- Visibility 224 Views
- Downloads 40 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2020.138
-
CrossMark
- Citation
Acetazolamide assisted rapid resolution of optic disc pit maculopathy in a 15 year old child
- Author Details:
-
Ruchir Amit Mehta *
-
Neha Raka Mehta
-
Samip Mehta
-
Amit Mehta
Abstract
A 15 years old girl presented to us with diminution of vision within 4 days of onset. The child underwent relevant investigations and a diagnosis of optic disc pit maculopathy (OPD-M) was made. The parents refused surgical intervention and so we started the child on oral acetazolamide. She was kept under repeated and close follow-ups. We noticed rapid resolution of optic disc pit maculopathy within 2 months of presentation with complete visual recovery. Oral acetazolamide was tapered during the course of 2 months. We conclude that although numerous treatment modalities have been described for optic disc pit maculopathy, a trial of oral acetazolamide can be offered in cases of optic disc pit maculopathy in paediatric patients.
Introduction
Optic disc pit is a rare congenital anomaly resulting from an imperfect closure of the superior edge of the embryonic fissure that can be congenital or acquired.[1], [2] The incidence of optic disc pit has been reported to be about 1 in 11,000, being bilateral in 15% of the cases.[3] Optic disc pits may be asymptomatic, but they may also present with macula related complications such as serous retinal detachment or cystoid macular edema affecting visual acuity in nearly 50% of the cases.[4] Various treatment alternatives have been described for optic disc pit related maculopathy including conservative management, laser photocoagulation, macular buckling surgery, vitrectomy with or without internal limiting membrane (ILM) peeling, gas tamponade and the combination of them. Acetazolamide therapy has been studied in treatment of optic disc pit maculopathy, with variable success.[5] Herein, we report a rare case of rapid resolution of optic disc pit maculopathy and complete visual recovery in a 15 years old girl who was started on oral acetazolamide within 4 days of visual impairment.
Case History
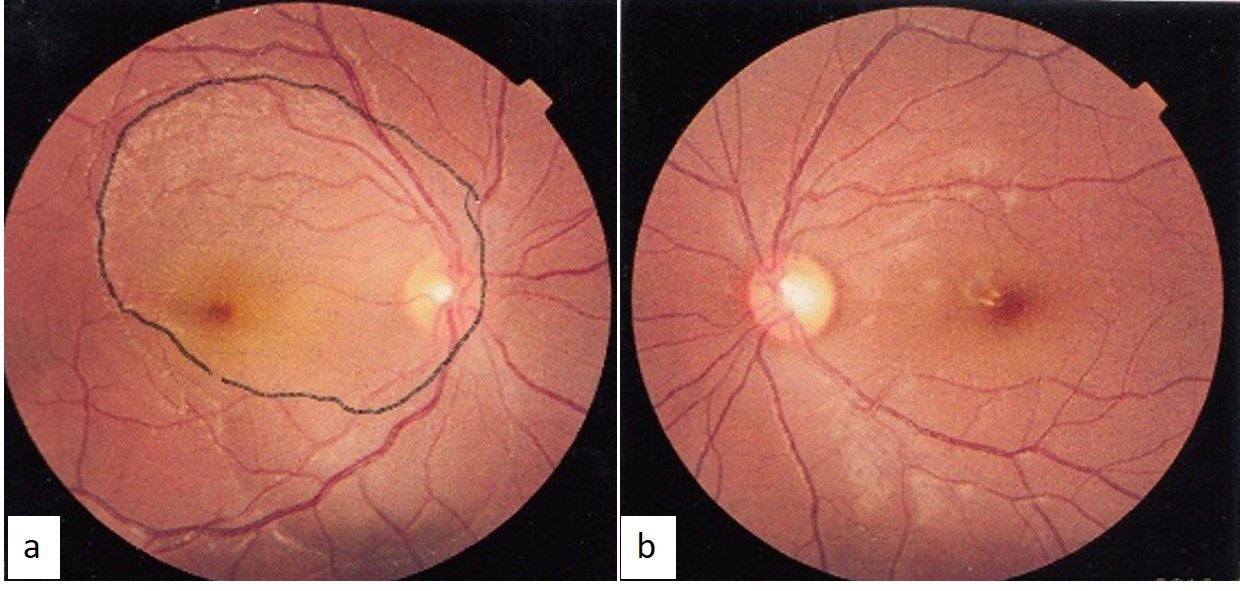
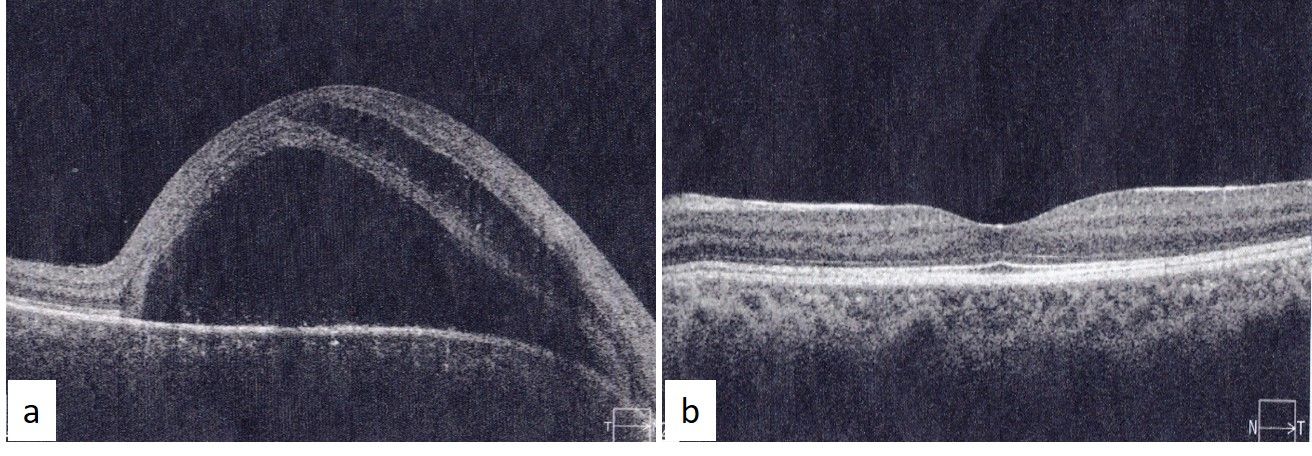
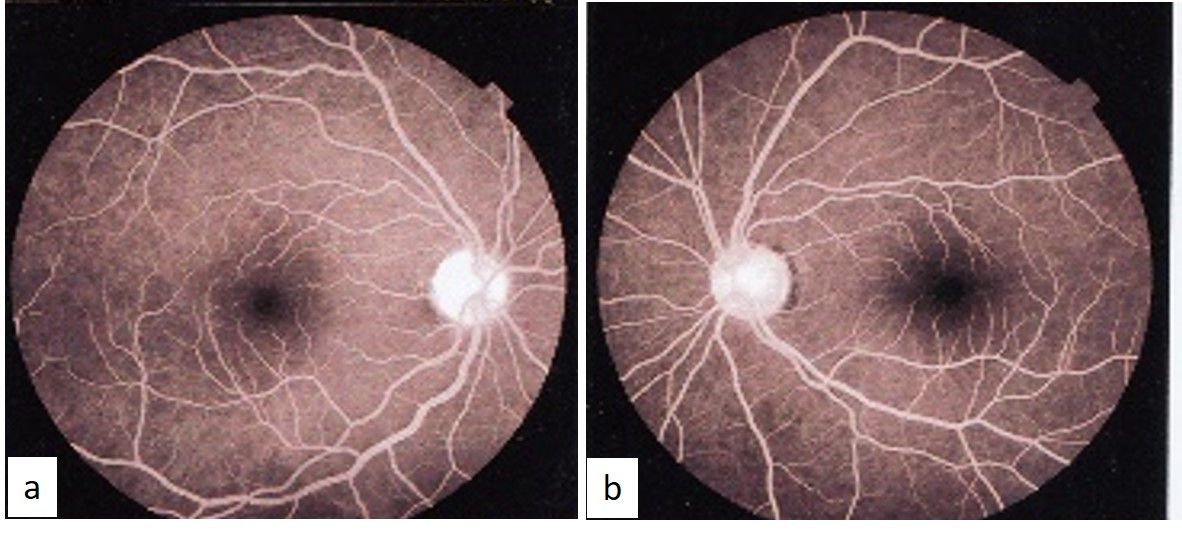
A previously healthy 15-year-old girl, weighing 40 kg, came to us with complaint of sudden painless decrease in vision in right eye since 4 days. The patient had undergone fundus photography, spectral domain optical coherence tomography (SD - OCT) and fundus fluorescein angiography elsewhere. Her best-corrected visual acuity (BCVA) was 20/400, <N36 in the right eye and 20/20, N6 in the left eye. Her intraocular pressures were 13 mmHg in both eyes. Her anterior segment examination was unremarkable. On fundus examination, serous macular detachments extending to the optic disc were noted in right eye but disc pit could not be localized. There were no pathological changes in left eye ([Figure 1] a, b). SD-OCT (Cirrus, Carl Zeiss Meditec. Inc.) imaging revealed macular schisis with neurosensory detachment extending to optic nerve in right eye ([Figure 2] a, b). The FFA images showed no abnormal findings ([Figure 3] a, b). The diagnosis of optic disc pit maculopathy (ODP-M) was made for right eye.
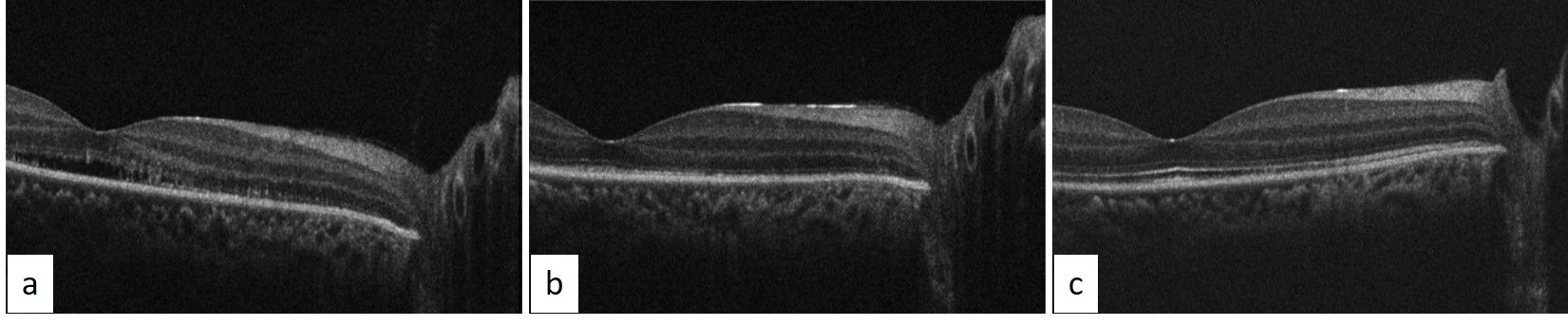
As the parents refused any laser/surgical intervention, patient was started on oral acetazolamide 250 mg three times a day, after ruling out all contraindications, under guarded visual prognosis. The patient was reviewed after 2 weeks, she was symptomatically better with BCVA in right eye improved to 20/120. SD-OCT of the right eye showed minimal subfoveal subretinal fluid, with resolution of macular schisis but complete loss of photoreceptor layers till the optic disc ([Figure 4] a). On further follow-up after 2 weeks, the patient’s visual acuity had improved to 20/40.
SD-OCT at this follow-up showed regenerated external limiting membrane (ELM) but absent ellipsoid zone (EZ) and interdigitation zone (IZ) nasally ([Figure 4] b). Finally, visual acuity of the right eye was 20/20 at 2 months after presentation and initiation of treatment. Fundus examination of the right eye showed good foveal reflex with flat retina and no posterior vitreous detachment (PVD). SD-OCT showed complete resolution of subretinal fluid with complete regeneration of ELM, EZ and IZ within 2 months of presentation ([Figure 4] c). 250 mg oral acetazolamide was tapered to twice daily at 1 month, once daily at 1 ½ months and eventually stopped once there was complete resolution of the maculopathy at 2 months post presentation. The patient maintained her vision and fundal findings on her last visit 12 months from presentation.
Discussion
The source of submacular fluid in OPD-M is controversial and has been suggested to arise from cerebrospinal fluid or liquefied vitreous entering the submacular space through a communication either between the subarachnoid space and the optic pit or through a fenestration in the membrane overlying the pit. There are a few cases reported in literature of spontaneous resolution of maculopathy due to optic disc pit in children[6], [7] and adults,[1], [8], [9], [10] 25% of ODP-Ms do resolve spontaneously, but mostly these result in poor visual outcome, especially if subretinal fluid persists for more than 3 months.[2] As the disease mechanism is still not understood, the management strategy remains debatable. Various treatment alternatives have been described for ODP-M including conservative management, laser photocoagulation, macular buckling surgery, vitrectomy +/- internal limiting membrane (ILM) peeling, gas tamponade and the combination of them. It has been suggested that PVD releases the traction on the fenestration overlying the disc pit and can lead to resolution of ODP-M but there was no PVD in our case at any point. Acetazolamide therapy has been studied in optic disc pit maculopathy as a standalone treatment or an adjuvant therapy with variable success.[5]
Pradeep S Prasad and colleagues[5] first reported use of oral acetazolamide as a standalone therapy for resolution of ODP-M in a 9-year-old child with Incontinentia Pigmenti. They noted complete resolution of ODP-M with a visual outcome of 20/25 after 13 months of oral therapy. Carbonic anhydrase inhibitors (CAIs) improve retinal adhesion and induce resorption of subretinal fluid by producing acidification of the subretinal space.[11] In addition, acetazolamide also inhibits the carbonic anhydrase enzyme in the choroid plexus, resulting in decreased cerebrospinal fluid production and reduction in intracranial pressure.[12] Assuming the fluid in ODP-M originates from the pressure gradient between the subarachnoid space and the eye, lowering the ICP using CAIs could decrease the fluid accumulation in the macular region. Furthermore, acetazolamide also decreases IOP, which might affect the pressure gradient at the lamina cribrosa. The dosage of 250 mg thrice daily for our patient was decided based on US-FDA approved maximum dosage of 1000 mg/ day (10-30 mg/ kg/ day) of oral acetazolamide for children. We also referred to previous reports of use of oral acetazolamide in paediatric patients and the dosage used for those patients.[5], [13], [14] Prasad et al. used 125 mg of oral acetazolamide for 13 months in their 9 years old patient. Osigian et al. and Martins D. et al. have each reported a single case of adjuvant therapy with oral acetazolamide post vitrectomy in case of ODP-M. [13], [14] Osigian et al. placed their 86 kg 12 years old patient on 500 mg of extended-release acetazolamide tablets three times a day. Although duration of acetazolamide therapy was not clearly reported in their study. Considering the speed of improvement in our patient it seems less likely to be a case of spontaneous resolution and more of acetazolamide assisted one. It is noteworthy that the patient has stayed symptom free, off acetazolamide therapy, for 12 months.
Despite numerous case reports offering different treatment modalities, the best method has not yet been determined for paediatric cases with OPD-M. Low-dose oral acetazolamide should be considered in the management of OPD-M, given the rapid and sustained results demonstrated in this case and the potentially decreased risk compared with other treatment strategies, especially in paediatric patients.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Vedantham V, Ramasamy K. Spontaneous improvement of serous maculopathy associated with congenital optic disc pit: an OCT study. Eye. 2005;19(5):596-9. [Google Scholar] [Crossref]
- Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefe's Arch Clin Exp Ophthalmol. 2011;249(8):1113-22. [Google Scholar] [Crossref]
- Kranenburg EW. Crater-Like Holes in the Optic Disc and Central Serous Retinopathy. Arch Ophthalmol. 1960;64(6):912-24. [Google Scholar] [Crossref]
- Gass JDM. Serous detachment of the macula secondary to optic disc pits. Am J Ophthalmol. 1969;67(6):821-41. [Google Scholar]
- Prasad PS, Shah SP, Reddy S, Hubschman JP. Resolution of serous maculopathy associated with optic disk pits and incontinentiapigmenti using oral acetazolamide. Retinal Cases Brief Rep. 2011;5(3):267-9. [Google Scholar] [Crossref]
- Yuen CHW, Kaye SB. Spontaneous resolution of serous maculopathy associated with optic disc pit in a child: A case report. J Am Assoc Pediatr Ophthalmol Strabismus. 2002;6(5):330-1. [Google Scholar] [Crossref]
- Polunina AA, Todorova MG, Palmowski-Wolfe AM. Function and morphology in macular retinoschisis associated with optic disc pit in a child before and after its spontaneous resolution. Documenta Ophthalmol. 2012;124(2):149-55. [Google Scholar] [Crossref]
- Sugar HS. Congenital pits in the optic disc and their equivalents (congenital colobomas and coloboma like excavations) associated with submacular fluid. Am J Ophthalmol. 1967;63:298-307. [Google Scholar]
- Patton N, Aslam SA, Aylward GW. Visual improvement after long-standing central serous macular detachment associated with an optic disc pit. Graefe's Arch Clin Exp Ophthalmol. 2008;246(8):1083-5. [Google Scholar] [Crossref]
- Cruzado-Sánchez DR, Valdivieso HL, Nájar SML. Spontaneous resolution of macular detachment associated with congenital anomalies of the optic nerve: Coloboma and optic disc pit. Arch Soc Esp Oftalmol. 2013;88(5):201-3. [Google Scholar] [Crossref]
- Lashay AR, Rahimi A, Chams H, Davatchi F, Shahram F, Hatmi ZN. Evaluation of the effect of acetazolamide on cystoid macular oedema in patients with Behcet's disease. Eye. 2003;17(6):762-6. [Google Scholar] [Crossref]
- Celebisoy N, Gokcay F, Sirin H, Akyurekli O. Treatment of idiopathic intracranial hypertension: topiramate vs acetazolamide, an open-label study. Acta Neurol Scand. 2007;116:322-7. [Google Scholar]
- Osigian CJ, Gologorsky D, Cavuoto KM, Berrocal A, Villegas VM. Oral acetazolamide as a medical adjuvant to retinal surgery in optic disc pit maculopathy in a pediatric patient. Am J Ophthalmol Case Rep. 2020;17. [Google Scholar] [Crossref]
- Martins D, Bacalhau C, Santos MF. Etiology and treatment of serous macular detachment associated with optic pit - clinical case. . 2012. [Google Scholar]
How to Cite This Article
Vancouver
Mehta RA, Mehta NR, Mehta S, Mehta A. Acetazolamide assisted rapid resolution of optic disc pit maculopathy in a 15 year old child [Internet]. Indian J Clin Exp Ophthalmol. 2020 [cited 2025 Oct 12];6(4):650-653. Available from: https://doi.org/10.18231/j.ijceo.2020.138
APA
Mehta, R. A., Mehta, N. R., Mehta, S., Mehta, A. (2020). Acetazolamide assisted rapid resolution of optic disc pit maculopathy in a 15 year old child. Indian J Clin Exp Ophthalmol, 6(4), 650-653. https://doi.org/10.18231/j.ijceo.2020.138
MLA
Mehta, Ruchir Amit, Mehta, Neha Raka, Mehta, Samip, Mehta, Amit. "Acetazolamide assisted rapid resolution of optic disc pit maculopathy in a 15 year old child." Indian J Clin Exp Ophthalmol, vol. 6, no. 4, 2020, pp. 650-653. https://doi.org/10.18231/j.ijceo.2020.138
Chicago
Mehta, R. A., Mehta, N. R., Mehta, S., Mehta, A.. "Acetazolamide assisted rapid resolution of optic disc pit maculopathy in a 15 year old child." Indian J Clin Exp Ophthalmol 6, no. 4 (2020): 650-653. https://doi.org/10.18231/j.ijceo.2020.138
