- Visibility 30 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijceo.2020.101
-
CrossMark
- Citation
Bilateral branched retinal vein occlusion in a patient on oral contraceptive pills: A case report
- Author Details:
-
Parthapratim Roy *
-
Saura Kamal Dutta
Introduction
Retinal vein occlusion (RVO), the most common acquired retinal vascular pathology in adults.[1] RVO can be central (CRVO), hemi-central (HRVO) or branch retinal vein occlusion (BRVO). The reported prevalence of CRVO is 0.8, RVO is 5.2/1000, and 4.42 for BRVO.[2] Important risk factors for BRVO in young patients are increased body mass index, hyperlipidemia, systemic hypertension, thrombophilia and oral contraceptive pills.[3], [4] Other risk factors associated with retinal vein occlusion are smoking, alcohol consumption, cardiovascular disorders, sedentary life style, bleeding or clotting disorders, vasculitis, dehydration, closed-head trauma, glaucoma and autoimmune disorders e.g. lupus, antiphospholipid antibody syndrome, & sarcoidosis.
Oral contraceptive pills (OCP) treatment is one of most popular birth control methods in young population. The health benefits of these drugs are numerous and outweigh the risks of their use in some cases like when used for protection against ovarian and endometrial cancers, benign breast disease, pelvic inflammatory disease, iron-deficiency anemia and ectopic pregnancy. It has also been suggested that oral contraceptives may provide a benefit on bone mineral density, uterine fibroids, toxic shock syndrome, and colorectal cancer. Dysmenorrhea, irregular or excessive bleeding, acne, hirsutism, and endometriosis-associated pain are common targets for oral contraceptive therapy Although well tolerated there are a couple of ocular side effects such as retinal vascular thrombosis, retinal vitreous hemorrhage, serous chorioretinopathy. Although rare severe side effects includes thrombosis of central retinal vein or artery or acute ischemic optic neuropathy. Rise in the usage of OCP & its role in causing various problems like retinal vascular occlusions is a cause of concern. Here we present the case of a young patient who was on OCP without any other risk factors for thrombosis that was diagnosed with bilateral BRVO.
Case Report
A 35-year-old female presented to us with bilateral blurred vision and headache, started three weeks ago. The dimness of vision was gradual in onset, painless, without any history of trauma, discharge, photophobia, She was a non-smoker, normal BMI, without any comorbidities, and was not on any long-term medication, except the oral contraceptive pills(ethinyl-estradiol 0.030 mg and levonorgestel 0.150 mg) she was taking for the last two years. On examination, visual acuity in right eye was 6/60 while in the left eye was 4/60. Intraocular pressure and on slit-lamp.
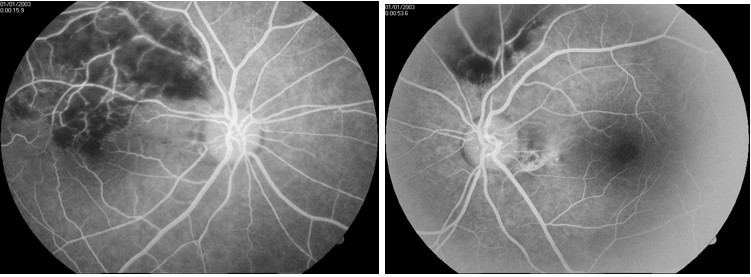
exam all the anterior segment findings were found to be within normal limits in both eyes. Fundoscopic examination in both eyes were similar and it revealed flame-shaped intraretinal hemorrhage, dilated and sinuous veins, cotton-wool exudate and narrow arteries, and edematous retina in the region of superior temporal retinal vein ([Figure 1]) which was confirmed on Fundus fluorescent angiography (FFA) ([Figure 2]). A full assessment which included ruling out any family history of thromboembolic disorders, laboratory testing directed towards identifying various systemic vascular problems, basic workup including complete blood cell count (CBC), glucose tolerance test, lipid profile, coagulation profile, activated partial thromboplastin time (a PTT), Venereal Disease Research Laboratory (VDRL), thrombophilia screening, testing for lupus anticoagulant and anticardiolipin antibodies. Excluded cardiovascular pathology, diabetes mellitus, coagulopathy or autoimmune conditions. A diagnosis of BRVO was established and appropriate therapy instituted.

Differential diagnosis
A thorough history taking and clinical examination including the slit-lamp and fundus exam in a must for diagnosing any case of decreased vision symptoms. But for retinal vascular condition suspicion, evaluation for risk factors becomes the priority presence of diabetes mellitus, hypertension, coagulopathies, hyperlipidemia, advanced age, cigarettes smoking, vasculitis, infection or medication (OCP, drug abuse) should be considered. BRVO can be major, macular or peripheral, depending on the retinal area involved. The type and extent of occlusion is also important. Retinal artery occlusion an ophthalmologic emergency presents with sudden onset symptoms and has a very poor prognosis. Obstruction of the ophthalmic or internal carotid artery can lead to visual field loss as well.
Treatment
The patient was advised to stop OCP and was advised with intravitreal anti-vascular endothelial growth factor injection (Bevacizumab). Follow up was done for six weeks very week after the first injection. The visual acuity gradually improved with decrease of edema and hemorrhage. The patient was reevaluated monthly and gradually a full recovery of visual acuity was noticed.
Discussion
In retinal vein occlusions, the exact pathogenesis of the thrombotic occlusion of the central retinal vein is not known. Thrombotic occlusion of the central retinal vein can occur as a result of compression of the vein due to structural changes in lamina cribrosa like in glaucomatous cupping, inflammatory swelling in optic nerve, hemodynamic disturbances which cause hyperdynamic or sluggish circulation, vessel wall changes in vasculitis, and due to changes in the blood like in deficiency of thrombolytic factors, or the increase in clotting factors.
Occlusion of the central retinal vein leads to the logging of the blood in the retinal venous system and increased resistance to venous blood flow this causes ischemic damage to the retina. This ischemic damage to the retina stimulates production of vascular endothelial growth factor (VEGF) in the vitreous cavity which stimulate neovascularization of the posterior and anterior segment (secondary complications due to central retinal vein occlusion). Also, it has been shown that VEGF causes capillary leakage leading to macular edema.
The OCPs are used in management of wide spectrum of diseases including the treatment of functional ovarian cysts, polycystic ovarian syndrome, dysfunctional uterine bleeding, and puberty menorrhagia. Besides their main effect oral contraceptives have been implicated in central retinal vein occlusion and the mechanisms for retinal vascular occlusion development, symptomatology, clinical features, and treatment modalities remain the same as with other predisposing factors for central retinal vein occlusion.[5]
Various studies have being done in this field and notable ones include Vessev et al,[6] Kirwan et al.[7] and Scoditti et al.,[8] In the cohort study by Vessev et al., [6] they found the eye disease with increase in risk in oral contraceptives users was a retinal vascular problem. Similarly, Kirwan et al.[7] said the prevalence of retinal vein occlusion in female patients less than 35 years taking the OCP was 66.0%. Scoditti et al.,[8] reported that the use of low estrogen oral contraceptives was associated with an increased risk of cerebral venous thrombosis and ischemic stroke,
Oral contraceptive pills are known as pro-coagulants and OCPs used in our case contained a small dose of estrogen (30 μg) and a second generation progestin. The thrombotic risk associated with OCP use was proved to decrease with reduced estrogen dose and third generation progestin use.[9]
Conclusions
BRVO is an uncommon complication in young patients without comorbidities. There was no other cause for retinal venous thrombosis in this patient apart from OCP treatment. Considering the available data, it is reasonable to consider a causal association between OCP and BRVO.
Source of Funding
None.
Conflict of Interest
None.
References
- M Bradvica, T Benašić, M Vinković, S Rumelt. Retinal Vascular Occlusions. Advances in Ophthalmology 2012. [Google Scholar]
- S Rogers, R L McIntosh, N Cheung, L Lim, J J Wang, P Mitchell. The Prevalence of Retinal Vein Occlusion: Pooled Data from Population Studies from the United States, Europe, Asia, and Australia. Ophthalmol 2010. [Google Scholar]
- H D Lam, J M Lahey, J J Kearney, R R Ng, J M Lehmer, S C Tanaka. Young patients with branch retinal vein occlusion: a review of 60 cases. Retina 2010. [Google Scholar]
- C Glueck, R K Hutchins, J Jurante, Z Khan, P Wang. Thrombophilia and retinal vascular occlusion. Clin Ophthalmol 2012. [Google Scholar]
- V Beral, C Hermon, C Kay, P Hannaford, S Darby, G Reeves. Mortality associated with oral contraceptive use: 25 year follow up of cohort of 46 000 women from Royal College of General Practitioners' oral contraception study. BMJ 1999. [Google Scholar]
- M P Vessey, P Hannaford, J Mant, R Painter, P Frith, D Chappel. Oral contraception and eye disease: findings in two large cohort studies. Br J Ophthalmol 1998. [Google Scholar]
- J F Kirwan, M D Tsaloumas, H Vinall, P Prior, E E Kritzinger, P M Dodson. Sex hormone preparations and retinal vein occlusion. Eye 1997. [Google Scholar]
- U Scoditti, G P Buccino, M Pini, C Pattacini, D Mancia. Risk of acute cerebrovascular events related to low oestrogen oral contraceptive treatment. Ital J Neurol Sci 1998. [Google Scholar]
- R K Shrestha, J K Shrestha, S Koirala, D N Shah. Association of systemic diseases with retinal vein occlusive disease. JNMA J Nepal Med Assoc 2006. [Google Scholar]
