- Visibility 20 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijceo.2021.129
-
CrossMark
- Citation
Profile of ocular injuries amongst various trauma patients presenting to tertiary care centre of Punjab
- Author Details:
-
Arushi Kakkar
-
Anubha Bhatti *
-
Shakeen Singh
Introduction
Ocular trauma is a major but under-recognized cause of disability that has affected younger generation commonly. Approximately, 1.6 million people are blind owing to ocular trauma, 2.3 million are bilaterally visually impaired and 19 million have unilateral visual loss.[1] In India, the reported incidence of ocular trauma varies from 1-5%.[2] Different methods of study of ocular trauma result in geographical and referral bias leading to different conclusions and plenty of misinformation. Data collected from developed countries like U.S.A cannot be applied to developing countries. Analysis of profile of ocular trauma is helpful in identifying the risk factors and planning strategies for the management of ocular injuries.
Material and Methods
This study was conducted for a period of eighteen months in the department of Ophthalmology at SGRD Charitable hospital according to the guidelines of the Declaration of Helsinki and after obtaining approval from ethical committee of Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar. Informed consent was obtained from all individual participants included in the study. All trauma related patients including past history of ocular trauma and those polytrauma patients associated with orbital and ocular injuries were included in the study. Patients in which clinical findings were of non-traumatic origin and with past history of trauma related surgery in the eye were excluded from the study. The patients were informed about the study and a prior written informed consent was taken from all the patients. Detailed history taking was done as per the proforma prepared. Focus was kept on age, sex, occupation, risk factors associated with trauma and location of trauma. Time lag between trauma and presentation to our centre was also documented. Documentation of presenting complaints, type of injury (open globe or closed globe) and extent of ocular involvement (monocular / binocular) was done. Matters of medicolegal concern were also recorded. Detailed ophthalmic work up of all the patients including slit lamp examination, +90D/+78D examination and indirect ophthalmoscopy was carried out. Investigations like B-Scan ultrasonography, CT-scan, MRI with or without contrast, Angiography, VER or any other specific investigation required in any patient was carried out before further management, solely or in collaboration with other speculation. Follow up of these patients was done till their final disposal over 1.5 years.
Results
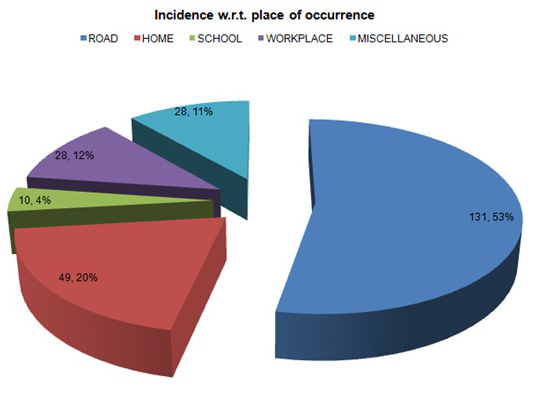
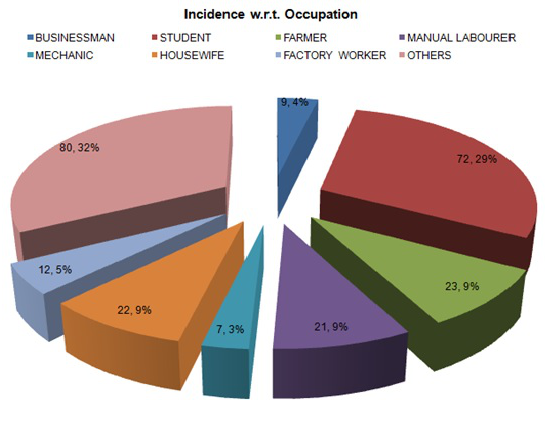
246 patients fulfilled the inclusion criteria. Large proportion of these patients were males (87%). Pediatric age- group comprised 16.7% of the ocular trauma cases. Majority of the patients were from rural background (86.2%). Most of the patients had unilateral ocular involvement, right eye was involved in 102 (41.5%), left eye in 90 (36.6%) and both eyes were involved in 54 (22%) patients. The elapsed time between injury and presentation varied between 1-7 days in 111 (45.1%) patients followed by 4-24 hours in 66(26.8%) patients. ([Table 1]) Incidence with respect to place of occurrence of trauma and with respect to occupation of patients has been shown in [Figure 1], [Figure 2].
|
Variable |
Categories |
Incidence |
|
Location |
Rural |
86.2% |
|
Urban |
13.8% |
|
|
Sex |
Male |
87% |
|
Female |
13% |
|
|
Age |
<15 Years |
16.7% |
|
15-30 Years |
45.9% |
|
|
31-45 Years |
19.1% |
|
|
46-60 Years |
13% |
|
|
61-75 Years |
4.9% |
|
|
Laterality |
Monocular |
78.1% |
|
Binocular |
22% |
|
|
Time of presentation |
<4 hours |
10.6% |
|
4-24 hours |
26.8% |
|
|
1-7 days |
45.1% |
|
|
After 7 days |
17.5% |
|
|
Medicolegal aspect |
Yes |
28.5% |
|
No |
71.5% |
|
|
Alcohol intake |
Yes |
17.1% |
|
No |
82.9% |
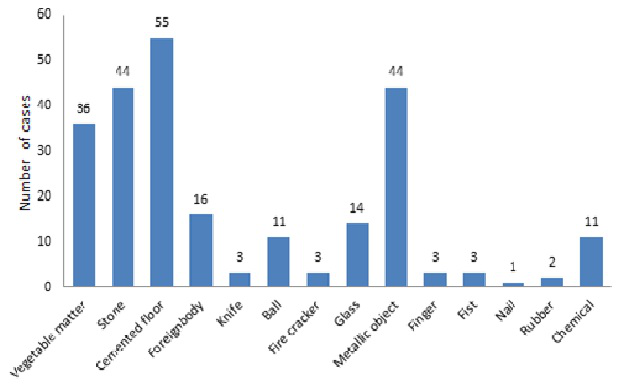
Majority (53.3%) of the patients had trauma on roadside and that too in students. 55 (22.35%) patients had injury on hard (cemented) floor followed by injury with metallic object (17.88%) and stone (17.88%) ([Figure 3]).
Maximum number of ocular injuries in children occurred in the month of January (10 cases) probably due to kite flying around the festival of Lohri while maximum number of ocular injuries in adults occurred in the month of May likely attributed to increased outdoor activities during vacations. Out of the total 235 cases of mechanical injury, closed globe injuries accounted for 209 (88.94%) cases and open globe injuries accounted for 26 cases (11.06%) (Table 2).
|
Open globe |
Closed globe |
||
|
Type of Injury |
Rupture |
4 |
- |
|
Penetrating |
17 |
- |
|
|
Iofb |
1 |
- |
|
|
Perforating |
- |
- |
|
|
Mixed |
4 |
- |
|
|
Contusion |
- |
184 |
|
|
Lamellar laceration |
- |
8 |
|
|
Superficial F.B |
- |
17 |
|
|
Grade (V/A) |
>6/12 |
2 |
155 |
|
>6/60 TO <6/12 |
2 |
28 |
|
|
>1/60 TO <6/60 |
2 |
11 |
|
|
PL TO 1/60 |
15 |
11 |
|
|
NLP |
5 |
4 |
|
|
Zone |
I |
15 |
195 |
|
II |
7 |
11 |
|
|
III |
4 |
3 |
|
|
RAPD |
+VE |
3 |
14 |
|
-VE |
23 |
195 |
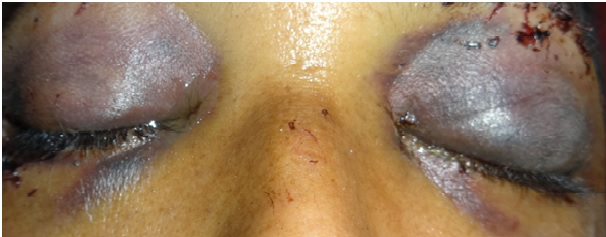
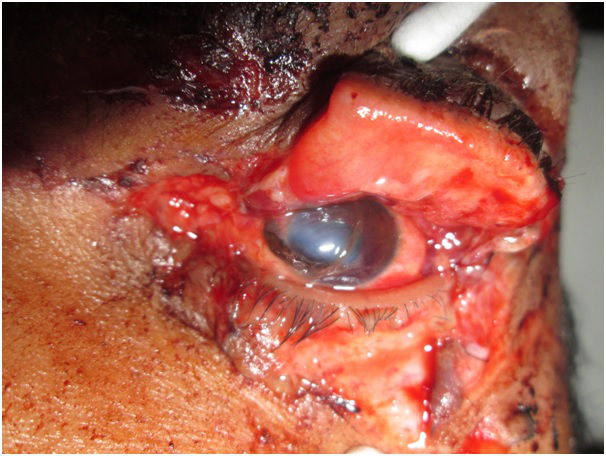
In closed globe injuries, Contusion (184 patients) was the most common presentation and in open globe injuries, penetrating type of injuries (17 patients) was the most common presentation. Conjunctiva was the ocular structure most commonly involved in injury (196 cases) followed by lids (177 cases), orbit (88 cases), cornea (50 cases), anterior chamber (28 cases) and iris (25 cases). Lacrimal apparatus was least involved in ocular injury (2 cases). In our study, lid edema was the most common finding in 154 cases (62.6%) which was followed by lid ecchymosis in 152 patients (61.8%), subconjunctival hemorrhage in 149 patients (60.6%), orbital fracture in 88 patients (35.8%), lid laceration in 47 patients (19.1%), chemosis and hyphaema in 14 patients (5.7%), corneal laceration, sphincter tear and traumatic optic neuropathy in 12 patients (4.9%), epithelial defect in 10 patients (4.1%), scleral laceration and iris prolapse in 7 patients (2.8%) ([Figure 4], [Figure 5], [Figure 6]). [Table 3] outlines the grades of visual loss in whole study population.
|
Grade of visual loss |
Total cases |
Adult cases |
Children cases |
|
NPL |
9 |
9 (100.0%) |
0 (0.00%) |
|
PL To <1/60 |
27 |
21 (77.77%) |
6 (22.22%) |
|
>1/60 To <6/60 |
13 |
11 (84.61%) |
2 (15.38%) |
|
>6/60 To<6/18 |
31 |
27 (87.1%) |
4 (12.90%) |
|
>6/12 |
166 |
137 (82.53%) |
29 (17.46%) |
|
Total |
246 |
205 (83.33%) |
41 (16.66%) |

|
Study |
Year
|
Place |
Duration |
Patients |
Gender |
Laterality |
CG/OG |
Visual Morbidity |
|
Present Study |
2015-2016 |
SGRDIMSR, Amritsar |
18 months |
246 |
M=214 |
R=102 |
CG=88.94% |
49 |
|
F=32 |
L=90 |
OG=11.06% |
||||||
|
B=54 |
||||||||
|
Soliman et al[3] |
2008 |
Kasr El Aini Hospital, CAIRO University |
6 months |
147 |
M=80% |
CG=19.6% |
108 |
|
|
F=20% |
0G=80.4% |
|||||||
|
Omolase et al[4] |
2011 |
Owo, Nigeria |
1 Year |
132 |
M=77.3% |
CG-84.1% |
||
|
F=22.7% |
OG=12.1% |
|||||||
|
Dhasmana et al[5] |
2012 |
Himalyan Institute, Dehradun |
1 Year |
88 |
M=65.9% |
CG=53.39% |
54 |
|
|
F=34.09% |
OG=38.83% |
|||||||
|
Misra et al[6] |
2013 |
Pravara Institute, Loni |
2 Years |
60 |
M=71.7% |
CG=68.33% |
39 |
|
|
OG=31.67% |
||||||||
|
Titiyal et al[7] |
2013 |
Dr. Sushila Tiwari Govt. Hospital, Haldwani |
1 Year |
165 |
M:F= 10:1 |
CG=31.9% |
93 |
|
|
OG=45.5% |
||||||||
|
Gopinath et al[8] |
2015 |
K.R Hospital, Mysore |
1 Year |
60 |
M:F= 3:1 |
CG=66.6% |
15 |
|
|
OG=26.6% |
Discussion
Blindness is a serious public health problem as it affects one’s quality of life. It imposes major socioeconomic and psychological burden on patients and their relatives. Incidence of blindness varies in different communities ranging from 0.2-1 percent (WHO).[9]
The epidemiology of eye injuries varies in different parts of the world and in different age-groups. It depends on many factors including age, sex, profession, life-style, socioeconomic status, traffic behavior, sports and other creative activities. The epidemiology will vary with type of registration and recording of data.[10]
Though literature available on ocular injuries in developed countries is sufficient while data available on ocular injuries from developing countries is limited. The purpose of this study was to make profile of ocular injuries and critically analyze these injuries for better treatment in developing country like India and especially in this northern region.
In our study, majority (86.2%) of the patients were from rural background. Incidence of ocular injuries is less in urban population because of increased awareness amongst them. This rural/urban disparity may be due to urban patients preferring private practitioners which seldom contribute to statistics.
The incidence of ocular trauma was found to be maximum in 15-30 year age group (45.9%), it being the most active period of human life. A gradual decline in incidence was noted after 60 years of age (4.9%). This may be due to sedentary life style adopted by many people in this age-group. The incidence in children (less than 15 years of age) is reported to be 16.7% which may be because children of this age group in this region are more involved in outdoor activities and actively participate in games like bow and arrow and gilli-danda without understanding dangers associated with them. These children are often left to play without protective measures and being supervised by elders.
The latent period between occurrence of injury and reporting to the hospital has an important bearing on the outcome of vision in ocular trauma patients. In developing countries, people generally report late to the hospitals due to many reasons like ignorance, inaccessibility etc. In the present study, 92 (37.4%) cases of ocular trauma reported to the hospital within 24 hours of the occurrence of the injury. Most of these patients were injured in road traffic accidents and many of them were students. Other than this big chunk (45.1%) of the cases reported after 24 hours i.e. between 1-7 days of injury to the hospital. Only amongst them were few patients who reported late and also left the hospital against medical advice. Due to late reporting, chances of complications increase which in turn contribute to increased morbidity and poor visual outcome. Hence, time factor carries an important role in reducing the amplitude of visual morbidity in these ocular trauma patients. The findings in the other studies are different because of many factors like variability in awareness amongst people and accessibility to health care facilities. [Table 4] gives the comparison of our study with other studies.
Visual prognosis in cases of ocular trauma is determined by multitude of factors like latent period between injury and reporting, mode, severity of injury and associated complications.In the present study, complete vision loss was observed in 9 adult cases. 40 cases had vision PL to 6/60 of which 32 were adults and 8 were children. 166 cases had vision more than 6/12 of which 137 were adults and 29 were children. Closed globe injuries were less severe and had better visual outcome than open globe injuries. Visual morbidity in our study was less as compared to other studies. This may be due to more number of benign injuries, prompt referral and close follow up and less industrial injuries (which are usually of severe nature) in our study.
Conclusion
Our study, inspite of having the limitation of short duration of study, gives a good idea of statistics of eye trauma. It will help to design appropriate preventive and therapeutic interventions. The same surveillance system is used to monitor the effectiveness of preventive, acute care and rehabilitative interventions. In a developing country like India, people should be made aware regarding early referral to tertiary care centres to reduce visual morbidity.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
References
- AD Negrel, B Thylefors. The global impact of eye injuries. Ophthalmic Epidemiol 1998. [Google Scholar]
- B Shukla, B Shukla, S Natrajan. Epidemiology of ocular trauma. Management of ocular trauma 2005. [Google Scholar]
- CO Osmolase, EO Omolade, OT Ogunleye, BO Omolase, CO Ihemedu, OA Adeosun. Pattern of ocular injuries in Owo, Nigeria.. J Ophthalmic Vis Res 2011. [Google Scholar]
- GS Gopinath, S Hegde, P Vijaylaxmi, AA Acharya, BK Sudharani. A Study of Clinical Profile and Visual Outcome in Ocular Trauma. Int J Sci Stud 2015. [Google Scholar]
- GS Titiyal, C Prakash, S Gupta, V Joshi. Pattern of Ocular Trauma in Tertiary Care Hospital of Kumaon Region. J Indian Acad Forensic Med 2013. [Google Scholar]
- S Misra, R Nandwani, P Gogri, N Misra. Clinical profile and visual outcome of ocular injuries in a rural area of western India. Australas Med J 2013. [Google Scholar]
- R Dhasmana, H Bahadur, K Jain. Profile of ocular trauma in Uttarakhand. A Hospital Based Study. Indian J Community Health 2012. [Google Scholar]
- MM Soliman, TA Macky. Pattern of ocular trauma in Egypt. Graefes Arch Clin Exp Ophthalmol 2008. [Google Scholar]
- S Resnikoff, D Pascolini, D Etya’ale, I Kocur, R Pararajasegaram, G P Pokharel. Global data on visual impairment in the year 2002. Bull World Health Organ 2004. [Google Scholar]
- HS Al-Mahdi, A Bener, SP Hashim. Clinical pattern of pediatric ocular trauma in fast developing country. Int Emerg Nurs 2011. [Google Scholar]
