- Visibility 36 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijceo.2021.106
-
CrossMark
- Citation
To measure angle of anterior chamber using Topcon SD-OCT: A new technique
- Author Details:
-
Nida Khan *
-
Prakash Agarwal
-
Saroj Gupta
-
Khalid Khan
Introduction
Gonioscopy is the current reference standard for the assessment of the anterior chamber angle. The technique is semi quantitative and subject to inter- and intraobserver discrepancies. Anterior segment optical coherence tomography (AS-OCT) is a new method of imaging the angle. AS-OCT uses the principle of low-coherence interferometry to assess ocular tissues and may be used to obtain quantitative morphometric information. It has been shown that compared with normal eyes, eyes with occludable angles and with PACG have smaller anterior chamber depth (ACD), thicker lenses, and shorter axial length.[1], [2], [3], [4], [5], [6], [7], [8]
Previously used methods for evaluation of the anterior chamber angle of the eye, such as slit-lamp biomicroscopy, or gonioscopy, are known to be subjective. Ultrasound biomicroscopy (UBM) reportedly allows for a quantitative measurement of the anterior chamber angle.[9], [10], [11], [12] However, due to the fact that UBM is a contact measurement, the utilization of this method is limited to patient screening, and cannot be used for immediate postoperative cases.[13], [14], [15], [16], [17], [18], [19], [20] ASOCT have several advantages over gonioscopy as it is rapid, non-contact (can be used in post operative cases), quantitative, qualitative, no interobserver variability, reproducible, it provide rapid estimation of the various anterior segment parameters, including corneal thickness, anterior chamber depth and also helps in examination of posterior segment parameters and provide its measurement.
Materials and Methods
Material
120 Consecutive patients (240 eyes) presenting to ophthalmology out patient department of tertiary health care center in the central India were enrolled in a cross-sectional study. All patients underwent comprehensive ocular examination with included best corrected visual acuity, slit lamp, dilated fundus examination, gonioscopy, intraocular pressure (IOP) measured by Goldmann applanation tonometer, evaluation of angle (i.e. AOD, TISA, TIA) of anterior chamber with SD-OCT was done. The duration of study was one year six months. The data were analyzed by using SPSS 16.0. This study was approved from the research and ethics committee of the institute. Informed consent was obtained.
Inclusion criteria were age >40 years, patients with written informed consent.
Exclusion criteria were patient with Intumescent, mature and hyper mature cataract, high myopia, glaucoma, ocular trauma, major intra ocular eye disease.
The patients above 40 years of age is taken as angle of anterior chamber gets narrower as the age increases.
Methods of evaluation
Eyes that fulfilled both exclusion and inclusion criteria were selected for analysis. After complete clinical examination details of the patient including age, sex, race (Asian) specific examination modes were selected.
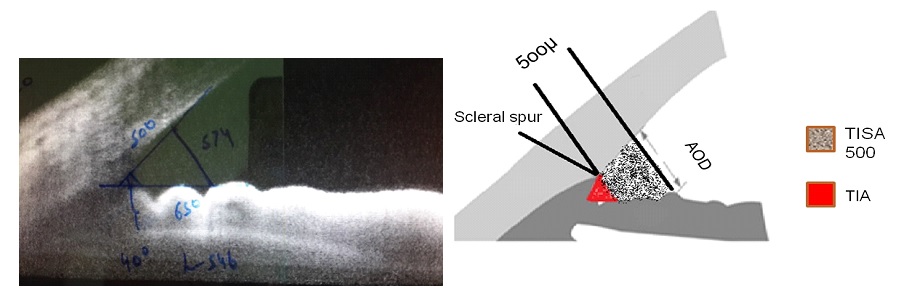
Method of measurement of angle of anterior chamber (AOD, TIA, TISA)
Scleral spur identification is the first step for calculating anterior chamber parameters by OCT. Inbuilt digital calipers of Topcon OCT machine are then used to mark a point on posterior surface of cornea 500 microns anterior to sclera spur. Now a transparent plastic sheet is placed on the computer screen and these 2 points (From scleral spur and posterior surface of cornea i.e. 500 microns) are marked on the sheet. Using digital caliper of Topcon OCT machine a line is drawn perpendicular from posterior corneal point to the surface of iris. This line is AOD 500. A line parallel to AOD500 is drawn from sclera spur to surface of iris. The 2 points on the iris are connected to each other. The quadrilateral (trapezoid) thus formed is called TISA. All these points are marked on the transparent sheet by tracing method. Now the plastic sheet is removed from the screen and using normal scale the lines along cornea and iris and drawn backwards to meet at a point in the angle depth. This defines the apex of anterior chamber angle i.e. TIA. The area of trapezoid (TISA) is measured with the help of applying formula of trapezoid i.e. area = (b1+b2/2)h where b1 height of 1st base b2 is height of 2nd base and h is height of trapezoid.
Results
In our study we have studied the AS-OCT parameters among normal subjects and results of 120 subjects (240 eyes) were analyzed. The mean age of subjects was 53.94 years with a SD ± 8.05 years. There were 61 males and 59 females.
|
Parameter |
Mean nasal |
Mean temporal |
|
AOD µm Male |
0.4583 |
0.4613 |
|
AOD µm Female |
0.4175 |
0.4142 |
|
TISA µm Male |
0.3847 |
0.4569 |
|
TISA µm Female |
0.4258 |
0.4926 |
|
TIA (Deg) Male |
28.2626 |
27.3979 |
|
TIA (Deg) Female |
26.3434 |
25.5054 |
|
Parameter |
Mean Nasal |
Mean Temporal |
|
AOD µm |
0.430 ± 0.137 |
0.433 ± 0.177 |
|
TISA µm |
0.405 ± 0.261 |
0.408 ± 0.278 |
|
TIA (Deg) |
26.904 ± 7.691 |
26.016 ± 7.781 |
|
|
Number of subjects |
Quadrant |
Mean AOD 500µ |
Mean TISA 500µ |
Mean TIA degree |
|
Present study |
120 |
Nasal |
0.43 |
0.40 |
26.90 |
|
Temporal |
0.43 |
0.40 |
26.01 |
||
|
Yuko Maruyama |
130 |
Nasal |
0.42 |
0.16 |
Not done |
|
Temporal |
0.44 |
0.17 |
Not done |
||
|
D S Grewal |
265 |
Nasal |
0.48 |
0.33 |
Not done |
|
Temporal |
0.49 |
0.32 |
Not done |
||
|
Nishant Amer Singh |
239 |
Nasal |
0.27 |
0.11 |
Not done |
|
Temporal |
0.26 |
0.10 |
Not done |
||
|
Sunita Radhakrishnan |
43 |
Nasal |
0.44 |
0.15 |
Not done |
|
Temporal |
0.44 |
0.17 |
Not done |
Discussion
Angle assessment is essential for determining type of glaucoma based on angles. Although gonioscopy has been considered as the gold standard for characterizing the ACA, it is subjective and requires the expertise. Placement of a contact lens on the eye and localized corneal compression can cause fluid displacement and widening of the angle. Light intensity can alter grading of the angle. Imaging with OCT defines ACA characteristics in an objective manner avoiding contact with the globe with contact lens. These images can be analysed qualitatively and quantitatively. As a result, it is a quick, easily tolerated procedure for the patient and there is also less distortion of angle morphology due to lack of globe manipulation.[21]
Yuko Maruyama et al studied an AS-OCT in 130 subjects where they found mean AOD nasal was 0.42 µm and mean AOD temporal was 0.44 µm. While in our study the mean AOD nasal and temporal values are 0.43 µm so, it is showing correlation.[22]
D S Grewal et al. did a study using SD-ASOCT (spectral domain ASOCT) in 265 eyes where the mean AOD nasal was 0.48 µm and AOD temporal was 0.49 µm. While the value of TISA nasal was 0.33 µm and temporal was 0.32 µm.[23] These values are correlating with the values of our study (nasal and temporal AOD 0.43 µm, TISA nasal and temporal 0.40 µm).
Radhakrishnan et al. studied 43 subjects and found mean AOD nasal and temporal was 0.44 µm and mean TISA nasal was 0.15 µm and TISA temporal was 0.17 µm.[24]
Amersingh et al. in their study of 239 subjects they found mean value of AOD nasal was 0.27 µm and temporal was 0.26 µm while mean TISA nasal was 0.11 µm and TISA temporal was 0.10 µm.[25]
In our study the angle measured (in degrees) by gonioscopy correlated with TIA (in degrees) measured by ASOCT. This is comparable with the study of Nolan WP et al. where all patients who have closed angles on gonioscopy also showed closed angles on ASOCT. [26]
Limitation
Small sample size remains the limitation of our study. With more number of patients, a normative value and cut off values for occludable angle can be found out. Also, the scleral spur of superior and inferior quadrants could not be identified in the model of the OCT used in the study.
Conclusion
Anterior segment imaging plays an important role in diagnosis and management of glaucoma. However due to lack of measurement tools(calipers) in OCT machine, in-built software and standard measurement protocols, the parameters such as AOD, TISA and TIA are not discussed in most of these studies. The study proved that the proposed method of measuring AOD,TISA,TIA is the effective method as the Topcon-2000 does not have any inbuilt software like that of other asoctmachines so in such condition it provides a good information for both anterior and posterior segment examination with the help of single machine.
Clinical significance
The study proved that this method of measuring angle of anterior chamber is an effective method of measuring the angles. Anterior segment imaging plays an important role in diagnosis and management of glaucoma. Identification of narrow anterior chamber angle is important for glaucoma screening and prophylactic treatment prevents acute angle closure glaucoma event. So with the help of single machine we can get information of both anterior & posterior segment.
Source of Funding
The authors have no funding or support to disclose for this study.
Conflict of Interest
None.
References
- S Saxena, PK Agrawal, VB Pratap, R Nath. Anterior chamber depth and lens thickness in primary angle closure glaucoma: a case control study. Indian J Ophthalmol 1993. [Google Scholar]
- R Sihota, V Gupta, HC Agrawal, RM Pandey, KK Deepak. Comparison of symptomatic and asymptomatic, chronic, primary angle closure glaucoma, open angle glaucoma and controls. J Glaucoma 2000. [Google Scholar]
- R Sihota, NC Lakshmaiah, HC Agrawal, RM Pandey, JS Titiyal. Ocular parameters in the subgroups of angle closure glaucoma. Clin Exp Ophthalmol 2000. [Google Scholar]
- R Sihota, T Dada, R Gupta, P Lakshminarayan, RM Pandey. Ultrasound biomicroscopy in the subtypes of primary angle closure glaucoma. J Glaucoma 2005. [Google Scholar]
- WC Panek, RE Christensen, DA Lee, DT Fazio, LE Fox, TV Scott. Biometric variables in patients with occludable anterior chamber angles. Am J Ophthalmol 1990. [Google Scholar]
- A Tomilinson, DA Leighton. Ocular dimensions in the heredity of angle closure glaucoma. Br J Ophthalmol 1973. [Google Scholar]
- DA Lee, RF Brubaker, DM Illstrup. Anterior chamber dimensions in patients with narrow angles and angle closure glaucoma. Arch Ophthalmol 1984. [Google Scholar]
- R George, PG Paul, M Baskaran. Ocular biometry in occludable angles and angle closure glaucoma: a population based survey. Br J Ophthalmol 2003. [Google Scholar]
- CJ Pavlin, FS Foster. Ultrasound biomicroscopy. High-frequency ultrasound imaging of the eye at microscopic resolution. Radiol Clin North Am 1998. [Google Scholar]
- LM Sakata, TT Wong, HT Wong. Comparison of Visante and slit-lamp anterior segment optical coherence tomography in imaging the anterior chamber angle. Eye (Lond) 2010. [Google Scholar]
- SF Urbak, JK Pedersen, TT Thorsen. Ultrasound biomicroscopy. II. Intraobserver and interobserver reproducibility of measurements. Acta Ophthalmol Scand 1998. [Google Scholar]
- C Tello, J Liebmann, SD Potash, H Cohen, R Ritch. Measurement of ultrasound biomicroscopy images: intraobserver and interobserver reliability. Invest Ophthalmol Vis Sci 1994. [Google Scholar]
- I Grulkowski, M Gora, M Szkulmowski, I Gorczynska, D Szlag, S Marcos. Anterior segment imaging with Spectral OCT system using a high-speed CMOS camera. Opt Express 2009. [Google Scholar]
- JP Garcia, RB Rosen. Anterior segment imaging: optical coherence tomography versus ultrasound biomicroscopy. Ophthalmic Surg Lasers Imaging 2008. [Google Scholar]
- LM Sakata, R Lavanya, DS Friedman. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology 2008. [Google Scholar]
- T Dada, R Sihota, R Gadia, A Aggarwal, S Mandal, V Gupta. Comparison of anterior segment optical coherence tomography and ultrasound biomicroscopy for assessment of the anterior segment. J Cataract Refract Surg 2007. [Google Scholar]
- CK Leung, H Li, RN Weinreb. Anterior chamber angle measurement with anterior segment optical coherence tomography: a comparison between slit lamp OCT and Visante OCT. Invest Ophthalmol Vis Sci 2008. [Google Scholar]
- MD Bailey, LT Sinnott, DO Mutti. Ciliary body thickness and refractive error in children. Invest Ophthalmol Vis Sci 2008. [Google Scholar]
- M Pekmezci, TC Porco, SC Lin. Anterior segment optical coherence tomography as a screening tool for the assessment of the anterior segment angle. Ophthalmic Surg Lasers Imaging 2009. [Google Scholar]
- WB Khor, LM Sakata, DS Friedman. Evaluation of scanning protocols for imaging the anterior chamber angle with anterior segment-optical coherence tomography. J Glaucoma 2010. [Google Scholar]
- DLK Quek, ME Nongipur, SA Perera, T Aung. Angle imaging: advances and challenges. Indian J Ophthalmol 2011. [Google Scholar]
- Y Maruyama, K Mori, Y Ikeda, M Ueno, S Kinoshita. Morphological analysis of age-related iridocorneal angle changes in normal and glaucomatous cases using anterior segment optical coherence tomography. Clin Ophthalmol 2014. [Google Scholar] [Crossref]
- DS Grewal, GS Brar, R Jain. Comparison of Scheimpflug imaging and spectral domain anterior segment optical coherence tomography for detection of narrow anterior chamber angles. Eye (Lond) 2011. [Google Scholar]
- S Radhakrishnan, J Goldsmith, D Huang, V Westphal, DK Dueker, AM Rollins. Comparison of optical coherence tomography and ultrasound biomicroscopy for detection of narrow anterior chamber angles. Arch Ophthalmol 2005. [Google Scholar]
- N Amerasinghe, PJ Foster, TY Wong, HM Htoon, M He, SY Shen. Variation of angle parameters in asians: an anterior segment optical coherence tomography study in a population of singaporemalays. Invest Ophthalmol Vis Sci 2009. [Google Scholar]
- WP Nolan, JL See, PTK Chew, DS Friedman, SD Smith. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology 2007. [Google Scholar]
