- Visibility 20 Views
- Downloads 1 Downloads
- DOI 10.18231/j.ijceo.2019.106
-
CrossMark
- Citation
A study on intralesional triamcinolone acetonide injection- A non-surgicaltechnique of treatment of chalazion
- Author Details:
-
Gautam Paul
-
Dharmendra Kumar *
-
Tanveer Ahmed
Introduction
Chalazion is a chronic lipogranulomatous, non-infective inflammation of anmeibomian glands. It can affect superior or inferior part of eyelids.[1] It is seen in all age groups and most frequently in females.[2] There is a slight possibility to induce refractive problems among children or blurred vision due to induced astigmatism by pressing on corneal surface and mechanical ptosis if it is too large. It is also associated with cosmetic disfigurement, irritation and rarely conjunctivitis.[1],[3],[4]
Histologically, it was described as epitheloid granuloma, composed of histiocytes, mononuclear granulocytes, lymphocytes, plasma cells, eosinophils.[5]
In initial phase conservative treatment may be tried like antibiotic or corticosteroid eye drops along with warm compression and correction of refractive error. It was reported in other studies that there was 25 to 50% success rate after conservative managements.[5],[6],[7] But higher percent of chalazion reacts to surgical treatment which includes intralesional steroid injection, CO2, laser therapy and incision and curettage of chalazi on with success rate of 60 to 90%.[5],[6],[7]
It is also necessary to rule out malignant lesion such as sebaceous gland carcinoma of eyelid which sometime mimic as chalazion but its incidence is very rare.
Materials and Methods
A prospective study was conducted in the department of Ophthalmology at SMCH, Silchar over a period of one year. The study included 20 patients diagnosed with primary chalazi on. All these patients were undergoing intralesional injection of 4mg (0.2ml) triamcinolone acetonide.
Inclusion criteria
Patients more than 12 years of age, either sex with chalazion of size not less than 6mm.
Exclusion criteria
Infected chalazion with pre -septal cellulitis, recurrent chalaz ion, very small chalazion, patients lower than 1 2 years of age or if the patient was found to have hypersensitivity to local anasthetics. Informed consent was taken prior to the procedure.
Materials
This study included a series of 20 patients selected as per the inclusion criteria. The history of presenting illness was noted. Then the patient was examined under diffuse illumination by torch and by using the slit lamp. Sex and age distribution, lesion recurrence, success rate and the time required for regression was noted. Results are depicted as tables.
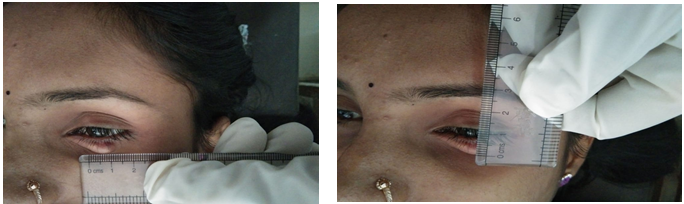
Preoperative examination
Visual acuity testing was done by Snellen's chart. Distant and near vision were noted,intraocular pressure (IOP) was measured using Goldmann applanation tonometry, anterior and posterior segment examination was done to rule out any other pathology, specific examination of the chalazion including size (measure by Castroviejo calliper), its location, duration, extent was noted.
Procedure
Patient was informed about the procedure and informed consent was taken. Topical anaesthesia with proparacaine 0.5 % eye drops were instilled prior to the procedure in the affected eye. 10% betadine was used to thoroughly clean the c halazion site. A twenty-six-gauge (26G) needle over a 1ml syringe was taken into used for injecting 0.2ml of 4 mg of Triamcinolone acetonide (TA) intralesional through transcutaneous into the chalazion. After the administration of the drug, no local antibiotic or eye bandage was given. Patching was also not done after the procedure.
Follow up
All the patients were examined on the first post-operative day, again after 2 weeks and 4 weeks.
Patients who did not respond to intralesional steroid injection were ask to choose between I&C or a second intralesional TA injection. Major outcome measures were the size of the chalazion during every follow-up interval, time required for complete resolution and complications arising due to the procedure. All means were given as mean ± standard deviation.
Results and Observations
| Intralesional triamcinolone injection | ||
| No. of Patients | 20 | |
| No. of chalazion | 20 | |
| Average Age (years) | 27.5 ± 12.08 | |
| Gender | Male | 12 (60%) |
| Female | 8 (40%) | |
| Average Size of chalazion (mm) | 8.52 | |
| Site | Right upper lid | 8 (40%) |
| Right lower lid | 4 (20%) | |
| Left upper lid | 6 (30%) | |
| Left upper lid | 2 (10%) |
From the above table it was noted that, majority of the patients are male as compared to female with average age of 2 7.5 ± 9.63 and average size of chalazion is 8.52mm. Maximum no. of chalazion were noted in RUL (40%) followed by LUL (30%).
| Intralesional triamcinolone injection | |
| Resolution after 14 days post-operative | 14(70%) |
| Resolution after 4th week | 16(80%) |
| Repeat treatment required | 4(20%) |
| Resolution after 14 days on repeat TA injection | 1(25%) |
| Incision and curettage | 3(15%) |
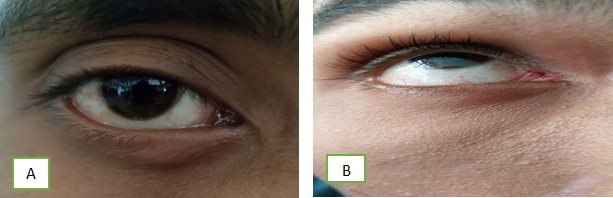
Seventy percent of chalazions completely resolved in 2 weeks after injection and 80 % of chalazions resolved in 4 weeks, whereas 20% of chalazions did not decrease in size by 2 weeks and were given second TA injection after which 25% resolution was achieved (out of 4 patients) post the repeat therapy after 2 weeks. 3 failed cases (15%) required I&C.
Complications
In our study only 1 case develop skin depigmentation due to subcutaneous steroid deposition.


Discussion
Chalazion is one of the most common ocular pathologies which requires surgical correction. Since a long time, the surgical procedure which is being used is tarsal conjunctival incision and curettage of the chalazion. Mostly cases, the above mention treatment modality doesn’t have any complications. Chalazion surgery should not be underestimated and given the same respect like any other ocular surgery.[8] The steroid intralesional injection was first described by Leinfelder et al.,[9] for the treatment of chalazion
In our study we found that intralesional TA injection was an effective and safe treatment alternative for primary chalazions which are not responding to conservative management. Complete resolution of the chalazion was brought about in 8 0 % of the patients after 4 weeks. One injection was sufficient in most cases and only four needed a second injection.[10],[11],[12],[13],[14],[15],[16],[17],[18]
Watson et al., observed that 77 % of chalazions resolved with a 0.22-mg injection of steroid in comparison to 90 % in the I&C group.[13] Many publications have confirmed a similar success rate between intralesional steroid injection (80 – 84%) and I&C (87 – 89%), with a slightly more success rate in the latter.[10],[11],[13],[14] Simon et al.,[15],[16] noted a higher resolution rate with a 4-mg intralesional TA injection (81%) compared to I&C (79%). When it comes to time required for resolution, Pavicic-Astalos et al.,[17] noted that 95 % of chalazions reduced in size by 80% without recurrence after an intralesional TA injection of 4 – 8 mg, with a mean time of 15.27 days, which is similar to our outcome (15.7 ± 10.0 days). About the route of administration, TA injections can also be given subcutaneously, outside the lesion. Ho and Lai found that by using 2-mg subcutaneous TA injection 54.2 % of chalazions resolved completely with single injection and 35.4 % resolved after two injections.[19] In their series, two patients also developed depigmentation over the site of the injection. Also, Chung et al.,[20] reported that 93.8% of chalazions complete resolution with a 3-mg subcutaneous TA injection. Simon GJ et al.,[21] reported that complete resolution was obtained in 33(79%) of 42 patients in the I&C group and in 42(81%) of 52 patients in the TA group.
At many places it is done as a day care procedure on the first visit of the patient. This approach is appropriate as the patients are not prepared for a surgical intervention.
After that many studies have proclaimed the efficacy of intralesional corticosteroid injection and have shown near similar efficacy of both modalities for treatment of chalazion.[9],[16],[17]
Those patients who were treated with intralesional triamcinolone acetonide application (TA) had less er number of visits to ophthalmologists, almost nil requirement of antibiotic therapy and analgesics. Also there is no need of compressive occlusion of the eye unlike patients who undergo classical curettage of chalazion, who have to be given eye occlusion for 24 hours. Though both modalities are equally efficacious, a conclusion can be drawn that each of them has its own field of indication. Steroid therapy is most effective when the chalazion has not been secondarily infected. If secondarily infected, surgical procedure has an upper hand. Triamcinolone injection must be given preference when chalazion is located close to the lacrimal drainage system as surgical damage will be avoided then. The modality of choice when treating chalazion in children and younger patients is triamcinolone acetonide application (TA) as these patients may have a substantial psychological aversion to surgery as opposed to a simple injection.
Surgical treatment (incision & curettage) should be preferred when treating infected lesions, patients not responding to 2 or 3 triamcinolone acetonide (TA) injections, chalazia which are close to the lacrimal drainage system, patients having glaucoma and patients suspected to have adenocarcinomatous lesions where the histopathological verification of resected material is mandatory.
There were no complications while executing any of the two methods of chalazion management. If doing surgical incision and curettage, it is important to follow up the patient to observe scar formation over the site of incision, which can induce irritative symptoms. The major adverse effect of intralesional application of triamcinolone acetonide (TA) is local depigmentation of the skin. If using the conjunctival approach there is minimal risk of penetration of the globe and depigmentation. Ho et al.,18 no ted that two out of 48 patients in whom subcutaneous intralesional triamcinolone acetonide injection was given developed localized skin depigmentation later. In the Gowalla study, none of the 56 patients who were given intralesional triamcinolone injection suffered this adverse effect. In our study, one patient suffered local skin depigmentation. The reason why depigmentation develops may be because a small portion of triamcinolone acetonide (TA) might be deposited by the needle on the way in side or out side the injection site. Another explanation may be that the higher concentration of the drug that was used by us in treatment (40mg/ml), whereas it was lower in Ho’s study (10 mg/mL). The mean time of resolution of the chalazion after one triamcinolone acetonide (TA) injection was two weeks which very well corelates with the study of Simon et al.,[19] Only one patient developed complication due to steroid deposition subcutaneously which lead to skin depigmentation. Simon G J observed that there were no complications like eyelid depigmentation, increased intraocular pressure, or visual loss in either group.
Conclusion
We hereby conclude that intralesional injection of triamcinolone acetonide (TA) has the advantage of being a simple, fast and less painful procedure while treating children, patients having local or systemic hypersensitivity reactions to local anaesthesia and in chalazia located close to the lacrimal drainage system.
The conventional surgery i.e, incision & curettage takes longer time, requires injection of local anaesthesia and may also be associated with increased rate of complications like pain, scarring and hemorrhage. Also, patching of the eye is often required after the procedure.
Source of Funding
None.
Conflict of Interest
None.
References
- A Bagheri, H R Hasani, F Karimian, M Abrishami, S Yazdani. Effect of chalazion excision on refractive error and corneal topography. Eur J Ophthalmol 2009. [Google Scholar]
- A Bagheri, M Tavakoli, H Saloor, M Abrishami, M Aletaha, A Kanani. Epidemiology of eyelid skin masses over a 10-year period at Labbafinejad Medical Center. Bina J Ophthalmol 2013. [Google Scholar]
- . Chalazion treatment. Orbit 2008. [Google Scholar]
- G J Simon, N Rosen, M Rosner, A Spierer. Intralesional triamcinolone acetonide injection versus incision and curettage for primary chalazia: a prospective, randomized study. Am J Ophthalmol 2011. [Google Scholar]
- A A Kothari, A D Sarkar. Chalazion management-surgical treatment versus intralesional injection of long acting steroids. Current Indian Eye Res J Ophthalmic Res Group . [Google Scholar]
- G M Bohigian. Chalazion: A clinical evaluation. Ann Ophthalmol 1979. [Google Scholar]
- H D Perry, R A Serniuk. Conservative treatment of chalazia. Ophthalmol 1980. [Google Scholar]
- L D Pizzarello, F A Jakobiec, A J Hofeldt, M M Podolsky, D N Silvers. Intralesional corticosteroid therapy of chalazia. Am J Ophthalmol 1978. [Google Scholar]
- P J Leinfelder. Depo-Medrol in treatment of acute chalazion. Am J Ophthalmol 1964. [Google Scholar]
- M Y Wong, G S Yau, J W Lee, C Y Yuen. Intralesional triamcinolone acetonide injection for the treatment of primary chalazions. Int Ophthalmol 2014. [Google Scholar]
- J Palva, P E Pohjanpelto. Intralesional corticosteroid injection for the treatment of chalazia. Acta Ophthalmol 1983. [Google Scholar]
- A P Watson, D J Austin. Treatment of chalazions with injection of a steroid suspension. Br J Ophthalmol 1984. [Google Scholar]
- S Ahmad, M A Baig, M A Khan, I U Khan, T A Janjua. Intralesional corticosteroid injection vs surgical treatment of chalazia in pigmented patients. J Coll Physicians Surg-Pak 2006. [Google Scholar]
- S Ahmad, M A Baig, M A Khan, I U Khan, T A Janjua. Intralesional corticosteroid injection vs surgical treatment of chalazia in pigmented patients. J Coll Physicians Surg-Pak 2006. [Google Scholar]
- G J Simon, L Huang, T Nakra, R M Schwarcz, J D Mccann, R A Goldberg. Intralesional triamcinolone acetonide injection for primary and recurrent chalazia: is it really effective?. Ophthalmol 2005. [Google Scholar]
- J Pavii-Astalo, R Ivekovi, T Kneevi, I Krolo, K Novak-Lau, E Tedeschi-Reiner. Intralezijska injekcija triamcinolon acetonida u lijeenju halaziona. Acta Clin Croat 2010. [Google Scholar]
- K Mohan, V Munjal, Jain I. The use of intralesional steroids in the treatment of chalazion. Ann Ophthalmol (Birmingham) 1986. [Google Scholar]
- A W Ormond. Notes on three cases of acquired astigmatism associated with meibomian cysts. Br J Ophthalmol 1921. [Google Scholar]
- S Y Ho, J S Lai. Subcutaneous steroid injection as treatment for chalazion: prospective case series. Hong Kong Med J Xianggang yi xue za zhi 2002. [Google Scholar]
- C F Chung, J S Lai, P S Li. Subcutaneous extralesional triamcinolone acetonide injection versus conservative management in the treatment of chalazion. Hong Kong Med J Xianggang yi xue za zhi 2006. [Google Scholar]
- G J Simon, N Rosen, M Rosner, A Spierer. Intralesional triamcinolone acetonide injection versus incision and curettage for primary chalazia: a prospective, randomized study. Am J Ophthalmol 2011. [Google Scholar]
