- Visibility 137 Views
- Downloads 14 Downloads
- DOI 10.18231/j.ijceo.2020.090
-
CrossMark
- Citation
A comparison between retinoscopy and autorefraction in acceptance of subjective correction in school age children
- Author Details:
-
Sinchana Adyanthaya
-
Abhilash B *
Introduction
Refractive error is one of the most common causes of visual impairment around the world, especially among children aged 5-15 years accounting for 12.8 million, representing a prevalence of 0.97%.[1] Retinoscopy and subjective refraction remain the gold standard for assessing the refractive status in children. However, more recently, automated refractometers are widely used to assess the refractive status in children.[2] The accuracy of the technique used for measuring refractive error in children is crucial as the potential effects of underestimation and overestimation of the error lead to accommodative stress, thus increasing the possibility of amblyopia.
Discrepancies have been reported between the results of objective refraction obtained with autorefraction (AR), retinoscopy, and the correction which is accepted by patients on subjective refraction. The studies previously conducted have not been conclusive in determining the single most accurate technique. It is of utmost importance to understand which of the two methods of objective correction is better accepted by the patients, before deciding on the technique to be used as a standard one.
Hence the aim of this study is to determine which of these methods of refraction is more reliable in children. In this study, two different techniques of objective refraction, i.e, retinoscopy and autorefraction was compared and their accuracy in predicting the acceptance of subjective correction was observed.
Materials and Methods
It was a prospective randomised study of 1 year duration, from Jan 2017 to Dec 2017, conducted on 140 eyes of 70 school going children (6-15 years of age) with complaints of blurring of vision or asthenopic symptoms, attending the outpatient department of a tertiary care hospital in South India. Children with media opacities, abnormal fundus findings and diminished vision due to causes other than refractive error were excluded from the study. All children with refractive errors were enrolled for the study after obtaining informed consent from the parent/guardian and assent from the children.
A routine ophthalmological examination of both eyes was conducted to rule out any ocular co-morbidities. Anterior segment examination and posterior segment findings were recorded if any. Visual acuity was tested using Snellen’s chart. Uncorrected visual acuity and pinhole acuity and near vision was recorded for each eye.
Cycloplegia was then achieved using cyclopentolate 1% eyedrops, instilled thrice in the eye at 10 minute intervals. Cycloplegic auto refractometry and cycloplegic retinoscopy was performed, approximately 45-60 minutes after the first use of cyclopentolate 1%. Retinoscopy was done using Welch Allyn streak retinoscope, at 2/3rd metre distance, in a dark room using fixation target of Snellen’s drum at 6m distance, and loose trial lenses. Auto refraction was done using NIDEK AR 600 A auto refractor. Three values were taken and the average value used for analysis. After 3 days, subjective refraction, both monocular and binocular, was done until best corrected visual acuity was achieved.
Data analysis
Patient characteristics like age, sex, ocular examination findings, and refractive error estimation with retinoscope, AR and subjective acceptance were tabulated and summarized in the form of mean, SD, frequency (N) and percentage (%). The results of subjective refraction were compared with the findings of autorefraction and retinoscopy, and statistical analysis was carried out using Chi-square test. p value <0.05 was considered as statistically significant. The method which was near to subjective refraction was considered more accurate for the purpose of this study. Data was analyzed using MedCalc software. The agreement between measurements or accuracies obtained with different methods was analyzed using Bland and Altman[3] plots with 95% limit of agreement. Sensitivity and specificity of the different methods of refraction in diagnosing myopia (>/= -0.5D) and hypermetropia (> +2D) were calculated.
Results
Mean age of the study population was 10.99 years. Females constituted 57.1% while 42.9% of them were males. The male to female ratio was 1:1.33. Based on subjective refraction, 50% (70 eyes) were myopic and 41.4% (58 eyes) were hypermetropic. The mean negative sphere accepted subjectively was -1.26D with SD of 0.97. The mean positive sphere accepted subjectively was 2.4 dioptres with SD of 0.21. With reference to cylindrical power estimation, 43.6% of the eyes accepted negative cylinders and 15% of the eyes accepted positive cylinders.
| Method | Number of eyes | Mean | SD | 95% CI | P value* |
| Retinoscopy | 70 | -1.09 | 0.83 | -1.29 to -0.892 | 0.06 |
| AR | 70 | -1.52 | 1.2 | -1.8 to -1.24 | 0.0001 |
| Subjective | 70 | -1.26 | 0.97 | -1.49 to -1.02 |
| Number of eyes | Mean | SD | 95% CI | P value | |
| Retinoscopy | 58 | 2.44 | 0.21 | 2.38 to 2.49 | 0.06 |
| AR | 58 | 2.29 | 0.38 | 2.19 to 2.39 | 0.01 |
| Subjective | 58 | 2.4 | 0.21 | 2.34 to 2.46 |
On comparing the values of spherical error by retinoscopy and subjective refraction, 70 myopic eyes had mean of -1.09±0.83 on retinoscopy and -1.26 ±0.97 on subjective correction (p=0.06), while 58 hypermetropic eyes had mean of 2.44±0.21 on retinoscopy and 2.4±0.21 on subjective refraction (p=0.06).
On comparing the spherical error recorded by autorefractometer and subjective method, 70 myopic eyes had mean of -1.52±1.2 on autorefraction with a p value of 0.0001, while 58 hypermetropic eyes had mean of 2.29±0.38 on autorefraction resulting in p value of 0.01. Cylindrical error values recorded by retinoscopy when compared with subjective method showed a mean of -0.0839±0.304 and -0.157±0.384 respectively, with a p value of 0.0007. Whereas, when the values of cylindrical error analysed by autorefraction with a mean of -0.207±0.497, were compared with the subjective method (-0.157±0.384), it showed a statististical significance at p value of 0.0088.
| Method | Number of eyes | Mean | SD | 95% CI | P value * |
| Subjective | 140 | -0.157 | 0.384 | -0.221 to-0.093 | - |
| Retinoscopy | 140 | -0.0839 | 0.304 | -0.135 to -0.033 | 0.0007 |
| AR | 140 | -0.207 | 0.497 | -0.29 to -0.124 | 0.0088 |
Subjectively, 89.3% and 35% of the eyes accepted retinoscopy and AR sphere estimates respectively, 49.2% and 72.8% of the eyes accepted retinoscopy and AR cylinder estimates respectively and 55.7% and 75.7% of the eyes accepted the axis as estimated by retinoscopy and AR respectively.
On studying the intracluster correlation between retinoscopy and AR with subjective refraction using Bland Altman principle, it was observed that, for spherical power estimation, the correlation was higher for retinoscopy. AR was found to overestimate myopia and underestimate hypermetropia. For cylindrical power and axis estimation, the correlation was higher for AR than retinoscopy.
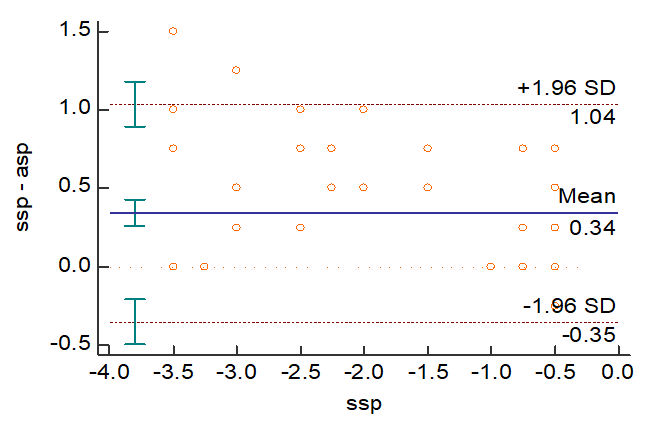
In [Figure 1], AR has overestimated the power to the extent of 0.34 D. The p value was found to be <0.0001, which is statistically significant.
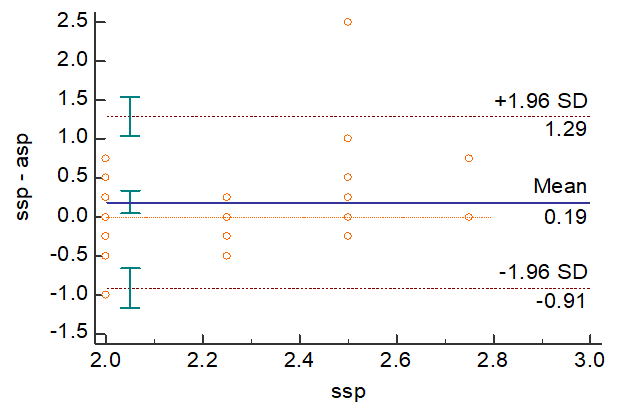
In [Figure 2], AR has underestimated the power to the extent of 0.19 D. The p value was found to be 0.0129, which is statistically significant.
On comparing the diagnostic accuracy of retinoscopy against subjective correction in myopic eyes, retinoscopy was found to have 100% sensitivity and 98.6% specificity. In case of hypermetropia, the sensitivity and specificity of retinoscopy was 100%. When the diagnostic accuracy of AR was compared against subjective correction, it was seen that AR has 100% sensitivity and 90% specificity for myopia whereas 87.9% sensitivity and 100% specificity for hypermetropia.
Discussion
Studies have suggested that during noncycloplegic autorefraction and noncycloplegic retinoscopy, the accommodative effort may not be completely neutralized, resulting in reduced accuracy, especially in children who have high accommodative reserve.[4], [5] Also Hepsen et al[6] suggested that one of the possible factors contributing to the rise in myopia prevalence in children is excess accommodation. Children wearing glasses with minus over correction would need to exert excess accommodative effort which may in turn predispose them to myopic progression.[2] To negate this, in the present study comparison was done under cycloplegic conditions.
In myopic eyes, the spherical error values obtained by retinoscopy was comparable to the subjective refraction, while autorefraction showed overestimation of myopia when compared with subjective refraction. In case of hypermetropic eyes, when compared with subjective acceptance, retinoscopy showed similar values whereas autorefraction underestimated the hypermetropia.
Bullimore MA et al[7] conducted a study to evaluate the accuracy of autorefraction using three autorefractors by comparing to subjective refraction in the diagnosis of refractive error in children.117 children were evaluated and the study concluded that all three autorefractors had a tendency towards minus over correction in children resulting in over diagnosis of myopia.
In our study, 89.3% eyes accepted the spherical power estimated by retinoscopy, while only 35% eyes accepted the spherical power as given by autorefraction. With respect to cylindrical powers, 49.2% eyes accepted the retinoscopy values, where as 72.8% eyes accepted the autorefraction values. Finally, retinoscopy estimates of axis of cylinder, were accepted in 55.7% eyes, while autorefraction values were accepted in 75.7% eyes, suggesting that while retinoscopy is a better modality for estimating the spherical powers, AR is more accurate in estimating the cylinder powers, along with their axis.
These findings agree with other previously published studies that observed a closer agreement between autorefraction and other refraction methods regarding the cylinder component, whereas poorer agreement was reported for the sphere component.[8], [9]
Jorge J et al[10] study observed a higher agreement between retinoscopy and subjective refraction for the sphere power component. For cylinder power and axis, autorefraction and retinoscopy displayed similar agreement.
According to a study by DeCarlo et al[11] comparing autorefraction with trial frame (subjective) refraction, it was found that auto refraction correlates well with trial frame refraction for cylinder power.
In our study, it was observed that retinoscopy and AR have comparable diagnostic accuracy similar to the results obtained by previous studies. Choong YF et al[2] reported that under cycloplegic conditions, autorefraction resulted in high sensitivity and specificity for myopia and high sensitivity for hypermetropia.
Verboven L et al[12] in their study observed that Nidek ARK-900, representing the third generation of objective refractors, is comparable and superior to retinoscopy in accuracy in children, can be easily run by ophthalmic technician and therefore eliminates the physician’s examination time required for retinoscopy.
In our study, the refractive status of school age children was assessed using conventional retinoscopy and autorefraction, and the accuracy of these objective methods was compared against subjective refraction. Both retinoscopy and autorefraction were found to have comparable diagnostic accuracy. However, it was observed that higher correlation was found with retinoscopy for spherical error, while autorefraction correlated better with subjective correction for cylindrical error and axis estimation.
Conclusion
In conclusion, it can be inferred that conventional retinoscopy is still the most accurate objective method to estimate the refractive status in children and can be considered a reliable starting point for subjective refraction, however, autorefraction has comparable accuracy and can be a valuable aid to prescribe cylindrical correction.
Source of Funding
None.
Conflict of Interest
None.
References
- D Pascolini, S P Mariotti. Global estimates of visual impairment: 2010. Br J Ophthal 2012. [Google Scholar]
- Y F Choong, A H Chen, P P Goh. A Comparison of Autorefraction and Subjective Refraction With and Without Cycloplegia in Primary School Children. Am J Ophthal 2006. [Google Scholar]
- P Cool, M M Ockendon. . Stats Book. Lancet 1986. [Google Scholar]
- W Wesemann, B Dick. Accuracy and accommodation capability of a handheld autorefractor. J Cataract Refractive Surg 2000. [Google Scholar]
- J Zhao, J Mao, R Luo, F Li, G P Pokharel, L B Ellwein. Accuracy of Noncycloplegic Autorefraction in School-Age Children in China. Optom Vis Sci 2004. [Google Scholar]
- I F Hepsen, C Evereklioglu, H Bayramlar. The effect of reading and near-work on the development of myopia in emmetropic boys: a prospective, controlled, three-year follow-up study. Vis Res 2001. [Google Scholar]
- M A Bullimore, R E Fusaro, C W Adams. The Repeatability of Automated and Clinician Refraction. Optom Vis Sci 1998. [Google Scholar]
- D A Goss, T Grosvenor. Reliability of refraction--a literature review. J Am Optom Assoc 1996. [Google Scholar]
- N A McBrien, M Millodot. Clinical Evaluation of the Canon Autoref R-1. Optom Vis Sci 1985. [Google Scholar]
- J Jorge, A Queiros, J B Almeida, M A Parafita. Retinoscopy/autorefraction: which is the best starting point for a noncycloplegic refraction. Optom Vis Sci 2005. [Google Scholar]
- D K DeCarlo, G McGwin, K Searcey, L Gao, M Snow, J Waterbor. Trial Frame Refraction versus Autorefraction among New Patients in a Low-Vision Clinic. Invest Opthal Vis Sci 2013. [Google Scholar]
- L Verboven, L Missotten. Possibilities and limitations of refraction measurement by an automatic refractor. Bull Soc Belge Ophtalmol 1983. [Google Scholar]
