- Visibility 323 Views
- Downloads 17 Downloads
- DOI 10.18231/j.ijceo.2020.129
-
CrossMark
- Citation
Effectiveness of patching and non-patching in treatment of corneal abrasion: A comparative study
- Author Details:
-
Baby Deka
-
Saura Kamal Dutta *
-
Shibashis Deb
-
Harish Goswani
-
Tanveer Ahmed
Introduction
Corneal abrasion is a scratch to the outer surface of the most transparent part of eye ball: the cornea. Most of the cases are due to minor trauma to the eye like finger nail injury, by a small foreign body when it is rubbed under a closed eye lid. It also occurs after removal of small metallic foreign body like iron particles in grinding workers. It can occur by a small branch of tree among farmers or by a animal tail injury in people related to diary farming. Corneal abrasions can be caused by the use of hard and soft contact lenses, it occurs when they are being removed after keeping them in-situ for a long duration of time.
More over in conditions of severe dry eye the cornea becomes excessively brittle and there occurs superficial corneal aberration on eye movements. Corneal aberration are common and recurrent in lattice dystrophy of cornea. In emergency we can also find patients with a history of trauma by insect while travelling by a bike and on fluorescent staining a corneal abrasion is detected.
The cornea is richly supplied by sensory nerves whose endings ramify in the epithelium.[1] A corneal epithelial defect produces immediate pain, tearing, photophobia, and foreign body sensation that often motivates the patient to seek medical attention. Approximately 10% of the visits to eye emergency unit[2] are having corneal epithelial defects & generally heal within 2 to 3 days without any long-term complications.
Corneal epithelium is a self-renewing tissue and providing a life-long supply of proliferating cells for epithelial regeneration is the stem cell niche residing in the corneoscleral junction (Di Girolamo, 2015; West et al., 2015). Various pathological physical, and chemical insults cause the disruption of its barrier function and wound formation the corneal epithelium. To preserve corneal transparency and vision proper wound healing needs to be dynamic in order to maintain the integrity and health of corneal epithelial surface. The healing of corneal epithelial wounds has various stages like cell migration, proliferation, adhesion and differentiation with cell layer stratification. It involves extracellular matrix (ECM) and growth factor/cytokine signal-mediated interactions at the wound site to re-establish epithelial integrity and restore homeostasis. The kinetics of epithelial wound healing has two distinct phases: latent phase and closure phase. The latent phase includes cellular and subcellular reorganization to trigger migration of the epithelial cells at the wound edge (Kuwabara et al., 1976; Crosson et al., 1986). The closure phase includes cell migration, which is independent of cell mitosis (Anderson, 1977), followed by cell proliferation and differentiation and followed by stratification to restore the original multicellular epithelial layer (Crosson et al., 1986).
Cytokines and growth factors are important regulators that stimulate growth, proliferation, ECM deposition, proteinase regulation, migration, differentiation, and adhesion of cells involved in wound healing. They also mediate different cell functions including intercellular and intracellular signaling molecules. Corneal cells express cytokines and growth factors that have specific effects on epithelial cells, such as platelet-derived (PDGF), epidermal growth factor (EGF), acidic (FGF-1) and basic (FGF-2) fibroblast growth factors and transforming (TGF) growth factors α and β, keratinocyte (KGF), hepatocyte (HGF) growth factors, insulin-like (IGF-I), interleukins (IL)-1, -6, and -10, thymosin-β4,(Tβ4), and tumor necrosis factor (TNF)-α. All of these factors are activated during wound healing (Lu et al., 2001; Yu et al., 2010b).
Another wound healing factor is the release of matrix metalloproteinases (MMPs), which triggers a series of processes to disengage cell-cell and cell-matrix adhesion leading to cell migration via cross-talk with integrins and the production of ECM proteins in the wound area that act as a temporary scaffold for migratory cells (Tuft et al., 1993). Corneal epithelium makes its own ECM that is apposed to underlying collagenous Bowman’s layer and provides structural support and regulates through various receptors for epithelial proliferation, differentiation, adhesion migration, and apoptosis (Kurpakus et al., 1992; Zieske et al., 1994Azar et al., 1992;)
The sensory nerve fibers of cornea that originate and derived from the ophthalmic branch of the trigeminal ganglion terminate in numerous fine endings among the epithelial cells. The integrity of these nerve fibers is crucial for normal corneal function by sensing stimuli leading to the release of essential neurotrophins, substance P contained in nerve terminals (Gallar et al., 1990) for corneal homeostasis and wound healing (Göbbels et al., 1989).
Wounded epithelial cells of corneal secret the cytokine, IL-1α, which can cause increased immune infiltration of the cornea leading to neovascularization, which may result in visual loss. However, IL-1RN (IL-1α antagonist), prevents leucocyte invasion of the cornea and suppresses neovascularization (Stapleton et al., 2008). In response to wounded epithelium, platelets accumulate in the limbus and migrate to the stroma which is necessary for efficient re-epithelialization through cell adhesion molecules such as P-selectin (Li et al., 2006b; Lam et al., 2011)
The basal limbal epithelial cells are a diverse population with a small number of Limbal Epithelial Stem cells (LESC) predominantly located in the palisades of Vogt (Goldberg and Bron, 1982), and/or in the deeper stromal limbal crypts connected to the limbal epithelium (Dua et al., 2005). Limbal Epithelial Stem cells have a lifetime capacity for self-renewal, and are thought to migrate into the central cornea, proliferate rapidly afterwards and differentiate into central corneal epithelial cells. This process takes place during corneal homeostasis and wound healing.
Epithelial wound healing is mediated by various cytokines and growth factors that activate both sequential and parallel downstream signaling pathways. The evidence suggests the existence of intracellular signaling cross-talk in the epithelial healing after injury. For initiating cell migration, the first step of the healing process, in the initial phase of wound healing several signaling pathways, which cross-talk, are activated to reorganize cellular and subcellular structures. These initial factors include EGF and PDGF (Tuominen et al., 2001), IL-1 and TNF-α (Wilson et al., 1999), which trigger a series of responses leading to epithelial cell migration.
There are several treatment options for corneal abrasions, including pressure patching, bandage contact lenses, and porcine collagen shields. Double patching, in which both the injured and non-injured eyes are patched, has been shown to produce more rapid healing, presumably by decreasing ocular movement.[3], [4] Unfortunately, double patching is infeasible, because it renders the patient unable to perform daily activities without assistance. Porcine collagen shields and bandage contact lenses have been effective in the treatment of corneal abrasions, but both modalities are expensive and require treatment and close follow-up by an ophthalmologist to prevent serious complications. The use of a pressure patch in treatment of corneal abrasions is not accepted by all, because it removes binocular vision, can be uncomfortable for the patient, and may retard healing.[5] Many studies have questioned the effectiveness of patching corneal abrasions in recent past.[3], [5], [6]
Aims and Objectives
The aim was to compare the effectiveness of patching and non-patching in the treatment of non-infected, non-contact lens related traumatic corneal abrasions, as well as of abrasions following foreign body removal.
Materials and Methods
Study design
A prospective, controlled, randomized study on 100 patients presenting with ocular pain following a history of trauma or foreign body removal & corneal abrasion was found on fluorescein stain.
Patients were randomized:
Control group {with patch}: :(receiving an eye patch with topical antibiotics and
Study group {without patch}: :(topical antibiotics with no eye patch
Inclusion criteria
All patients visiting department of ophthalmology, Silchar Medical College & Hospital with traumatic corneal abrasion or removal of superficial corneal foreign body in < 36 hours duration.
The patients with informed consent were enrolled with following criteria:2 c. No history of previous eye trauma or disease in the affected eye;d. No other signs of ocular trauma;e. Simple epithelial defect without stromal edema, or infiltrate andf. No earlier treatment being entered into the study
Exclusion criteria
Any patients who did not fulfill the criteria mentioned in inclusion criteria and patients who used contact lenses were excluded from the study regardless of the cause of the corneal abrasion
Method of data collection
The patients were enrolled after fulfilling the criteria and a complete examination and ophthalmic history including the cause of the abrasion and the time of presentation were noted.
In addition, careful examination of the fellow (non injured) eye was performed to ensure the absence of any preexisting corneal diseases that would exclude the patient from the study.
After fluorescein drops were administered to the eye, the stained corneal abrasion was measured horizontally and vertically to the nearest 0.5 mm by Slit lamp examination (Haag- Streit-900).
Patients were then randomly assigned to one of two treatment groups.
|
Patch group |
No patch group |
|
Mydriatic drops (cyclopentolate 1%), |
Mydriatic drops (cyclopentolate 1%), |
|
Tobramycin eye ointment |
Tobramycin eye ointment |
|
Moxifloxacin eye drops (0.5%) |
Moxifloxacin eye drops (0.5%) |
|
Pressure patch applied to the injured eye. |
No pressure patch applied to the injured eye. |
The pressure patch used in our study consisted of a sandwich of cotton in between two gauge pieces above and below placed over the closed eyelids. To ensure proper placement, patients were asked if they could blink if the patient could be able to blink beneath the patch, it was reapplied with increased pressure until no eyelid movement was possible. The patients were instructed to leave the pressure patch in place for 24 hours. In addition, the patients were instructed how to take care of the patch, including not getting the patch wet, leaving the patch on for 24 hours continuously & not wearing the patch after it has been taken off by the patient.
Patients were daily followed up about photophobia, watering, foreign body sensation, and blurry vision. They were also questioned about their level of pain, which was assessed on a scale of 0-10.
The corneal abrasion was considered healed when:
The patient reported a score of < 2 or
When only minor, nonconfluent, superficial punctate staining of the corneal epithelium remained after fluorescein stain.
Patients were followed until the corneal abrasion was considered healed either subjectively or objectively.
All the data was put on MS Office and statistical analysis was carried out using MS Excel.
Results
Hundred patients were enrolled in the study among them 70 were males and 30 were females. The mean age for all study participants was 32 years (range, 18-60 years). The corneal abrasions were 50 the right eye and 50 in left eye that is its spread equally among presenting eyes [Table 2] shows the most common causes of the corneal abrasions.
|
Cause |
% of total |
|
Foreign body removal |
40 |
|
Fingernail injury |
40 |
|
Pencils injury |
2 |
|
Miscellaneous |
4 |
|
Unknown |
4 |
|
|
No patch group |
Patch group |
|
No. of patients |
50 |
50 |
|
Time before presentation average (hrs)* |
10 |
10 |
|
Size of corneal abrasion in average mm2 |
4.4 |
4.6 |
|
Injured eye pain scale on presentation average (0-10) * |
5.5 |
5.6 |
|
|
No Patch group |
Patch group |
P value |
|
Pain (scale 1-10) |
|||
|
Presentation |
5.5 |
5.6 |
|
|
Day 1 |
1.9 |
2.8 |
0.000176563 |
|
Day 2 |
1.0 |
1.8 |
0.0000000003 |
|
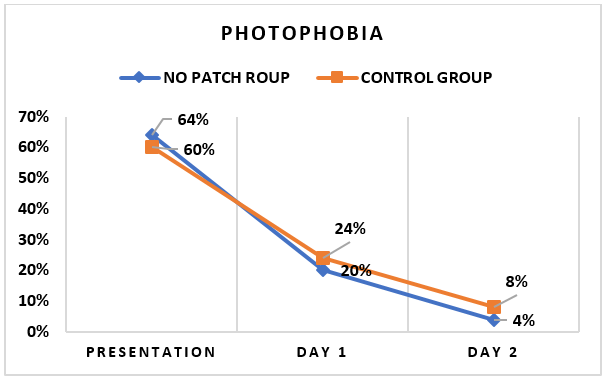
Photophobia |
|||
|
Presentation |
30 (60%) |
32 (64%) |
|
|
Day 1 |
10 (20%) |
12 (24%) |
0.731912 |
|
Day 2 |
2 (4%) |
4 (8%) |
0.437513 |
|
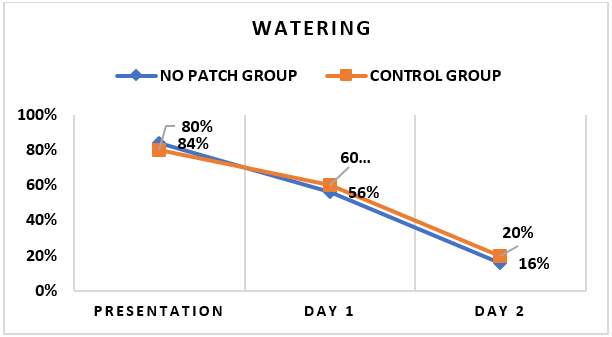
Tearing |
|||
|
Presentation |
40 (80%) |
42 (84%) |
|
|
Day 1 |
28 (56%) |
30(60%) |
0.887402 |
|
Day 2 |
8 (16%) |
10 (20%) |
0.67698 |
|
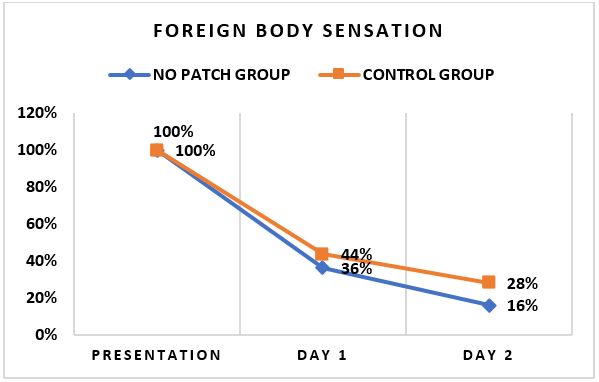
Foreign body sensation |
|||
|
Presentation |
50 (100%) |
50 (100%) |
|
|
Day 1 |
18 (36%) |
22 (44%) |
0.414216 |
|
Day 2 |
8(16%) |
14 (28%) |
0.147501 |
|
"Blurry vision" |
|||
|
Presentation |
24 (48%) |
22 (44%) |
|
|
Day 1 |
18(36%) |
20 (40%) |
0.15265 |
|
Day 2 |
08(16%) |
10(20%) |
0.479762 |
|
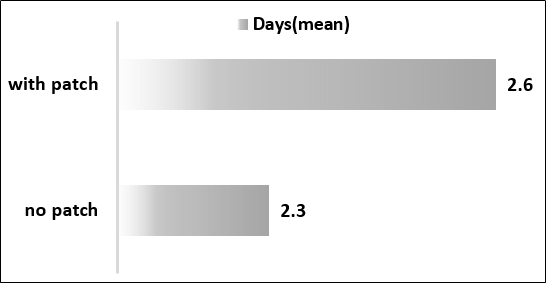
Days till healed (days)* |
2.3 |
2.6 |
0.210027279 |
[Table 3], [Table 4] shows the characteristics of the no-patch and control groups for traumatic corneal abrasions.
Patients in the no-patch group had less pain then the control group at 24-hour follow-up. The control group's pain scale score averaged 2.80, whereas the no-patch group's average score was 1.90. In addition, the difference in the pain scale score between presentation and 24-hour follow-up was 3.6 in the no-patch group and 2.8 in the control group.
The no-patch group showed significantly faster healing times. The control group took average 2.6 days to heal, whereas the no-patch group took 2.3 days. Table 3 shows that fewer symptoms were reported by the no-patch group. 44% percent of patients in the control group reported blurred vision, compared with 17% of patients in the no-patch group. Furthermore, the no-patch group had better compliance with the treatment protocols. Among patients in the control group, 8 (16%) removed their eye patch before the end of the 24-hour treatment period due to different reasons including discomfort and accidental removal while all the patients of no patch group were compliant to treatment. Except for improvement in watering all the values found in the study was statistically significant.
During the study, no systemic complications and no allergic reactions were observed in either group secondary to the treatment protocols.
Discussion
In our study, young adults were more likely to present with corneal abrasions. The average age of study participants was 32 years, and 70% of patients were male. The predisposition to injuries were equal between eyes. Most of the corneal abrasions were secondary to trauma (50%), where as 40% were secondary to removal of corneal foreign bodies.
Corneal epithelial defects heal by migration and proliferation of cells at the margins of the abrasion over the denuded area.[3], [5] For abrasions involving less than 60% of the total corneal surface area, there is an exponential decrease in wound size with time and wounds heal in 1-4 days. With both methods of treatment all abrasions in this study healed within 3 days. The corneal abrasions took 2.6 days to heal in the patch group, compared with 2.3 days in the no-patch group so it appears that the control group healed faster.[5]
Not only healing times were increased the patching caused discomfort in the group of patients who received a pressure patch leading to 8 persons not complying with the treatment protocol. Patients in the no-patch group had significantly faster healing times and lower pain level scores and had a better compliance with treatment protocols.[5] All of the patients in the no-patch group had complied with the study guidelines.
Pitfalls
As with any study of this size, in the current study, statistical error and bias may be present. Although we made every attempt to minimize these errors, some were unavoidable. Because the patients were entered into the study after the diagnosis was made and were randomized at that time, the observer and patients were not masked to the treatment protocol. This allowed for the possibility of observer bias. In addition, follow-up visits often allowed the observer the chance to determine what treatment protocol the patient was in. To circumvent this problem, we performed both subjective and objective measurements of healing; however, we could not eliminate this source of error. Also, we did not chart the amount of mild oral analgesics consumed by the study participants.
Conclusion
Amidst the various school of thought about patching in corneal abrasion, various studies have shown both the merits and demerits of patching. Though the exact mechanism of action of pathing is not lucid possibly it reduces the mechanical friction by preventing blinking. On the contrary some speak against patching saying that pressure patching over a closed eye lid chokes the corneal oxygenation leading to anaerobic metabolism that depletes the corneal glycogen reserve. The pressure patch may locally increase the corneal temperature that slows down healing and can invite microbial invasion. It has been seen that there is a reluctant attitude of patient towards patching because of two conditions one psychological effect making it appear as a grave disease and number two the loss of binocularity. One thing to take into consideration that if an undetected foreign body remains in the conjunctival fornixes a pressure patch on a bad day can cause impaction of foreign body which in due course of time can become nidus of infection. Thus, although the pressure patch has some theoretical advantages, our results combined with the risk of complications from application of a pressure patch suggest that future treatment of corneal abrasions should not involve use of the pressure patch.
Source of Funding
None
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- . Traumatic corneal abrasion. Lancet 1987. [Google Scholar]
- A P Chiapella, A R Rosenthal. One year in an eye casualty clinic.. Br J Ophthalmol 1985. [Google Scholar] [Crossref]
- H Jackson. Effect of Eye-pads on Healing of Simple Corneal Abrasions. BMJ 1960. [Google Scholar] [Crossref]
- P L Gregersen, E Ottovay, C Kobayashi, S E Hansen, J Bohnstedt. Treatment of corneal abrasion. Ugeskr Laeger 1991. [Google Scholar]
- J N P Kirkpatrick, H B Hoh, S D Cook. No eye pad for corneal abrasion. Eye 1993. [Google Scholar] [Crossref]
- M F G Hulbert. Efficacy of eyepad in corneal healing after corneal foreign body removal. Lancet 1991. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Deka B, Dutta SK, Deb S, Goswani H, Ahmed T. Effectiveness of patching and non-patching in treatment of corneal abrasion: A comparative study [Internet]. Indian J Clin Exp Ophthalmol. 2020 [cited 2025 Sep 12];6(4):616-621. Available from: https://doi.org/10.18231/j.ijceo.2020.129
APA
Deka, B., Dutta, S. K., Deb, S., Goswani, H., Ahmed, T. (2020). Effectiveness of patching and non-patching in treatment of corneal abrasion: A comparative study. Indian J Clin Exp Ophthalmol, 6(4), 616-621. https://doi.org/10.18231/j.ijceo.2020.129
MLA
Deka, Baby, Dutta, Saura Kamal, Deb, Shibashis, Goswani, Harish, Ahmed, Tanveer. "Effectiveness of patching and non-patching in treatment of corneal abrasion: A comparative study." Indian J Clin Exp Ophthalmol, vol. 6, no. 4, 2020, pp. 616-621. https://doi.org/10.18231/j.ijceo.2020.129
Chicago
Deka, B., Dutta, S. K., Deb, S., Goswani, H., Ahmed, T.. "Effectiveness of patching and non-patching in treatment of corneal abrasion: A comparative study." Indian J Clin Exp Ophthalmol 6, no. 4 (2020): 616-621. https://doi.org/10.18231/j.ijceo.2020.129
