- Visibility 296 Views
- Downloads 69 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2020.117
-
CrossMark
- Citation
Clinical correlation of glaucoma with systemic hypertension and its effect on visual morbidity
- Author Details:
-
Radha Anamalai *
-
P Priyadharshini
-
M Muthayya
Abstract
Background: Glaucoma and hypertension share a common pathophysiology of altered sodium transport in the renal and ciliary epithelium and can co exist. High blood pressure is a significant risk factor for glaucoma progression due to intraocular pressure spikes.
Aims: This study was performed to evaluate the association of hypertension with glaucoma and to assess the extent of optic disc damage, the role of anti hypertensive medications and visual morbidity.
Materials and Methods: This is a prospective, multidisciplinary study performed on a cohort of 118 hypertensive patients over 1 year. Ophthalmic examination, ancillary ocular investigations, systemic tests and multi speciality referrals were obtained for all patients.
Results: Among 118 hypertensive patients, 64 (54.8%) had glaucoma. 65 patients (55.1%) were female and 53 patients (44.1%) male. Age group most frequently affected was between 60 and 70 years. There was increased incidence of ocular hypertension which was statistically significant (p value of 0.02). The range of IOP in those on anti hypertensive medications was 10-16 mmHg which was statistically significant (p value = 0. 03).
Discussion: Risk of glaucoma in hypertension was higher in women. An elevation of diastolic blood pressure is more significant than systolic BP in raising IOP. Decreased IOP was highest among patients taking calcium channel blockers.
Conclusion: Hypertension can cause both reduction and elevation in IOP. Treatment of hypertension does lower the IOP and prevent further progression of glaucoma and prevent any visual loss.
Introduction
Glaucoma is a common blinding disease which is due to damage to the optic nerve and raised intraocular pressure being a major modifying risk factor.[1] It initially results in peripheral visual field loss followed by loss of central visual field and eventually leads to tunnel vision if not treated early and appropriately.[2] Hypertension due to raised systemic blood pressure (BP) both diastolic and/or systolic is associated with morbidities like stroke, cardiovascular, renal or ocular disease. It has been reported that high blood pressure is a significant risk factor for glaucoma progression.[3] Ocular perfusion pressure is given by the difference between arterial and venous BP. Low ocular perfusion pressure is associated with decreased nutrient and blood supply to optic nerve head (ONH), triggering ischemia of the ONH. This leads to reduced transmission of axoplasmic flow and its stasis.[4] Hypertension and raised intra ocular pressure share an overlapping pathophysiology.[5]
Altered sodium transport in distal nephrons and ciliary epithelium mediated by corticosteroid receptors and enzyme 11β-hydroxysteroid dehydrogenase has been found to be a common biochemical process in the occurrence of hypertension and glaucoma.[6], [7] Increasing age is a common risk factor in primary open angle glaucoma and hypertension.[8] Oral hypotensive medications are effective in lowering raised blood pressure and thereby reduce the complications of raised BP. Drugs used in the treatment of hypertension are also known to produce changes in the intraocular pressure. This study was performed to evaluate the association between hypertension and occurrence of glaucoma. The extent of optic disc damage and the visual morbidity in our patients along with the effects of type and duration of hypertension medications on the levels of intraocular pressure (IOP) were also evaluated.
Materials and Methods
This is a prospective hospital based study conducted in Sri Ramachandra Institute of Higher Education and Research on a cohort of 118 patients over a period of 1 year from January 2019 to December 2019.
It was performed on 118 patients between the age groups of 30 to 70 years which included newly diagnosed hypertensives and previously diagnosed hypertensives receiving treatment and on follow up now. Patients with other systemic diseases or vascular pathologies were excluded from the study. Those with hypertension but less than 30 years of age were not enrolled into the study as both glaucoma and hypertension could be due to congenital causes in young individuals.
The study was performed after ethics committee approval (CSP- MED/19/APR/52/40) was obtained. Patients were incorporated after getting informed consent from each one and the study was explained to them. All patients had a minimum follow up of 6 months and the need for regular review visits was explained to them. During the first visit and each follow up opinions regarding the progress of hypertension was obtained from departments of cardiology, internal medicine and neurology.
Patients are classified as hypertensive based on elevated BP readings of >120/80 mm Hg on two separate occasions according to current American Heart Association.[9]
Blood pressure measurements were made over 3 visits and the average of last two measurements was used for analysis. Recording was done with manual sphygmomanometer. The oral hypotensive medication taken by patients were categorized into 5 groups as calcium channel blockers(CCB), diuretics, angiotensin converting enzyme inhibitors (ACE), angiotensin receptor blockers and beta blockers.
Glaucoma was defined as progressive optic neuropathy associated with visual field loss in which IOP is a modifiable factor according ICO Glaucoma Guidelines.
A detailed history of age, sex, duration of hypertension, history of other co morbidities and treatment were collected. The participants then underwent a detailed ophthalmological evaluation including visual acuity, anterior segment evaluation using slit-lamp bio-microscopy and fundus evaluation using a + 90 D lens/ indirect ophthalmoscope. IOP measurement was done by applanation tonometry with Goldman Applanation Tonometer. Fluorescein was instilled in each eye and the tonometer was set at 10mmHg. Mires were viewed through the prism and measurements were read from the rotating dial. The same procedure was repeated in the other eye. Phasing technique of repeating recordings was done and the average IOP was used in the study. Gonioscopy was performed and the visual field of patients was analysed using Humphrey visual field analyser.
The collected data were analysed using IBM SPSS statistics software 23.0 Version. To describe about the data descriptive statistics frequency analysis, percentage analysis were used for categorical variables and the mean & S.D were used for continuous variables. To find if significant difference existed between the bivariate samples in independent groups the unpaired sample t-test was used. To find the significance in categorical data Chi-Square test was used. In both the above statistical tools the probability value 0.05 was considered as a significant level.
Results
Among the 118 hypertension patients involved in the study, 64 patients (54.8%) were found to have glaucoma. 65 patients (55.1%) were female and 53 patients (44.1%) were male. Age group affected was 12% between 30-40 years, 27% between 50 to 60 years and 60% between 60 and 70 years, the mean age being 59 years.
Hypertensive patients diagnosed with having glaucoma had a mean duration of 4.26 years. Among the 40 newly diagnosed patients 26 patients had glaucoma and 14 patients did not have glaucoma. They had been on oral hypertension medications for a duration ranging from 1 month to 6 months.
32 (13%) patients with increased of greater than 20mm Hg systolic BP had an increase of IOP. 112 (73%). 27 patients (40%) with a diastolic BP raise of 10mmHg had 0.6mm raise of IOP. Those with increase in IOP were treated with medical management in 81%, (topical beta blockers in 61%, prostaglandin analogues in 12%, alpha agonists in 9% and combination therapy in 21%), surgical management (trabeculectomy) in 12%.
Type of glaucoma associated with systemic hypertension was primary open angle glaucoma (POAG) in 9 patients (13)%, ocular hypertension (OHT) in 78 patients (87%) and normal tension glaucoma (NTG) in 2 patients 3%. The increased incidence of OHT among hypertensives was statistically significant with a p value of 0.02. We did not see any association with angle closure glaucoma or secondary open angle in any of our patients.
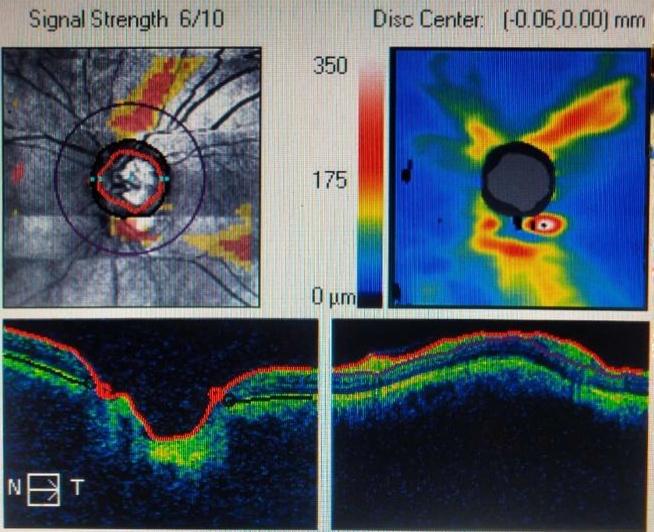
In those with OHT, predominant fundus changes were seen as increased cup disc ratio in 12%% and neuroretinal thinning in 9%. Visual field analysis showed nasal step with isolated scotomas in the Bjerrum’s area as the commonest change in 5% patients. Corneal thickness in patients diagnosed with ocular hypertension was on an average 0.720 +/-0.02mm. Thicker cornea was noted in 32%. Thinner cornea was noted in 2% of patients.
The oral hypotensive medication taken by patients were categorized into 5 groups as calcium channel blockers(CCB), diuretics, angiotensin converting enzyme inhibitors (ACE inhibitors), angiotensin receptor blockers (ARB) and beta blockers. Total number of patients taking oral hypertensives was 78. In the group on medications the range of IOP was between 14- 26mmHg.
Decreased IOP was highest among patients taking CCB in 25 patients (50%), followed by beta blockers in 14 patients (44.4%), ACE inhibitors, ARB and diuretics in 1 patient. The range of IOP in the treated population was between 10-16mmHg and this difference in those on hypertension medications was statistically significant with p value = 0. 03.
|
HTN Duration |
|
N |
Mean |
STD Deviation |
P Value |
|
Glaucoma |
Yes |
46 |
4.26 |
4.511 |
0.744 |
|
No |
52 |
6.94 |
4.913 |
|
Medication |
Glaucoma |
Total |
||
|
|
|
No |
Yes |
|
|
CCB |
Count |
25 |
25 |
50 |
|
% |
50% |
50% |
100% |
|
|
Diuretics |
Count |
4 |
1 |
5 |
|
% |
80% |
20% |
100% |
|
|
ACE inhibitors |
Count |
21 |
16 |
37 |
|
% |
56.8% |
43.2% |
100% |
|
|
ARB |
Count |
9 |
8 |
17 |
|
% |
52.9% |
47.1% |
100% |
|
|
Beta blockers |
Count |
5 |
4 |
9 |
|
% |
55.6% |
44.4% |
100% |
|
|
Total |
Count |
64 |
54 |
118 |
|
% |
54.2% |
45.8% |
100% |

Discussion
Intraocular pressure is affected by raised systemic blood pressure. The overlapping pathogenesis in both hypertension and glaucoma has been found to be due to an increased blood pressure especially systolic which increases ciliary artery perfusion pressure.[10] This in turn leads to an increased filtration of aqueous fluid through the ciliary body thus causing elevation in IOP.[11] Raised blood pressure also affects the episcleral venous pressure which regulates the aqueous flow across trabecular meshwork through Schlemms canal.[12] However, we found in our patients that an increased diastolic BP more frequently caused raised IOP.
It has been reported following various studies that for every 1mm increase in perfusion pressure there will be an increase of 1mm in IOP. There is an alteration in sodium transport in the distal nephrons and ciliary epithelium, leading to increased excursion of sodium into the renal filtrate and aqueous humour respectively. This is mediated by corticosteroid hormone (cortisol and aldosterone) and glucocorticoid and mineralocorticoid receptors.[13]
In our study, OHT was the commonest type of glaucoma and was associated with structural and functional changes in the optic nerve head and visual fields. It has already been established in literature that a thinner or thicker cornea can give IOP readings which may be higher or lower than the actual value. A correction to the recorded IOP is always has to be done based on the pachymetry readings before treatment for glaucoma is started.
Reduced IOP readings were associated more in patients taking CCB, ACE inhibitors and ARB drugs. This is in concurrence with Langman et al. who stated that IP association showed increased odds ratio in hypertensive patients taking CCB, ACE inhibitors and ARB drugs.[14]
Klein et al. stated that beta blocker drugs had a protective effect for glaucoma and hypertension. [15] In our study we noted that those on calcium channel blockers had least involvement of the ONH but those on beta blockers had lowest recordings of IOP. This variation of effects on glaucoma has not been reported in previous studies to the best of our knowledge. Leske et al. found that antihypertensive drugs was not associated with any increased risk of open angle glaucoma but that ocular perfusion pressure has a significant effect on IOP.[16] From our cohort of patients we found that oral anti hypertensive drugs does have beneficial effect in the control of IOP.
However we feel that systemic beta blockers are another important factor that would have to be considered as they may mask an elevated IOP making a diagnosis of glaucoma difficult. IOP though only a risk factor is important because it is the only treatable factor in glaucoma that can secondarily prevent progression of changes in the optic nerve head or visual field.
Specifically, ACE inhibitors caused reduction in IOP only on long term use (greater than 1 year) although widely prescribed as antihypertensive agents. Calcium channel blockers and beta blockers in combination with CCB can increase ocular blood flow and thus play a neuro protective effect by reducing apoptosis of neurons.
Different anti hypertensive medications are chosen based on associated heart failure or other systemic diseases and knowledge of the effect on IOP will be useful.[17] Beta blockers are not preferred in heart blocks or pulmonary obstructive disease and in such situations ACE inhibitors are used. CCB are usually second line agents.[18] Another important facet of treatment to be considered is that topical beta blockers in glaucoma management are not efficient in those on systemic beta blockers and hence treatment will have to be titrated accordingly.
There is an increased risk of glaucoma with both high and low BP. Drugs that can lower BP may sometimes increase the incidence of glaucoma due to specific effects on the optic nerve head. The exact cause of this complex relationship has not been understood but various influencing factors such as relationship between blood pressure and ocular perfusion pressure, dysfunctional autoregulation and peripheral vascular capacity have been suggested.[19]
We found that the risk of glaucoma in hypertension is higher in women. Among all drugs used in the treatment of hypertension we concluded from our study that beta blockers protect and calcium channel blockers and ACE inhibitors have a lesser effect on glaucoma. The limitation of the study was that the sample size and duration of study was less and a longer follow up could have provided more insight into disease progression. Hypertension and IOP have common biomechanical alteration in their pathogenesis.[20] Treatment of hypertension does lower the IOP and prevent further progression of glaucoma and prevent any visual loss.[21] A multidisciplinary approach which involves the ophthalmologist and treating physician will help in holistic monitoring the patient.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Maurya RP. Glaucoma Burden: Indian Scenario. Indian J Clin Exp Ophthmol. 2017;3(4):387-8. [Google Scholar]
- Maurya RP. Recent advances in glaucoma management. Indian J Clin Expl Ophthalmol. 2019;5(2):140-1. [Google Scholar] [Crossref]
- Deb AK, Kaliaperumal S, Rao VA, Sengupta S. Relationship between systemic hypertension, perfusion pressure and glaucoma: A comparative study in an adult Indian population. Indian J Ophthalmol. 2014;62(9):917-22. [Google Scholar] [Crossref]
- Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM. The impact of ocular blood flow in glaucoma. Prog Retinal Eye Res. 2002;21(4):359-93. [Google Scholar] [Crossref]
- Langman MJS. Systemic hypertension and glaucoma: mechanisms in common and co-occurrence. Br J Ophthalmol. 2005;89(8):960-3. [Google Scholar] [Crossref]
- Omoti AE, Enock ME, Okeigbemen VW, Akpe BA, Fuh UC. Vascular risk factors for open angle glaucoma in African eyes. Middle East Afr J Ophthalmol. 2009;16(3). [Google Scholar] [Crossref]
- Maurya R. Biomarkers of primary open-angle glaucoma. Ind J Clin Exp Ophth. 2017;3(4):387-388. [Google Scholar]
- Deokule S, Weinreb RN. Relationships among systemic blood pressure, intraocular pressure, and open-angle glaucoma. Can J Ophthalmol. 2008;43(3):302-7. [Google Scholar] [Crossref]
- Costa VP, Arcieri ES, Harris A. Blood pressure and glaucoma. Br J Ophthalmol. 2009;93(10):1276-82. [Google Scholar] [Crossref]
- Bill A. The role of ciliary blood flow and ultrafiltration in aqueous humor formation. Exp Eye Res. 1973;16(4):287-98. [Google Scholar] [Crossref]
- Moraes CGD, Cioffi GA, Weinreb RN, Liebmann JM. New Recommendations for the Treatment of Systemic Hypertension and their Potential Implications for Glaucoma Management. J Glaucoma. 2018;27(7):567-71. [Google Scholar] [Crossref]
- Melgarejo JD, Lee JH, Petitto M. Glaucomatous optic neuropathy associated with nocturnal dip in blood pressure: findings from the Maracaibo Aging Study. Ophthalmol. 2018;125:807-14. [Google Scholar]
- Chen HY, Lai SW. Relation between intraocular pressure and systemic health parameters in Taiwan. South Med J. 2005;98(1):28-32. [Google Scholar]
- Langman MJS. Systemic hypertension and glaucoma: mechanisms in common and co-occurrence. Br J Ophthalmol. 2005;89(8):960-3. [Google Scholar] [Crossref]
- Klein BE, Klein R, Knudtson MD. Intraocular pressure and systemic blood pressure: longitudinal perspective: the Beaver Dam Eye Study. Br J Ophthalmol. 2005;89(3):284-291. [Google Scholar]
- Leske MC. Ocular perfusion pressure and glaucoma: clinical trial and epidemiologic findings. Curr Opin Ophthalmol. 2009;20(2):73-8. [Google Scholar] [Crossref]
- Levine RM, Yang A, Brahma V, Martone JF. Management of Blood Pressure in Patients with Glaucoma. Curr Cardiol Rep. 2017;19(11). [Google Scholar] [Crossref]
- Krasińska B, Karolczak-Kulesza M, Krasiński Z, Pawlaczyk-Gabriel K, łopatka P, Głuszek J. Effects of the time of antihypertensive drugs administration on the stage of primary open-angle glaucoma in patients with arterial hypertension. Blood Press. 2012;21(4):240-8. [Google Scholar] [Crossref]
- Schmidl D, Garhofer G, Schmetterer L. The complex interaction between ocular perfusion pressure and ocular blood flow – Relevance for glaucoma. Exp Eye Res. 2011;93(2):141-55. [Google Scholar] [Crossref]
- Flammer J, Konieczka K, Bruno RM, Virdis A, Flammer AJ, Taddei S. The eye and the heart. Eur Heart J. 2013;34(17):1270-8. [Google Scholar] [Crossref]
- Horwitz A, Klemp M, Jeppesen J, Tsai JC, Torp-Pedersen C, Kolko M. Antihypertensive Medication Postpones the Onset of Glaucoma. Hypertens. 2017;69(2):202-10. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Anamalai R, Priyadharshini P, Muthayya M. Clinical correlation of glaucoma with systemic hypertension and its effect on visual morbidity [Internet]. Indian J Clin Exp Ophthalmol. 2020 [cited 2025 Oct 30];6(4):558-562. Available from: https://doi.org/10.18231/j.ijceo.2020.117
APA
Anamalai, R., Priyadharshini, P., Muthayya, M. (2020). Clinical correlation of glaucoma with systemic hypertension and its effect on visual morbidity. Indian J Clin Exp Ophthalmol, 6(4), 558-562. https://doi.org/10.18231/j.ijceo.2020.117
MLA
Anamalai, Radha, Priyadharshini, P, Muthayya, M. "Clinical correlation of glaucoma with systemic hypertension and its effect on visual morbidity." Indian J Clin Exp Ophthalmol, vol. 6, no. 4, 2020, pp. 558-562. https://doi.org/10.18231/j.ijceo.2020.117
Chicago
Anamalai, R., Priyadharshini, P., Muthayya, M.. "Clinical correlation of glaucoma with systemic hypertension and its effect on visual morbidity." Indian J Clin Exp Ophthalmol 6, no. 4 (2020): 558-562. https://doi.org/10.18231/j.ijceo.2020.117
