- Visibility 24 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijceo.2021.017
-
CrossMark
- Citation
Prevalence and risk factors of allergic conjunctivitis in a semi urban set up
- Author Details:
-
Manikala Sailaja
-
Muduthanpally Charani *
Introduction
Inflammation of the conjunctiva, which is caused due to exposure to allergens is called allergic conjunctivitis.[1], [2], [3] Some allergic conjunctivitis are more common and does not endanger the vision like seasonal allergic conjunctivitis, giant papillary conjunctivitis and perennial allergic conjunctivitis, while some threaten the vision and are less prevalent like atopic keratoconjunctivitis, and vernal keratoconjunctivitis.[4] This type of conjunctivitis is usually Type I atopic hypersensitivity, which is IgE mediated, many times, with the involvement of cell mediated Th2.[5]
Simple allergic conjunctivitis is fairly common and the symptoms are usually underrated and, most of the patients do not go to the hospital for treatment. As a result, it is very difficult to estimate the prevalence of this condition. It is however estimated that about 10-30% of the population are affected by this disorder. In United States around 40% of the people are affected by this disorder.[6], [7], [8]
Allergic conjunctivitis most frequently associated with allergic rhinitis. Other atopic diseases such as dust allergy, food allergy, eczema is also associated with allergic conjunctivitis.[9], [10]
The simple allergic conjunctivitis are acute, seasonal or perinneal. These are IgE mediated and results in the activation of the mast cells by the allergens and subsequent release of active substances like histamine and causing the dilatation of the blood vessels and irritation of nerve endings, resulting in to symptoms.[11] Mechanism of vernal kerato conjunctivitis is not very well understood, but is also said to be because of IgE and also T cell involvement. Atopic kerato conjunctivitis is expected to be due to IgE as well as a delayed hypersensitivity reaction.[12], [13]
The mode of treatment is generally antihistamines, which provide fast relief. There is a wide variation in the occurrence of allergic conjunctivitis in different geographical parts of the world. Therefore, this study was conducted to see the prevalence of allergic conjunctivitis in this part of country.
Materials and Methods
This observational study was conducted in the department of ophthalmology at Mallareddy institute of medical sciences and hospital, Telangana for a period of three years during December 2016 to August 2019. Over 3000 children between the ages 5 to 16 years were surveyed at 3 different schools near our hospital. Out of them 1398 children had various vision problems and were asked to come to the hospital for further treatment. Out of these children, 158 of them were found to have allergic conjunctivitis. The nature of the study was explained to the patents and informed consent was taken from all of them. After clearance from the institutional ethical committee, demographic details were collected from all the patients. The nature and the duration of the conjunctivitis was noted. The socioeconomic status of the child, the nature of the family and its size was also noted.
All children whose parents refused to give consent or whose red eye was diagnosed not to be allergic conjunctivitis were excluded from the study.
Visual acuity was checked for all the patients using Snellen lettered chart as well as the tumbling letter E chart. A slit lamp biomicroscope was used to assess the anterior segment and the posterior segment was assessed using the indirect and the direct ophthalmoscopes. History of redness, itching, photophobia, tears secretion, mucinous secretions were taken down in detail.
Results
Out of the 158 children included in the study, 67 (42.4%) of them were females and 91(57.4%) were males ([Figure 1]).

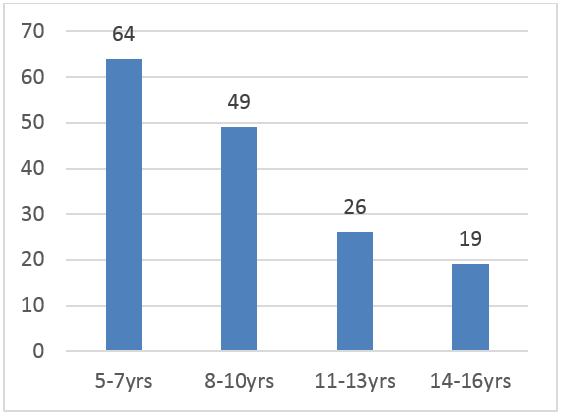
The most common age group which was affected with allergic conjunctivitis was between 5-7 years with 64 children affected (40.5%). 49 children between the ages 8-10 (31%), 26 (16.6%) between 11-13 and, 19 (12%) between 14-16 years were seen to be affected ([Figure 2]).
Most of the children were in their primary school, many of them in the 1st or 2nd standard. 84 (53.2%) were in the primary school, while 59 (37.3%) were in the middle school, or between 6-10th class and 15 (9.5%) were in the 11th or 12 std. Most of them were Hindus, which accounted for 78 (49.4%), 44 (29.8%) were muslims and 30 (19%) were Christians. 4 (2.5%) were Sikhs and 1 was a parsi and 1 was unable to say the religion. 86 (54.4%) were in a nuclear family while 72 (45.6%) were living in a joint family. 76 (48%) had a pet like a dog, a cat or a rabbit at home or in the compound ([Table 1]).
|
Details |
Number |
Percentage |
|
Education: |
|
|
|
Primary |
84 |
53.2% |
|
Middle school |
59 |
37.3% |
|
High school/Secondary school |
15 |
9.5% |
|
Religion: |
|
|
|
Hindu |
78 |
49.4% |
|
Muslim |
44 |
27.8% |
|
Christian |
30 |
19% |
|
Sikh |
4 |
2.5% |
|
Others |
2 |
1.3% |
|
Family lifestyle |
|
|
|
Joint Family |
72 |
45.6% |
|
Nuclear family |
86 |
54.4% |
|
Size of family |
|
|
|
< 4 members |
54 |
34.2% |
|
4-7 members |
59 |
37.3% |
|
8-11 members |
24 |
15.2% |
|
12-15 members |
19 |
12% |
|
>15 members |
2 |
1.3% |
|
Pets |
76 |
48% |
Exposure to dust was the main cause for allergic conjunctivitis as was seen in 51 (32.3%) of the cases. Smoke was the second most common cause with 36 (22.8%) affected, followed by Dry eyes in 22 (13.9%) of the cases19 (12.1%) of the children had AC due to excessive exposure to sunlight and pollen affected 14 (8.9%) of the cases ([Table 2]).
|
Causes |
Number |
Percentage |
|
Sunlight |
19 |
12.1% |
|
Smoke |
36 |
22.8% |
|
Dust |
51 |
32.3% |
|
Dry eye |
22 |
13.9% |
|
Pollen |
14 |
8.9% |
|
Dandruff |
11 |
7% |
|
Bacterial conjunctivitis |
3 |
1.9% |
|
Glaucoma |
1 |
0.6% |
|
Vit A deficiency |
1 |
0.6% |
All the patients experienced itching in the eye, and were rubbing their eyes often. (98.7%). 136 (86.1%) had watery eyes with over lacrimal secretion. Ropy discharge was seen in 13 (8.2%) of the cases and photophobia was experienced by 18 students (11.4%). 28 (17%) of the patients experienced gritty eyes, as if “sand was inside the eye’ ([Table 3]).
|
Itching |
158 |
100% |
|
Rubbing of eye |
157 |
98.7% |
|
Watery eyes |
136 |
86.1% |
|
Redness of eye |
61 |
38.6% |
|
Ropy discharge |
13 |
8.2% |
|
Photophobia |
18 |
11.4% |
|
Grittiness |
28 |
17.7% |
|
Clear mucinous discharge |
11 |
7% |
Majority of the patients with allergic conjunctivitis had allergic rhinitis i.e 129 patients, amounting to 81.6%. 51 (32.3%) had asthma, and 21 (13.3%) had atopic dermatitis ([Table 4]).
|
Allergic comorbidities |
Number |
Percentage |
|
Allergic rhinitis |
129 |
81.6% |
|
Asthma |
51 |
32.3% |
|
Atopic dermatitis |
21 |
13.3% |
Discussion
Allergies are known to affect around 20% of the world’s population. [14], [15] They are often familial. Eyes and nose are the most common sites for the allergens to attack and thus, one of the more common allergic reactions is allergic conjunctivitis. Some of the most common allergens are dust, pollen, mold spores, animal dander etc. this results in redness of the eyes and itchy. Most of the times the AC is mild, so the patients do not seek medical help and it goes unnoticed. Repeated reactions of the allergens cause it to become severe.[15], [16], [17], [18]
The prevalence of AC in a study by Wade et al. was 7.4%, while in the present study it was 5.2%.[19] Another study from Tanzania by Hall et al. reported 35% of the children presenting with AC.[20] In a study in Ghana, a very high prevalence of 40% was observed,[21] and in yet another study, by Abah et al. from Zaire, reported only 7.3% prevalence, similar to our study.[22] In the present study, the predominant gender affected was male, but this was not found to be significant. In the study by Wade et al., females were more in number than males with AC, but like our study, this difference too was not significant.[19] Uchio et al. also reported higher number of females with AC, while another study by Marback et al. reported more males than females.[23], [24]
40.5% of the children in our study belonged to the age group between 5-7 years and 31% were between 8-10 years. 12% of children between 16-14 years were affected. AC is said to occur in children above the age of 3 years and continues till puberty. It then resolves itself in most of the cases.[25]
100% of the patients experienced itching in the eye, and were rubbing their eyes often, while 86% had excessive lacrimation. Ropy discharge was seen in 8.2%, while photophobia was seen in 11.4%. In a survey by Singh and Sinha, itching was the most common symptom corroborating our study. The other symptoms associated with this condition was redness, irritation, water from the eyes.[19]
The most common age group which was affected with allergic conjunctivitis was between 5-7 years with 64 children affected (40.5%). 49 children between the ages 8-10 (31%), 26 (16.6%) between 11-13 and 19 (12%) between 14-16 years were seen to be affected..
Exposure to dust was the main cause for allergic conjunctivitis as was seen in 51 (32.3%) of the cases. Smoke was the second most common cause with 36 (22.8%) affected, followed by dry eyes in 22 (13.9%) of the cases19 (12.1%) of the children had AC due to excessive exposure to sunlight and pollen affected 14 (8.9%) of the cases. A study by Wade et al. reported 60.7% of allergic conjunctivitis in the dry season, the cause being chiefly pollen allergy.[19]
Allergic rhinitis was the most common comorbidity in the present study in more than 80% of the patients, followed by Asthma in 50% of the patients. The other comorbidity that was associated with allergic conjunctivitis was Allergic dermatitis. Rasario et al. reported that most of the children with allergic conjunctivitis had allergic rhinitis, resulting in a lower quality of life.[6] In a study by Singh and Sinha, the prevalence of AC was 30% of the total OPD in Ophthalmology clinics in North India. They found a variation in the season in their study. The said statistics was in the summer months, while in the others, it was far less, of only 10%.[26] A study by Gradman et al. in Denmark reported 42% of Ac to be associated with rhinitis, while 30% had eczema and 24% had asthma.[9] In a study by Malu et al., the most common comorbid condition to be observed was refractive error in 15.4% of the cases. [25].
Conclusion
In many of the cases ocular allergic reaction is overlooked as it is minor discomfort and does not lead to severe infections. As a result, patients do not come to the hospital and seek medical attention. Only when the symptoms become more severe, do they approach a doctor.
The best way to communicate to the people the importance of a regular eye checkup, is health education by the professionals working in the community. This would create an awareness among the people, so that they would take a timely action in treatment.
Source of Funding
None.
Conflict of Interest
None.
References
- L Bielory, MH Friedlaender. Allergic Conjunctivitis. Immunol Allergy Clin North Am 2008. [Google Scholar] [Crossref]
- SJ Ono, MB Abelson. Allergic conjunctivitis: Update on pathophysiology and prospects for future treatment. J Allergy Clin Immunol 2005. [Google Scholar] [Crossref]
- BZ Ortega, MAR Vargas, FMI Tsuchiya, BER Navarro, JJLS Monge. Allergic conjunctivitis in children. Rev Alerg Mex 2007. [Google Scholar]
- M La Rosa, E Lionetti, M Reibaldi, A Russo, A Longo, S Leonardi. Allergic conjunctivitis: a comprehensive review of the literature. Ital J Pediatr 2013. [Google Scholar] [Crossref]
- RP Maurya, VP Singh, MK Singh, P Bhushan, JK Mishra. . Ocular Allergy: An Overview Written in Book: “Update on Respiratory Disease & Allergy . [Google Scholar]
- N Rosario, L Bielory. Epidemiology of allergic conjunctivitis. Curr Opin Allergy Clin Immunol 2011. [Google Scholar] [Crossref]
- K Singh, S Axelrod, L Bielory. The epidemiology of ocular and nasal allergy in the United States, 1988-1994. J Allergy Clin Immunol 2010. [Google Scholar] [Crossref]
- G Brozek, J Lawson, D Szumilas, J Zejda. Increasing prevalence of asthma, respiratory symptoms, and allergic diseases: Four repeated surveys from 1993-2014. Respir Med 2015. [Google Scholar] [Crossref]
- J Gradman, OD Wolthers. Allergic conjunctivitis in children with asthma, rhinitis and eczema in a secondary outpatient clinic. Pediatr Allergy Immunol 2006. [Google Scholar] [Crossref]
- TFB Whitehorn, JM Spergel. The link between allergies and eosinophilic esophagitis: implications for management strategies. Expert Rev Clin Immunol 2010. [Google Scholar] [Crossref]
- L Bielory, MH Friedlaender. Allergic Conjunctivitis. Immunol Allergy Clin North Am 2008. [Google Scholar] [Crossref]
- G Jordakieva, EJ Jarolim. The impact of allergen exposure and specific immunotherapy on circulating blood cells in allergic rhinitis. World Allergy Organ J 2018. [Google Scholar] [Crossref]
- A Li, S Li, F Ruan, Y Jie. Atopic keratoconjunctivitis. Medicine 2018. [Google Scholar] [Crossref]
- B Hesselmar, B Aberg, B Eriksson, N Aberg. Allergic rhinoconjunctivitis, eczema, and sensitization in two areas with differing climates. Pediatr Allergy Immunol 2001. [Google Scholar]
- R Nathan, E Meltze, J Selner, W Storms. Prevalence of allergic rhinitis in the United States. Curr Opin Allergy Clin Immunol 1997. [Google Scholar] [Crossref]
- R Baig, AW Ali, T Ali, A Ali, MN Shah, A Sarfaraz. Prevalence of allergic conjunctivitis in school children of Karachi. J Pak Med Assoc 2010. [Google Scholar]
- J Biswas, I Saha, D Das, S Bandyopadhyay, B Ray, G Biswas. Ocular morbidity among children at a tertiary eye care hospital in Kolkata, West Bengal. Indian J Public Health 2012. [Google Scholar] [Crossref]
- JP Singla, Y Parashar. Prevalence of allergic rhinitis, allergic conjunctivitis and atopic dermatitis in children with recurrent wheeze. Indian Pediatr 2009. [Google Scholar]
- PD Wade, AN Iwuora, L Lopez, MA Muhammad. Allergic conjunctivitis at sheikh zayed regional eye care center, gambia. J Ophthalmic Vis Res 2012. [Google Scholar]
- A Hall, B Shilio. Vernal keratoconjunctivitis. Community Eye Health J 2005. [Google Scholar]
- I Baba. The red eye-first aid at the primary level. Community Eye Health J 2005. [Google Scholar]
- ER Abah, KK Oladigbolu, E Samaila, A Gani-Ikilama. Ocular disorders in children in Zaria children′s school. Niger J Clin Pract 2011. [Google Scholar] [Crossref]
- E Uchio, R Kimura, H Migita, M Kozawa, K Kadonosono. Demographic aspects of allergic ocular diseases and evaluation of new criteria for clinical assessment of ocular allergy. Graefes Arch Clin Exp Ophthalmol 2008. [Google Scholar] [Crossref]
- PMF Marback, D de Freitas, AP Junior, AP Junior, RB Junior. Epidemiology and clinical features of allergic conjunctivitis in a reference center. Arq Bras Oftalmol 2007. [Google Scholar]
- KN Malu. Allergic conjunctivitis in Jos-Nigeria. Niger Med Jo 2014. [Google Scholar] [Crossref]
- M Singh, BP Sinha. Allergic Conjunctivitits: a practice pattern survey from North India. Indian J Appl Res 2019. [Google Scholar]
