and conjunctivochalasis can heighten the risk of developing DED.[36] Additionally, systemic conditions like diabetes mellitus, chronic pain syndrome, rheumatoid arthritis, anxiety, depression, thyroid disorders, irritable bowel syndrome, allergic conditions, and hyperlipidemia have been linked to an increased susceptibility to DED.[37] Recent findings have suggested that vitamin D might have a potential role in influencing both the onset and progression of DED. Considering preclinical data and clinical reports, there is an indication that systemic vitamin D supplementation could be advantageous. After providing a foundational understanding of the underlying mechanisms behind DED, we will further explore and justify the potential use of vitamin D as a therapeutic strategy in managing this condition. Numerous ocular conditions, such as uveitis, retinoblastoma, diabetic retinopathy, age-related macular degeneration, myopia, and dry eye, have been linked to vitamin D insufficiency.[38] Additionally, preclinical studies have shown that several eye cells have the Vitamin D Receptor (VDR) and the enzymes required for vitamin D metabolism, indicating that vitamin D functions as a paracrine/autocrine regulator. According to experimental evidence, after exposure to UV light, corneal and retinal cells may produce vitamin D from exogenous 7-dehydrocholesterol and convert it into its active form.[39] Vitamin D is produced locally in the eye, as shown by the discovery of vitamin D metabolites in tear fluid, aqueous humour, and vitreous humour. Studies on mice have shown that vitamin D has a favourable effect on the corneal epithelium's barrier function while the lack of the VDR gene activity hinders the repair of the corneal epithelium. Additionally, vitamin D functions as a potent modulator of the innate and adaptive immune systems in the eye, inhibiting the migration of Langerhans cells into the cornea, decreasing the overproduction of proinflammatory substances, and reducing inflammation in dry eye models. These actions help to restrain corneal inflammation. However, it's important to note that recent clinical research about the therapeutic application of vitamin D in the pathogenesis of DED has produced a relatively limited number of studies.[40], [41]
Reduced tear break-up time, poorer Schirmer test scores, tear hyperosmolarity, and general tear film dysfunction have all been associated to vitamin D insufficiency as dry eye syndrome signs.[42] According to these results, there may be a link between vitamin D levels and the occurrence of dry eye symptoms. Furthermore, vitamin D blood levels are correlated with tear stability and secretion. Even when exhibiting modest dry eye symptoms, those with lower blood vitamin D levels often have more severe symptoms, which are frequently accompanied by a modified cytokine profile in their tears and increased amounts of proinflammatory molecules. Additionally, genetic evidence linking vitamin D to DED has been found, primarily via single-nucleotide polymorphisms in the VDR genes. Additionally, a case-control research including 70 DED patients and 70 matched controls found a strong correlation between the prevalence of DED and low blood vitamin D concentrations.[43] Furthermore, a comprehensive research of the adult population in Korea found a link between DED and insufficient sun exposure. These data taken together imply that getting enough sun exposure or vitamin D supplementation may be advantageous for those with DED.[44] However, a recent thorough meta-analysis of the information that is now available on the connection between vitamin D and dry eye reiterated the relevance of this correlation. It was shown that persons with DED often had lower blood vitamin D levels than healthy people, and that vitamin D insufficiency was significantly related with an increase in dry eye symptoms.
Vitamin D Supplementation to Manage DED
Vitamin D, available in the forms of ergocalciferol and cholecalciferol, is rapidly and effectively absorbed in the small intestine following oral ingestion. The peak concentration of 25(OH)D is typically achieved within a span of 7 to 14 days, contingent upon the administered dosage.[45] While vitamin D absorption was initially thought to occur solely through passive diffusion, recent research indicates a potential role for membrane carrier proteins, particularly those involved in cholesterol transport. Furthermore, the presence of dietary fat can enhance the absorption of vitamin D.[46] Vitamin D supplementation has been widely suggested as a remedy for DED; however, there is a scarcity of clinical studies assessing its impact. An observational investigation uncovered several favorable outcomes following intramuscular vitamin D administration in individuals with both vitamin D deficiency and DED that did not respond to artificial tear treatment. These benefits encompassed increased tear production, reduced tear instability, diminished inflammation on the ocular surface and eyelid margin, and amelioration of DED symptoms. Notably, vitamin D-deficient patients undergoing systemic vitamin D replacement therapy reported improvements in tear hyperosmolarity.[47]
Another notable study established a connection between low vitamin D levels, dry eye symptoms, and vitamin D supplementation. The introduction of systemic vitamin D supplementation resulted in elevated serum levels, better conditions on the ocular surface, enhanced tear quality, and alleviation of DED symptoms.[48] Furthermore, it was found to augment the effectiveness of topical lubricants containing lipids, such as carbomer-based artificial tears and hyaluronate, in individuals with DED. This suggests that the efficacy of topical lubricants may be contingent upon vitamin D serum concentrations. Overall, these findings indicate that patients grappling with DED may derive benefits from systemic vitamin D administration.[49] Vitamin D deficiency is associated with tear hyperosmolarity and tear film dysfunction, additionally it was demonstrated that patients with vitamin D deficiency developed dry eye and impaired tear function. They reported lower scores in Schirmer test and TBUT, and higher in OSDI scores in patients with vitamin D deficiency than in contro.[50] The recent study shows that Vitamin D replacement improves tear osmolarity in patients with vitamin D deficiency. [51] Vitamin D supplementation as an adjuvant to routine dry eye treatment improves ocular surface hemostasis parameters, results in better tear stability and a more improved tear osmolarity in patients with vitamin D deficiency.[52]
Vitamin B and DED
Vitamin B complexes represent a group of water-soluble vitamins with coenzyme activities that may play a role in maintaining ocular surface stability and preventing DED. Various micronutrients within the vitamin B group have been Linked to DED, specifically neuropathic ocular discomfort (NOP).Vitamin B1 (thiamine) has antioxidant properties and supports carbohydrate metabolism, protein synthesis, and neurotransmitter production53. Vitamin B2 (riboflavin) also possesses antioxidant activity and has shown features that hinder the development of cataracts. While vitamin B12 (cobalamin) promotes nerve regeneration and remyelination, vitamin B6 (pyridoxine) is essential for immune system control and neurotransmitter synthesis. These vitamins may be deficient, which can result in reduced neuron survival and regeneration, peripheral and central sensitization, and neuropathic pain, which can cause symptoms of dry eyes.[53] Chronic nerve injury may contribute to maladaptive neuroplastic alterations in somatosensory pathways and neuropathic pain in DED. This damage is often brought on by ocular surface damage and tear film instability.[54]
Studies have shown that the pathophysiology of DED is significantly influenced by anomalies in the neurosensory system. In 2017, neurosensory abnormalities were included to the Dry Eye Workshop II (DEWS II) criteria of DED. Chronic nerve injury may cause pathologic changes in the peripheral and central neurological systems, including ocular surface damage and tear film instability, which can lead to the development of NOP.[55] In DED patients, discrepancies between dry eye symptoms and signs are typical, and NOP may partially explain this phenomenon. Micronutrient supplementation has showed promise in alleviating DED, particularly NOP-associated DED, and vitamin B insufficiency may affect NOP-associated DED. Experimental studies have suggested that vitamin B12 plays a role in regulating nerve regeneration. Clinical cases have reported dramatic improvements in NOP with parenteral vitamin B12 administration. Vitamin B12 supplementation has been found to enhance ocular surface health, tear secretion, and stability, outperforming conventional treatments in some cases.[14], [56]
Furthermore, vitamin B12 deficiency has been associated with Sjögren syndrome, hinting at other mechanisms linking vitamin B12 and DED. Studies have explored the benefits of oral vitamin B1 and mecobalamin in improving both DED symptoms and signs.[57] Nebulized vitamin B applied to the ocular surface has led to reduced symptoms, improved tear film stability, and enhanced corneal health. Topical application of vitamin B12 and citicoline has been effective in patients with diabetes mellitus and DED, promoting ocular surface recovery and nerve plexus density.[58] Eye drops containing preservative-free hyaluronic acid and vitamin B12 have shown promise in alleviating DED symptoms and reducing oxidative stress.[59] However, more research is needed to evaluate the individual effects of each vitamin in DED management.
Vitamins C and E in Relation to DED
Vitamin C, a water-soluble vitamin represented by the chemical formula C6H8O6, plays a vital role in the prevention of DED owing to its antioxidative, anti-inflammatory, and immunomodulatory functions.[60] The natural composition of the human tear film includes notable amounts of vitamin C, which actively contribute to its inherent ability to safeguard against oxidative stress and inflammation on the eye's surface. Furthermore, the therapeutic potential of vitamin C in the recovery process of corneal injuries has garnered recognition.[61] Recent investigations, employing a rat model, have showcased the effectiveness of vitamin C in reducing corneal swelling and alleviating inflammation subsequent to damage induced by exposure to ultraviolet B radiation. In a similar vein, experiments using a mouse model have revealed that the application of topical vitamin C can ameliorate the infiltration of inflammatory cells within the cornea, foster the proliferation of limbal stem cells, and curtail the formation of new blood vessels in the cornea following alkali burns.[62], [63]
Vitamin E belongs to a group of fat-soluble compounds distinguished by a chromanol ring with a side chain at the C2 position. It is renowned for its antioxidative properties, which play a role in bolstering the eye's antioxidant defenses, potentially aiding in the prevention of DED. Recent experiments employing a rabbit model indicated that both vitamin C and E had comparable effects on the healing of corneal wounds.[64], [65] In individuals diagnosed with diabetes mellitus (DM), oral supplementation with vitamins C (at a daily dose of 1000 mg) and E (at a daily dose of 400 IU) for a span of 10 days resulted in enhancements in tear film stability (measured by TBUT), Schirmer scores, conjunctival goblet cell density, and the reversal of conjunctival squamous metaplasia. These improvements were attributed to a decrease in oxidative surface damage to the eye. The beneficial effects of oral antioxidant supplementation, including vitamins A, C, and E, were further substantiated in a prospective randomised experiment. Improvements were seen on the TBUT, Schirmer scores, corneal fluorescein staining scores, and reactive oxygen species levels in tears.[66], [67], [68]
After cataract surgery, Fogagnolo et al. suggested that topical vitamin E and coenzyme Q10 treatment might successfully stimulate the repair of the corneal subbasal nerve plexus and improve ocular surface stability.[69] Serrano-Morales et al. showed that eye drops containing 0.1% cross-linked hyaluronic acid, coenzyme Q10, and vitamin E exhibited similar efficacy to higher-dose carmellose eye drops in improving tear film stability and reducing symptoms of dry eyes in a study involving menopausal women receiving antidepressant treatment.[70] This raises the possibility of vitamin E's effectiveness. Additionally, topical vitamin E and coenzyme Q10 therapy showed promise in restoring ocular surface balance and enhancing tear film stability, particularly in paediatric patients and those who had been exposed to chlorinated water. In a recent investigation conducted by Li et al., a combination of 3% diquafosol and vitamin E (tocopherol at 0.005% or 0.01%) eye drops outperformed 3% diquafosol eye drops alone in enhancing tear film quality, lipid layer, corneal epithelial health, reducing inflammation on the ocular surface, and increasing conjunctival goblet cell density.[71] These results indicate that vitamin E by itself could potentially have a positive influence on Dry Eye Disease (DED) treatment. It's worth noting that while these studies provide valuable insights, further research is warranted to specifically evaluate the individual contributions of vitamins C and E in the context of DED.
Conclusion
The Studies discussed in this review highlights the potential link between vitamin deficiencies and the onset of DED. These findings emphasize the importance of monitoring vitamin levels in the blood of DED patients, particularly when conventional treatments yield limited results. Although there is a growing body of evidence supporting the effectiveness of vitamin supplementation in managing DED, especially with a focus on vitamins A and D, it is clear that further extensive research is required. This is particularly pertinent to vitamins B, C, and E, where the precise mechanisms of action and their specific influence on different types of DED (such as aqueous deficiency, lipid deficiency, and mucin deficiency) demand further elucidation. Prospective studies involving larger and more diverse populations are indispensable for establishing precise guidelines regarding the timing, composition, dosage, and duration of vitamin supplementation. It is important to note that short-term systemic vitamin administration, usually lasting 28 days or less, seems to carry a low risk of side effects. Nonetheless, the potential risks associated with long-term vitamin A supplementation, including complications like hypercalcemia, osteoporosis, and teratogenicity, as well as the potential for meibomian gland disorders and blepharoconjunctivitis with extended topical vitamin A use, underscore the need for prudent management.
In conclusion, this review underscores the role of vitamin deficiencies in the development of DED and suggests that vitamin supplementation can alleviate dry eye symptoms and contribute to the restoration of a healthy ocular surface. Unfortunately, there is a shortage of clinical studies that have explored the influence of vitamin D on Dry Eye Disease (DED). Consequently, looking ahead, it is essential to plan and conduct suitable studies to delve more deeply into this innovative treatment approach and thoroughly explore the beneficial impact of vitamin D in preserving eye health. However, comprehensive research efforts are essential to fully comprehend the mechanisms underlying the impact of each vitamin on DED and to establish well-defined guidelines for optimal patient care concerning supplementation.
Source of Funding
Not applicable
Conflict of Interest
None.
References
- Craig J, Nelson J, Azar D, Belmonte C, AB. The TFOS Dry Eye Workshop II: Executive Summary. Ocul Surf. 2017;15(4):802-12. [Google Scholar]
- Chao W, Belmonte C, Castillo J, Bron A. Report of the Inaugural Meeting of the TFOS i2 = initiating innovation Series: Targeting the Unmet Need for Dry Eye Treatment. Ocul Surf. 2016;14(2):264-316. [Google Scholar]
- Wei Y, Asbell P. The core mechanism of dry eye disease is inflammation. Eye Contact Lens. 2014;40(4):248-56. [Google Scholar]
- Stahl U, Willcox M, Stapleton F. Osmolality and tear film dynamics. Clin Exp Optom. 2012;95(1):3-11. [Google Scholar]
- Mittag T. Role of oxygen radicals in ocular inflammation and cellular damage. Exp Eye Res. 1984;39(6):759-69. [Google Scholar]
- Wei J, Gronert K. The role of pro-resolving lipid mediators in ocular diseases. Mol Aspects Med. 2017;58:37-43. [Google Scholar]
- Periman L, Perez V, Saban D, Lin M, Neri P. The Immunological Basis of Dry Eye Disease and Current Topical Treatment Options. J Ocul Pharmacol Ther. 2020;36(3):137-46. [Google Scholar]
- Malik A, Claoué C. Transport and interaction of cosmetic product material within the ocular surface: Beauty and the beastly symptoms of toxic tears. Cont Lens Anterior Eye. 2012;35(6):247-59. [Google Scholar]
- Thulasi P, Djalilian A. Update in Current Diagnostics and Therapeutics of Dry Eye Disease. Ophthalmology. 2017;124(11S):27-33. [Google Scholar]
- Kuo C, Huang Y, Lin K, Tsai T. Vitamin d deficiency is associated with severity of dry eye symptoms and primary sjögren’s syndrome: A systematic review and meta-analysis. J Nutr Sci Vitaminol (Tokyo). 2020;66(4):386-8. [Google Scholar]
- Sridhar U, Tripathy K. Commentary: Dry eye syndrome and vitamin D deficiency. Indian J Ophthalmol. 2020;68(6):1026-7. [Google Scholar]
- Gayton J. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 2014;3:405-12. [Google Scholar]
- Aguilera-Méndez A, Boone-Villa D, Nieto-Aguilar R, Villafaña-Rauda S, Molina A, Sobrevilla J. Role of vitamins in the metabolic syndrome and cardiovascular disease. Pflugers Arch. 2022;474(1):117-40. [Google Scholar]
- Pellegrini M, CS, Bernabei F, Cicero A, Vagge A. The role of nutrition and nutritional supplements in ocular surface diseases. Nutrients. 2020;12(4). [Google Scholar]
- Ruiz-Lozano R, Hernandez-Camarena J, Loya-Garcia D, Merayo-Lloves J, Rodriguez-Garcia A. The molecular basis of neurotrophic keratopathy: Diagnostic and therapeutic implications. A review. Ocul Surf. 2021;19:224-40. [Google Scholar]
- Mohan R, Kempuraj D, Souza S, Ghosh A. Corneal stromal repair and regeneration. Prog Retin Eye Res. 2022;91. [Google Scholar]
- Bonniard AA, Yeung J, Chan C, Birt C. Ocular surface toxicity from glaucoma topical medications and associated preservatives such as benzalkonium chloride (BAK). Expert Opin Drug Metab Toxicol. 2016;12(11):1279-89. [Google Scholar]
- Morkeberg J, Edmund C, Prause J, Lanng S, Koch C, Michaelsen K. Ocular findings in cystic fibrosis patients receiving vitamin A supplementation. Graefe’s Arch. Graefes Arch Clin Exp Ophthalmol. 1995;233(11):709-13. [Google Scholar]
- Ratay M, Bellotti E, Gottardi R, Little S. Modern therapeutic approaches for noninfectious ocular diseases involving inflammation. Adv. Healthc Mater. 2017;6(23). [Google Scholar] [Crossref]
- Xiao Y, Paiva C, Yu Z, Souza R, Li D, Pflugfelder S. Goblet cell-produced retinoic acid suppresses CD86 expression and IL-12 production in bone marrow-derived cells. Int Immunol. 2018;30(10):457-70. [Google Scholar]
- Tseng S. Topical tretinoin treatment for severe dry-eye disorders. J Am Acad Dermatol. 1986;15(4 Pt 2):860-6. [Google Scholar]
- Garrigue J, Amrane M, Faure M, Holopainen J, Tong L. Relevance of Lipid-Based Products in the Management of Dry Eye Disease. J Ocul Pharmacol Ther. 2017;33(9):647-61. [Google Scholar]
- Kim E, Choi J, Joo C. A Comparison of Vitamin A and Cyclosporine A 0.05% Eye Drops for Treatment of Dry Eye Syndrome. Am J Ophthalmol. 2009;147(2):206-13. [Google Scholar]
- Kim E, Joo C, Preedy V. Vitamin A with Cyclosporine for Dry Eye Syndrome. Handbook of Nutrition, Diet and the Eye. 2014. [Google Scholar]
- Brandão L, Vilar L, BC, Brandão P, Arantes T, Campos J. Serum levels of vitamin a, visual function and ocular surface after bariatric surgery. Arq Gastroenterol. 2017;54(1):65-9. [Google Scholar]
- Rafeeq H, Ahmad S, Tareen M, Shahzad K, Bashir A, Jabeen R. Biochemistry of Fat Soluble Vitamins, Sources, Biochemical Functions and Toxicity. Haya Saudi J Life Sci. 2020;5:188-6. [Google Scholar]
- Maurya V, Aggarwal M. Factors influencing the absorption of vitamin D in GIT: an overview. J Food Sci Technol. 2017;54(12):3753-65. [Google Scholar]
- Julian C, Lentjes M, Huybrechts I, Luben R, Wareham N, Moreno L. Fracture risk in relation to serum 25-hydroxyvitamin D and physical activity: Results from the epic-norfolk cohort study. PLoS One. 2016;11(10). [Google Scholar]
- Vieth R. Why the minimum desirable serum 25-hydroxyvitamin D level should be 75 nmol/L (30 ng/ml). Best Pract Res Clin Endocrinol Metab. 2011;25(4):681-91. [Google Scholar]
- Holick M, Binkley N, Bischoff-Ferrari H, Gordon C, Hanley D. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 1911;96(7):1911-30. [Google Scholar]
- SW. Non-musculoskeletal benefits of vitamin D. J Steroid Biochem Mol Biol. 2018;175:60-81. [Google Scholar]
- Lv Y, QY, Ma W, Liu H, Ji J, Li X. Associations of Vitamin D deficiency and Vitamin D receptor (Cdx-2, Fok I, Bsm i and Taq I) polymorphisms with the risk of primary open-angle glaucoma. BMC Ophthalmol. 2016;16. [Google Scholar] [Crossref]
- Stapleton F, Alves M, Bunya V, Jalbert I, Lekhanont K, Malet F. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15(3):334-65. [Google Scholar]
- Galor A, Feuer W, Lee D, Florez H, Carter D, Pouyeh B. Prevalence and risk factors of dry eye syndrome in a United States Veterans Affairs population. Am J Ophthalmol. 2011;152(3):377-84. [Google Scholar]
- Tan L, Morgan P, Cai Z, Straughan R. Prevalence of and risk factors for symptomatic dry eye disease in Singapore. Clin Exp Optom. 2015;98(1):45-53. [Google Scholar]
- Starr C, Gupta P, Farid M, Beckman K, Chan C, Yeu E. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019;45(5):669-84. [Google Scholar]
- Gherghel D. More than meets the dry eye: An ocular disease with complex systemic associations. Optician. 2021;2021:8609-1. [Google Scholar] [Crossref]
- Chan H, Zhang X, Ling X, CB, Wang Y, Ip P. Vitamin D and Ocular Diseases: A Systematic Review. Int J Mol Sci. 2022;23(8). [Google Scholar]
- Skowron K, Pawlicka I, Gil K. The role of vitamin D in the pathogenesis of ocular diseases. Folia Med Cracov. 2018;58(2):103-18. [Google Scholar]
- Elizondo RA, Yin Z, Lu X, Watsky M. Effect of vitamin D receptor knockout on Cornea epithelium wound healing and tight junctions. Invest Ophthalmol Vis Sci. 2014;55(8):5245-51. [Google Scholar]
- Reza D, Ying Q, Pedram H. Twenty-five-year panorama of corneal immunology: emerging concepts in the immunopathogenesis of microbial keratitis, peripheral ulcerative keratitis, and corneal transplant rejection. Cornea. 2000;19(5):625-43. [Google Scholar]
- Bron A, AT, Foulks G, Pepose J, Baudouin C, Geerling G. Rethinking dry eye disease: a perspective on clinical implications. Ocul Surf. 2014;12(2 Suppl):1-31. [Google Scholar]
- Meng Y, Lu J, Xing Q, Tao J, Xiao P. Lower serum vitamin D level was associated with risk of dry eye syndrome. Med Sci Monit. 2017;23:2211-6. [Google Scholar]
- Um S, Kim N, Lee H, Song J, Kim H. Spatial epidemiology of dry eye disease: Findings from South Korea. Int J Health Geogr. 2014;13. [Google Scholar]
- Isom K, Andromalos L, Ariagno M, Hartman K, Mogensen K, Stephanides K. Nutrition and metabolic support recommendations for the bariatric patient. Nutr Clin Pract. 2014;29(6):718-39. [Google Scholar]
- Reboul E, Borel P. Proteins involved in uptake, intracellular transport and basolateral secretion of fat-soluble vitamins and carotenoids by mammalian enterocytes. Prog Lipid Res. 2011;50(4):388-402. [Google Scholar]
- Watts P, Sahai A, Kumar P, Shamshad M, Trivedi G, Tyagi L. A prospective study to assess the role of vitamin D individually and in combination with cyclosporine in the treatment of dry eye in patients with deficient serum 25(OH)D levels. Indian J Ophthalmol. 2020;68(6):1020-6. [Google Scholar]
- Fogagnolo P, Cilla S, Alkabes M, Sabella P, Rossetti L. A review of topical and systemic vitamin supplementation in ocular surface diseases. Nutrients. 2021;13(6). [Google Scholar]
- Hwang J, Lee Y, Shin Y. Vitamin D enhances the efficacy of topical artificial tears in patients with dry eye disease. Cornea. 2019;38(3):304-10. [Google Scholar]
- Demirci G. Dry eye assessment in patients with Vitamin D deficiency. Eye Contact Lens. 2016;44:62-65. [Google Scholar]
- Kizilgul M, SK, Ozcelik O, Beysel S, Apaydin M, Ucan B. Vitamin D Replacement Improves Tear Osmolarity in Patients with Vitamin D Deficiency. Semin Ophthalmol. 2018;33(5):589-94. [Google Scholar]
- Najjaran M, Ghanavati SZ, Askari EA, Eslampoor A, Ziaei M. Effect of oral vitamin D supplementation on dry eye disease patients with vitamin D deficiency. Clin Exp Optom. 2023;106(3):257-62. [Google Scholar]
- Carrasco L. . Neurodegenerative Diseases and the Human Microbiota. 2020. [Google Scholar]
- Patel S, Sarantopoulos K, Galor A. Pathways and Mechanisms of Ocular Pain and Photophobia in Dry Eye Disease. Dry Eye Disease. 2022. [Google Scholar]
- Han S, Yang H, Hyon J, Wee W. Association of dry eye disease with psychiatric or neurological disorders in elderly patients. Clin Interv Aging. 2017;12:785-92. [Google Scholar]
- Ozen S, Ozer M, Akdemir M. Vitamin B12 deficiency evaluation and treatment in severe dry eye disease with neuropathic ocular pain. Graefe’s Arch. Graefes Arch Clin Exp Ophthalmol. 2017;255(6):1173-7. [Google Scholar]
- Wegelius O, Fyhrquist F, Adner P. Sjögren's Syndrome Associated with Vitamin B(12) Deficiency. Scand J Rheumatol. 1970;16(1):184-90. [Google Scholar]
- Ren X, Chou Y, Wang Y, Jing D, Chen Y, Li X. The Utility of Oral Vitamin B1 and Mecobalamin to Improve Corneal Nerves in Dry Eye Disease: An In Vivo Confocal Microscopy Study. Nutrients. 2022;14(18). [Google Scholar]
- Hynnekleiv L, Magno M, Vernhardsdottir R, Moschowits E, Tønseth K, Dartt D. Hyaluronic acid in the treatment of dry eye disease. Acta Ophthalmol. 2022;100(8):844-60. [Google Scholar]
- Teleanu R, Chircov C, Grumezescu A, Volceanov A, Teleanu D. Antioxidant therapies for neuroprotection-a review. J Clin Med. 2019;8(10). [Google Scholar]
- Babizhayev M, Yegorov Y. Biomarkers of Oxidative Stress and Cataract. Novel Drug Delivery Therapeutic Strategies Targeting Telomere Reduction and the Expression of Telomerase Activity in the Lens Epithelial Cells with N-Acetylcarnosine Lubricant Eye Drops: Anti-Cataract which Helps to Prevent and Treat Cataracts in the Eyes of Dogs and other Animals. Curr Drug Deliv. 2014;11(1):24-61. [Google Scholar]
- Chen W, Guo J, Guo H, Kong X, Bai J, Long P. Protective Effect of Vitamin C against Infancy Rat Corneal Injury Caused by Acute UVB Irradiation. Biomed Res Int. 2020;2020. [Google Scholar]
- Li M, Chen Z, Liu L, Ma X, Zou J. Topical Vitamin C Promotes the Recovery of Corneal Alkali Burns in Mice. J Ophthalmol. 2021;2021. [Google Scholar]
- Gujral G, Askari S, Ahmad S, Zakir S, Saluja K. Topical vitamin C, vitamin E, and acetylcysteine as corneal wound healing agents: A comparative study. Indian J Ophthalmol. 2020;68(12):2935-39. [Google Scholar]
- Friedrichson T, Kalbach H, Buck P, Kuijk F. Vitamin E in macular and peripheral tissues of the human eye. Curr Eye Res. 1995;14(8):693-701. [Google Scholar]
- Huang J, Yeh P, Hou Y. A randomized, double-blind, placebo-controlled study of oral antioxidant supplement therapy in patients with dry eye syndrome. Clin Ophthalmol. 2016;10:813-20. [Google Scholar]
- Peponis V, Bonovas S, Kapranou A, Peponi E, Filioussi K, Magkou C. Conjunctival and tear film changes after vitamin C and E administration in non-insulin dependent diabetes mellitus. Med Sci Monit. 2004;10(5):CR213-7. [Google Scholar]
- Jones L, Downie L, Korb D, Benitez-Del-Castillo J, Dana R, Deng S. TFOS DEWS II Management and Therapy Report. Ocul Surf. 2017;15(3):575-628. [Google Scholar]
- Fogagnolo P, Sacchi M, Ceresara G, Paderni R, Lapadula P, Orzalesi N. The effects of topical coenzyme Q10 and vitamin e d-α-tocopheryl polyethylene glycol 1000 succinate after cataract surgery: A clinical and in vivo confocal study. Ophthalmologica. 2012;229(1):26-31. [Google Scholar]
- Serrano-Morales J, De-Hita-Cantalejo C, Sánchez-González M, Bautista-Llamas M, Sánchez-González J. Efficacy of 0.1% crosslinked hyaluronic acid, coenzyme Q10 and vitamin E in the management of dry eye disease in menopause patients receiving antidepressants. Eur J Ophthalmol. 2022;32(1):658-63. [Google Scholar]
- Li L, Jin R, Li Y, Yoon H, Yoon H, KY. Effects of eye drops containing a mixture of 3% diquafosol sodium and tocopherol acetate (vitamin E) on the ocular surface of murine dry eye. Cutan Ocul Toxicol. 2021;40(4):350-8. [Google Scholar]
- Abstract
- Introduction
- Tear film instability and hyperosmolarity
- Inflammation and ocular damage
- Immune response
- Neurosensory abnormality
- Tear film composition
- Vitamin A and DED
- Evidence Linking DED and Vitamin D
- Vitamin D Supplementation to Manage DED
- Vitamin B and DED
- Vitamins C and E in Relation to DED
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Kallur S, Suryawanshi A, Kashid S, Gawade A, Papade A, Bhise T, Shendage S. Therapeutic potential of vitamin supplements in dry eye disease: A comprehensive review [Internet]. Indian J Clin Exp Ophthalmol. 2024 [cited 2025 Sep 14];10(1):4-12. Available from: https://doi.org/10.18231/j.ijceo.2024.002
APA
Kallur, S., Suryawanshi, A., Kashid, S., Gawade, A., Papade, A., Bhise, T., Shendage, S. (2024). Therapeutic potential of vitamin supplements in dry eye disease: A comprehensive review. Indian J Clin Exp Ophthalmol, 10(1), 4-12. https://doi.org/10.18231/j.ijceo.2024.002
MLA
Kallur, Santosh, Suryawanshi, Aditya, Kashid, Shruti, Gawade, Aishwarya, Papade, Anushka, Bhise, Tanaya, Shendage, Sujata. "Therapeutic potential of vitamin supplements in dry eye disease: A comprehensive review." Indian J Clin Exp Ophthalmol, vol. 10, no. 1, 2024, pp. 4-12. https://doi.org/10.18231/j.ijceo.2024.002
Chicago
Kallur, S., Suryawanshi, A., Kashid, S., Gawade, A., Papade, A., Bhise, T., Shendage, S.. "Therapeutic potential of vitamin supplements in dry eye disease: A comprehensive review." Indian J Clin Exp Ophthalmol 10, no. 1 (2024): 4-12. https://doi.org/10.18231/j.ijceo.2024.002
