- Visibility 133 Views
- Downloads 20 Downloads
- DOI 10.18231/j.ijceo.2020.021
-
CrossMark
- Citation
Relationship of diabetic retinopathy and systemic complications of diabetes
- Author Details:
-
Vishnu Priya N
-
Ramya Deepthi P
-
Kumar Amruth C *
-
P Sowmya
Introduction
Diabetic retinopathy is a microvascular complication affecting the eyes of both type 1 and type 2 diabetes mellitus.[1] Diabetic retinopathy is 4.8% of the 37 million cases of blindness throughout the world,[2] according to the World Health Organisation. India harbors 31.7 million diabetics, and the number is going to rise to an alarming 79.4 million by 2030.[3]
DM is a heterogeneous group of a syndrome in which not only carbohydrate metabolism but metabolism of lipids and proteins are also deranged. The associated metabolic deregulation causes subsequent pathophysiological changes in multiple organ systems, and the risk of complications increases with disease duration.
After 20 years, some grade of retinopathy develops in nearly 99 percent of patients of type 1 and about 60 percent of type 2 diabetes mellitus. Approximately 25 to 40 percent of patients with DM type I, and 20-30 percent of DM type II ultimately develop diabetic nephropathy.[4] About 60-70% of people with diabetes have some form of neuropathy.[5]
Diabetes is also a significant risk factor for cardiovascular disease.[6] Systemic complications of diabetes increases morbidity, as well as the risk of mortality. The presence of diabetic retinopathy indicates the development of these complications, thus putting the ophthalmologist in the front line in detecting these complications for the first time.
Materials and Methods
This study was carried out on 310 patients of diabetes coming to the Department of Ophthalmology. A complete history including the age of onset, duration, treatment for DM, any ocular treatment, and any other systemic illness taken. A complete ophthalmic examination is done.
The severity of DR was determined by fundus biomicroscopy and graded according to the ETDRS classification into five groups. 1. No DR, 2. Mild NPDR, 3. Moderate NPDR, 4. Severe NPDR, and 5. PDR. For the study purpose, the eye with a more severe form of diabetic retinopathy taken into consideration. Nephropathy was diagnosed by the abnormal serum creatinine and presence of microalbuminuria. Diabetic neuropathy was diagnosed clinically by testing for pain, touch, temperature, and vibration sensation as well as eliciting superficial and deep tendon reflexes. The presence of coronary artery disease (CAD) determined by history and previous records, as well as ECG and ECHO. Cerebrovascular disease diagnosed by a history of stroke.
After data compilation, results had statistically analyzed
Results
A total of 310 patients of diabetes mellitus enrolled for the study. The age of the patients ranges 45 to 75 years, with a mean age of 56.5 + 11.8 years with males 211(68.3%) and females 99 (31.70%).

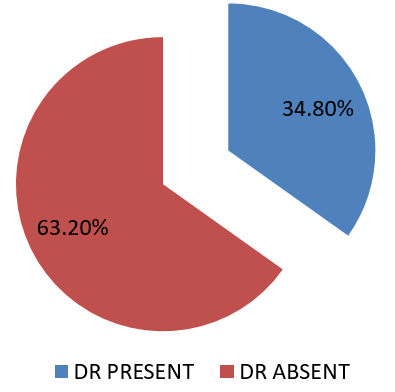
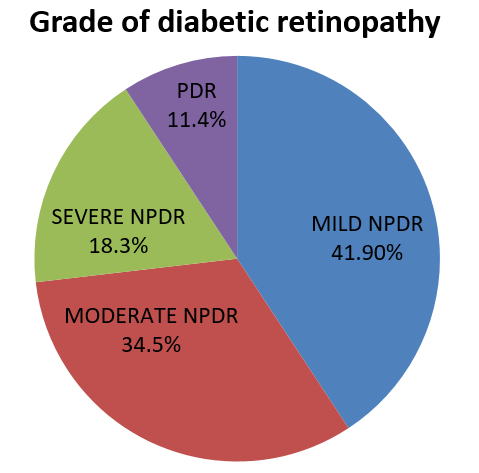
Diabetic retinopathy was present in 108 (34.8%) patients, of which 44 (41.9%) patients had mild NPDR, 35(34.5%) had moderate NPDR, 19(18.3%) had severe NPDR, and 10(11.4%) patients were of PDR.
| Duration of Diabetes | No DR | DR Present | P-value |
| 1-10YRS | 110(91.6%) | 10 (8.3%) | <0.001 |
| 10-20YRS | 86(61.4%) | 54(38.5%) | |
| >20YRS | 6(12%) | 44(88%) |
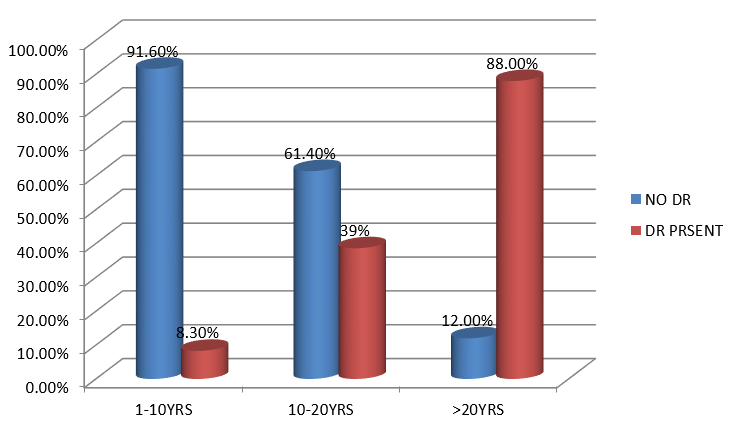
As the duration of diabetes increases, the presence of retinopathy increases significantly.
| Duration of Diabetes | No DR (202) | Mild NPDR (44) | Moderate NPDR(35) | Severe NPDR(19) | PDR(10) | P-value |
| 1-10YRS(120) | 110(91.6%) | 5(4.16%) | 3(2.5%) | 1(0.8%) | 1(0.8%) | <0.001 |
| 10-20YRS(140) | 86(61.4%) | 32(22.8%) | 12(8.5%) | 6(4.2%) | 4(2.8%) | |
| >20YRS(50) | 6(12%) | 7(14%) | 20(40%) | 12(24%) | 5(10%) |
As the duration of diabetes increases the severity of retinopathy increases significantly
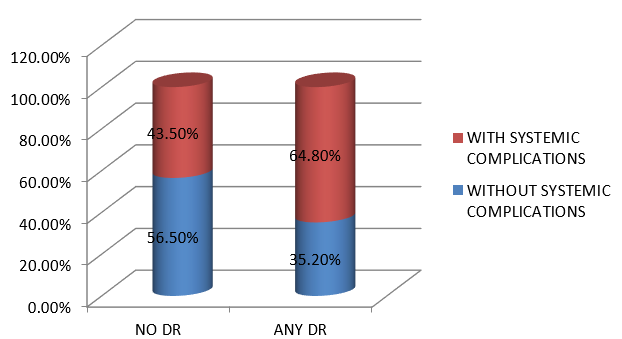
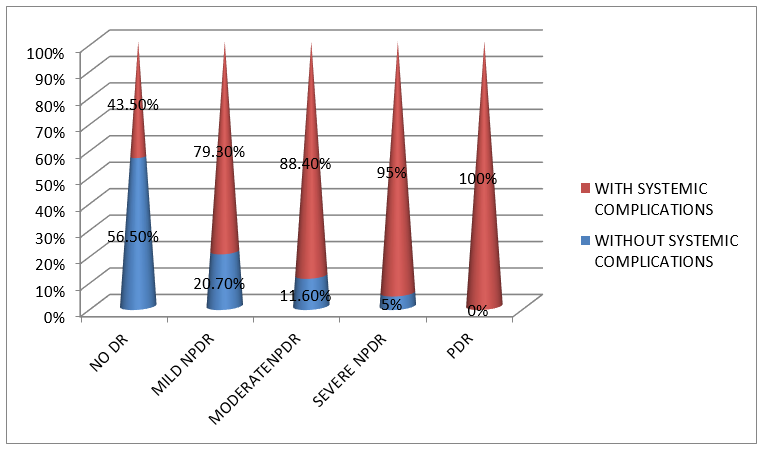
The overall prevalence of systemic complications was 52.6%, and they were significantly (p<0.001) more common in patients with DR (64.8%) as compared to those with no DR (43.5%).
| Diabetic retinopathy | Chronic Kidney Disease (46) | Peripheral Neuropathy (54) | Diabetic Foot (27) | Cerebro Vascular accident (17) | Coronary Artery Disease (23) |
| Present (108) | 25(23.1%) | 30(27.7%) | 14(12.9%) | 10(9.25)% | 15(13.8%) |
| Absent (202) | 21(10.5%) | 24(11.8%) | 13(6.4%) | 7(3.4%) | 7(3.46%) |
| P Value | 0.003 | <0.001 | <0.05 | 0.03 | 0.001 |
PN (27.7%) is the most common systemic complication associated with diabetes followed by CKD (23.1%), CAD (13.8%), DF(12.9%), CVA(9.25%).
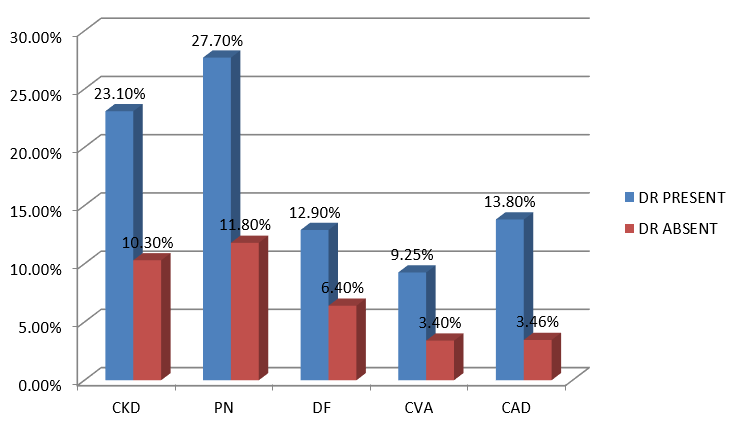
Systemic complications are significantly associated with diabetic retinopathy patients than in patients with no DR.
| Systemic Complications | Mild NPDR 44 | Moderate NPDR 35 | Severe NPDR 19 | PDR 10 | P-Value |
| CKD(46) | 10(22.7%) | 10(28.5%) | 3(15.7%) | 2(20%) | 0.26(NS) |
| PERIPHERAL NEUROPATHY(54) | 9(20.4%) | 10(28.5%) | 7(36.8%) | 4(40%) | 0.68(NS) |
| DF(27) | 5(11.3%) | 2(5.7%) | 3(15.7%) | 2(20%) | 0.72(NS) |
| CVA(17) | 5(11.3%) | 2(5.7%) | 2(10.5%) | 1(10%) | 0.65(NS) |
| CAD(23) | 6(13.6%) | 7(20%) | 1(5.2%) | 1(10%) | 0.39(NS) |
The maximum percentage of patients with systemic complications has seen amongst PDR patients (99.8%), followed by Severe NPDR (95.0%) moderate NPDR (88.40%) and mild NPDR (79.3%).
Discussion
The present study conducted on 310 diabetic patients of diabetes, of whom 108 (34.8%) had diabetic retinopathy of varying severity. According to the present study, DR may appear as early as 1-10 years of having diabetes, and more than 88% of patients develop DR after 20 years of having the disease. With the increasing duration of diabetes, the incidence of DR as well as the severity of retinopathy increases. Association of DR with the duration of diabetes is well known.[7] In the CURES Eye study, 41.8 percent had DR after 15 years of diabetes and severity of DR proportionally increased with longer duration of diabetes.[8]
Evaluating the relationship of diabetic retinopathy with systemic complications of diabetes, we found that out of 108 patients with DR, 64.8 % of patients were affected with systemic complications, while only 43.5 % of patients with no DR had systemic involvement. This was statistic ally significant (p value=0.001).
Diabetic kidney disease is found in 23.1% of patients with DR as compared to 10.30% in patients with no DR. This difference is statistically significant (p-value 0.003). Similar results were documented by Venkatesh P et al[9] and Tajunisah I et al,[10] who showed DR to be positively associated with overt nephropathy.
Peripheral neuropathy was more frequently associated with the patient having DR (27.7%) as compared to patients without DR (11.8%), and this difference was statistically significant (p-value <0.001). Similar results were seen in the study by Venkatesh P et al[9] and Dyck et al[11] where neuropathy was significantly associated with patients of diabetic retinopathy.
The diabetic foot was found in 12.90% of diabetic patients with retinopathy, while in those with no DR, it was seen only in 6.40%, the difference between both being statistically significant (p-value <0.05). A study by Ahmati I et al[12] also reported DR to be a significant risk factor for the development of the diabetic foot. CVA was also found to be significantly (p<0.05) more common in patients with DR (9.25%) than those without DR (3.4 %). Presence of retinopathy is associated with stroke, particularly in persons with associated hypertension as reported by Nakayama et al.[13]
CAD was also more commonly asso ciated with patients of DR (13.8%) than in those with no DR (3.4 6%), the difference being statistically significant as studied by Gadkari SS[14] et al. According to Cheung et al.,[15] 2007e, the presence of retinopathy was associated with a two-fold higher risk of incidnt coronary heart disease and a three-fold higher risk of fatal coronary heart disease.
Analyzing the relationship of these systemic complications with DR we found complications increases with the severity of DR. Studies by Venkatesh P et al,[9] Klein et al.,[16] 1999b reported a significant association of overt nephropathy and neuropathy with the severity of DR. A significant association between CAD and severity of DR was reported by Gerstein HC et al[17] and Cheung et al. Studies by Klein et al., reported PDR was associated with stroke mortality, independent of diabetes duration, glycemic control, and other risk factors in both type 1 and 2 diabetes.
Conclusion
Our observations support that diabetic retinopathy increases the risk of both micro and macrovascular complications of diabetes. Retinopathy may therefore represent vascular damage and injury not only in the eyes but also in other vital organs such as the brain, heart, and kidneys in people with diabetes. However, a thorough search must be done to detect concurrent systemic co-morbidities in all patients of diabetic retinopathy irrespective of the severity, which will surely help in reducing the morbidity and mortality associated with late detection of diabetic end-organ damage.
Conflict of Interest
None.
Source of Funding
No financial interest in study.
References
- Koushiki Mani, Rose C Davy. Prevalence of diabetic retinopathy in type 2 diabetes mellitus patients attending medicine out-patient department of a tertiary care hospital in Alappuzha. Int J Res Med Sci 2017. [Google Scholar]
- S Resnikoff, D Pascolini, D Etya’ale, I Kocur, R Pararajasegaram, G P Pokharel. Global data on visual impairment in the year 2002. Bull World Health Organ 2004. [Google Scholar]
- S Wild, G Roglic, R Sicree, H King. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Dia Care 2004. [Google Scholar]
- Charles M. Clark, D. Anthony Lee. Prevention and Treatment of the Complications of Diabetes Mellitus. N Engl J Med 1995. [Google Scholar]
- A M Aring, D E Jones, J M Falko. Evaluation and prevention of diabetic neuropathy. Am Fam Physician 2005. [Google Scholar]
- W B Kannel, M Hjortland. Castelli WP Role of diabetes in 8. Congestive heart failure: the Framingham study. Amjcardiol 1974. [Google Scholar]
- W Jenchitr. Prevalence of diabetic retinopathy to the duration of diabetes mellitus in community hospitals of Lampang. J Med Assoc Thai 2004. [Google Scholar]
- Rema M. Prevalence of diabetic retinopathy in urban India: the Chennai Urban Rural Epidemiology Study (CURES) eye study, I. Invest Ophthalmol Vis Sci 2005. [Google Scholar]
- P Venkatesh, S Tibrewal, D Bhowmik, M Tripathi, S Ramakrishnan, N Vashist. Prevalence of systemic comorbidities in patients with various grades of diabetic retinopathy. Indian J Med Res 2014. [Google Scholar]
- I Tajunisah, H Nabilah, S C Reddy. Prevalence and Risk Factors for Diabetic Retinopathy A Study of 217 Patients from University of Malaya Medical Centre. Med J Malaysia 2006. [Google Scholar]
- P. J. Dyck, J. L. Davies, D. M. Wilson, F. J. Service, L. J. Melton, P. C. O'Brien. Risk factors for severity of diabetic polyneuropathy: intensive longitudinal assessment of the Rochester Diabetic Neuropathy Study cohort. Diabetes Care 1999. [Google Scholar]
- N Ahmeti, B Laban-Guceva, Jovanovska, Milenkovc, Adamova. Diabetic foot with risk for ulcer formation associated with diabetic retinopathy in type 2 diabetes. Endocrine Abstracts 2011. [Google Scholar]
- Takeo Nakayama, Chigusa Date, Tetsuji Yokoyama, Nobuo Yoshiike, Momoko Yamaguchi, Heizo Tanaka. A 15.5-Year Follow-up Study of Stroke in a Japanese Provincial City. Stroke 1997. [Google Scholar]
- S S Gadkari, Q B Maskati, B K Nayak. Prevalence of diabetic retinopathy in India: The All India Ophthalmological Society Diabetic Retinopathy Eye Screening Study. Indian J Ophthalmol 2014. [Google Scholar]
- N. Cheung, J. J. Wang, R. Klein, D. J. Couper, A. R. Sharrett, T. Y. Wong. Diabetic Retinopathy and the Risk of Coronary Heart Disease: The Atherosclerosis Risk in Communities Study. Diabetes Care 2007. [Google Scholar]
- R. Klein, B. E. Klein, S. E. Moss, K. J. Cruickshanks, P. C. Brazy. The 10-year incidence of renal insufficiency in people with type 1 diabetes. Diabetes Care 1999. [Google Scholar]
- H. C. Gerstein, W. T. Ambrosius, R. Danis, F. Ismail-Beigi, W. Cushman, J. Calles, . Diabetic Retinopathy, Its Progression, and Incident Cardiovascular Events in the ACCORD Trial. Diabetes Care 2013. [Google Scholar]
How to Cite This Article
Vancouver
N VP, P RD, C KA, Sowmya P. Relationship of diabetic retinopathy and systemic complications of diabetes [Internet]. Indian J Clin Exp Ophthalmol. 2020 [cited 2025 Sep 10];6(1):94-98. Available from: https://doi.org/10.18231/j.ijceo.2020.021
APA
N, V. P., P, R. D., C, K. A., Sowmya, P. (2020). Relationship of diabetic retinopathy and systemic complications of diabetes. Indian J Clin Exp Ophthalmol, 6(1), 94-98. https://doi.org/10.18231/j.ijceo.2020.021
MLA
N, Vishnu Priya, P, Ramya Deepthi, C, Kumar Amruth, Sowmya, P. "Relationship of diabetic retinopathy and systemic complications of diabetes." Indian J Clin Exp Ophthalmol, vol. 6, no. 1, 2020, pp. 94-98. https://doi.org/10.18231/j.ijceo.2020.021
Chicago
N, V. P., P, R. D., C, K. A., Sowmya, P.. "Relationship of diabetic retinopathy and systemic complications of diabetes." Indian J Clin Exp Ophthalmol 6, no. 1 (2020): 94-98. https://doi.org/10.18231/j.ijceo.2020.021
