- Visibility 21 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijceo.2020.087
-
CrossMark
- Citation
To study the association of urine microalbumine and the severity of diabetic retinopathy among type II diabetics: A hospital based cross sectional study
- Author Details:
-
Sheldon J Goudinho *
-
Jasmine M Jacob
-
Neethu Rollands
Introduction
Diabetes mellitus is considered as one of the most common metabolic disorders. The overall global prevalence of diabetes mellitus is estimated to increase from 4% in 1995 to almost 5.4% by the year 2025.[1], [2] The two most common complications seen among patients with long standing diabetes is diabetic retinopathy and nephropathy.
These are the two major microvascular complications of long standing diabetes. They are thought to be due to endothelial dysfunction mediated microvascular complications of diabetes mellitus.[1] Worldwide diabetic nephropathy is considered as one of the most common cause for the end stage renal disease.
Due to this high magnitude of damages that are caused by these microvascular complications, there is an urgent need for a sensitive marker, that will aid in the detection of both nephropathy and retinopathy. Microalbuminuria is almost widely accepted as the first clinical sign of diabetic nephropathy.[3] Early detection of diabetic retinopathy can be done by screening all the diabetic patients by doing a dilated Fundus evaluation.[4]
The association between the renal and cardiovascular complications with that of microalbuminuria among type I diabetics has been well established whereas in type 2 diabetes only a lesser association is observed.[5] Many researchers in their studies have suggested the role of microalbuminuria as an important marker for predicting the mortality, cardio vascular disease and renal failure even in individuals without diabetes mellitus. There are only very few studies that have been done to investigate the possible association between diabetic retinopathy and microalbuminuria.[6], [7]
Purpose of the Study
The aim of this study is to estimate the prevalence of albuminuria (microalbuminuria and macroalbuminuria) among type II diabetics and to determine its role as a risk factor for both the presence and the severity of diabetic retinopathy.
Materials and Methods
We conducted a hospital based cross sectional study in 360 patients with type 2 diabetes in the department of ophthalmology, DR SMCSI medical college hospital, Karakonam. All the patients had undergone a comprehensive ophthalmic evaluation. The ETDRS scale was used for grading Diabetic retinopathy. A morning urine sample was used to detect albuminuria. Urine albumin excretion of value 30 – 300 mg in 24 hours was regarded as microalbuminuria and values more than 300 mg in 24hours was regarded as macroalbuminuria. In our study immunoturbidity method was used to estimate the urine micro albumin level. The analysis was done using SPSS 16.0.
Results
The study was conducted on 360 diabetic patients. The number of females were 197 and males were 163. The mean age was found to be 63.48 (SD +6.921) years. The minimum age was found to be 42 years and the maximum age was 88 years among the study participants. In our study the mean duration of diabetes mellitus was 9.36 years with most participants in the range of 5-15 years duration. Among the 360 study participants studied, 141 of them had diabetic retinopathy which accounted for 39.2%. Remaining 219 participants did not have any diabetic retinopathy changes (60.80%).

Among the 141 participants with diabetic retinopathy studied, it was found that the prevalence of very mild NPDR was 13.5%, mild NPDR was 18.4%, moderate NPDR was 36.9%, severe NPDR was 10.6%, very severe NPDR was 5% and PDR was 15.6%.
| Types of Diabetic Retinopathy | Frequency (n=141) | Prevalence |
| Very Mild NPDR | 19 | 13.5% |
| Mild NPDR | 26 | 18.4% |
| Moderate NPDR | 52 | 36.9% |
| Severe NPDR | 15 | 10.6% |
| Very Severe NPDR | 7 | 5% |
| PDR | 22 | 15.6% |
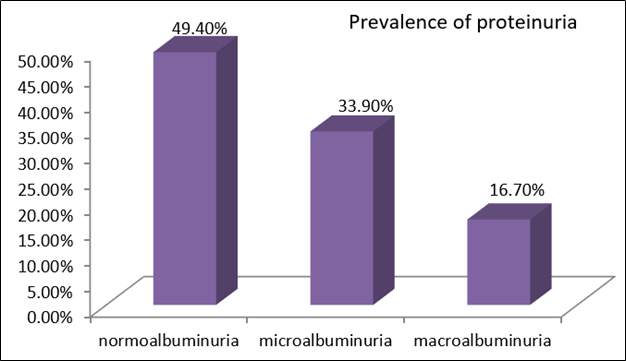
Among the 360 patients evaluated 178 (49.4%) were normoalbuminuric, 122 (33.9%) were microalbuminuric and 60 (16.7%) were macroalbuminuric.
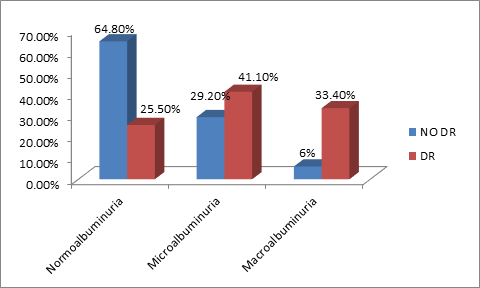
It was found that the prevalence of diabetic retinopathy was more among those with microalbuminuria (41.1%) and macroalbuminuria (33.4%) when compared to those with normoalbuminuria (25.5%).
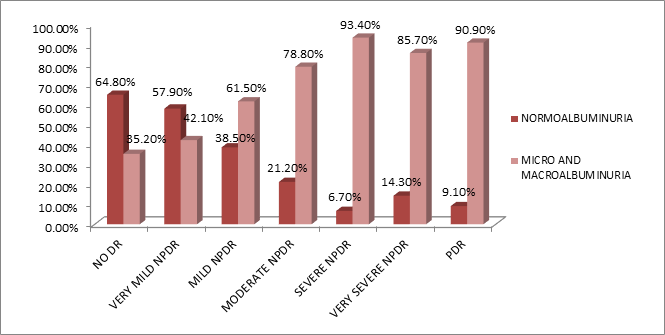
Among the 360 patients studied it was found that Proliferative diabetic retinopathy was seen in 22 patients. Remaining 338 patients did not have proliferative diabetic retinopathy (no DR in 219 patients, very mild NPDR in 19, mild NPDR in 26, moderate NPDR in 52, severe NPDR in 15 and very sever NPDR in 7).
Among those who had proliferative diabetic retinopathy 2 patients had normoalbuminuria (9.1%), remaining 20 patients (90.90%) had abnormal proteinuria (31.8% had microalbuminuria and 59.1% had macroalbuminuria).
Discussion
When compared to those with normoalbuminuria, subjects with microalbuminuria or macroalbuminuria were found to be more prone for the development of diabetic retinopathy. Therefore the presence of microalbuminuria can be considered as a marker to estimate the risk of the development and the progression of proliferative diabetic retinopathy. It does not only indicate a kidney disease, but is a secondary and indirect effect of a distant disease process on the kidney physiology.
In our present study we got a statistically significant association between diabetic retinopathy and proteinuria. In this study the prevalence of micro and macroalbuminuria was 33.9% and 16.7% respectively. 58(41.1%) subjects had urine microalbuminuria and 47(33.3%) subjects had macroalbuminuria among those with retinopathy compared to 64(29.2%) subjects having microalbuminuria and 13(5.9%) subjects having macroalbuminuria among those who had no diabetic retinopathy. Among those with microalbuminuria 8(42.1%) had very mild NPDR, 13(50%) had Mild NPDR, 23(44.2%) had moderate NPDR, 7(46.7%) had severe NPDR, 7(31.8%) had PDR. Whereas in those with macroalbuminuria very mild NPDR was seen in 0%, mild NPDR in 3(11.5%), moderate NPDR in 18(34.6%), severe NPDR in 7(46.7%), very sever NPDR in 6(85.7%), PDR in 13(59.1%). In a study conducted by Masoud R et al the prevalence of microalbuminuria and macroalbuminuria was found to be 25.9% and 14.5% respectively. In their study also they got a statistically significant association between various grades of diabetic retinopathy and urine albuminuria.[8] According to their study the prevalence of various grades of retinopathy among those with microalbuminuria was grade 1 retinopathy in 27(18.9%) subjects, grade 2 in 24(16.8%), grade 3 in 4(2.8%), grade 4 in 7(4.9%) whereas in those with macroalbuminuria grade 1 was seen in 21(26.3%), grade 2 in 19(23.8%), grade 3 in 9(11.3%), grade 4 in 14(17.5%). In literature there are various studies that were carried out to determine the association between the prevalence of diabetic retinopathy and microalbuminuria in Type 2 diabetes. All these studies yielded different rates ranging between 16 to 53.4% for retinopathy.[9], [10], [11]
The prevalence of albuminuria was found to differ among different studies. This variation could be because of the differences in the measurement methods that was used in various studies; variation in the control of the blood sugar levels and the differences in the population or races studied. The method that was used to measurethe microalbuminuria also may have a significant influence on the difference in the frequency of microalbuminuria. In our present study immunoturbidity method was used to measure the urine microalbumin level.
Chen H et al. in their study found that the frequency of diabetic retinopathy increases with the presence of microalbuminuria.[12] There are however few studies that oppose such a relationship. In a study conducted by Erasmus et al. they found that microalbuminuria may not predict retinopathy and they concluded that it occurs independently from either because of poor glycemic control or due to elevated levels of blood pressure.[13]
In our study we found that frequency of diabetic retinopathy increased with presence of microalbuminuria. The common mechanism that is involved in the tissue damage in both retinopathy and nephropathy could explain this association. Further studies are however required for the better knowledge and understanding of the relationship between urine microalbuminuria and diabetic retinopathy. A more clearer understanding about the association between retinopathy and microalbuminuria, will be very useful to have a better knowledge about the pathophysiology of the various microvascular complications caused as a result of diabetes mellitus.
Conclusion
The prevalence of urine albuminuria in Type 2 diabetics was significant and it may be considered as a risk factor for the presence and the severity of diabetic retinopathy. Therefore, diabetic patients with abnormal levels of microalbuminuria will definitetly benefit if they could get a more regular ophthalmic follow-ups. This will help in a more early recognition of diabetic retinopathy changes. The healthcare providers could pay more attention to the relationship between retinopathy and nephropathy in order to further optimize the frequency of screening for diabetic retinopathy in patients with type 2 diabetes.
Source of Funding
None.
Conflict of Interest
None.
References
- A Ramachandran. Socio-economic burden of diabetes in India. J Assoc Physicians India 2007. [Google Scholar]
- R P Maurya. Diabetic retinopathy :My brief synopsis. Ind J Clin Exp Ophth 2015. [Google Scholar]
- E Sobngwi, J C Mbanya, E N Moukouri, K B Ngu. Microalbuminuria and retinopathy in a diabetic population of Cameroon. Diabetes Res Clin Pract 1999. [Google Scholar]
- . Prevalence of small vessel and large vessel disease in diabetic patients from 14 centres. The World Health Organisation Multinational Study of Vascular Disease in Diabetics. Diabetes Drafting Group. Diabetologia 1985. [Google Scholar]
- T Deckert, H Yokoyama, E Mathiesen, B Ronn, T Jensen, B Feldt-Rasmussen. Cohort study of predictive value of urinary albumin excretion for atherosclerotic vascular disease in patients with insulin dependent diabetes. BMJ 1996. [Google Scholar]
- R Retnakaran, C A Cull, K I Thorne, A I Adler, R R Holman, . Risk Factors for Renal Dysfunction in Type 2 Diabetes: U.K. Prospective Diabetes Study 74. Diabetes 2006. [Google Scholar]
- P K Rani, R Raman, A Gupta, S Pal, V Kulothungan, T Sharma. Albuminuria and Diabetic Retinopathy in Type 2 Diabetes Mellitus Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study (SN-DREAMS, report 12). Diabetol Metab Syndr 2011. [Google Scholar] [Crossref]
- M R Manaviat, M Afkhami, M R Shoja. Retinopathy and microalbuminuria in type II diabetic patients. BMC Ophthalmol 2004. [Google Scholar]
- W T Cade. Diabetes-Related Microvascular and Macrovascular Diseases in the Physical Therapy Setting. Phys Ther 2008. [Google Scholar]
- . UK Prospective Diabetes Study (UKPDS). VIII. Study design, progress and performance. Diabetologia 1991. [Google Scholar]
- C Weyer, C Bogardus, D M Mott, R E Pratley. The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J Clin Investigation 1999. [Google Scholar]
- H Chen, Z Zheng, Y Huang, K Guo, J Lu, L Zhang. A microalbuminuria threshold to predict the risk for the development of diabetic retinopathy in type 2 diabetes mellitus patients. PloS One 2012. [Google Scholar]
- R T Erasmus, G Oyeyinka, A Arije. Microalbuminuria in non-insulin-dependent (type 2) Nigerian diabetics: relation to glycaemic control, blood pressure and retinopathy.. Postgraduate Med J 1992. [Google Scholar]
