- Visibility 221 Views
- Downloads 46 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2020.086
-
CrossMark
- Citation
A clinical study of patients with optic neuritis in a tertiary eyecare centre
- Author Details:
-
Anuradha A
-
Priyam Gupta *
-
Vidyadevi M
Abstract
Purpose: To evaluate the clinical profile and visual outcome of optic neuritis patients presenting to a tertiary eyecare centre.
Materials and Methods: It is a retrospective hospital-based study carried out over a period 5 years between 2013 to 2018 in a tertiary eyecare centre in South India. Case records of 20 patients diagnosed and treated for optic neuritis were evaluated based on clinical profile, type of presentation and visual outcome.
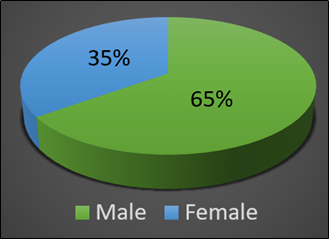
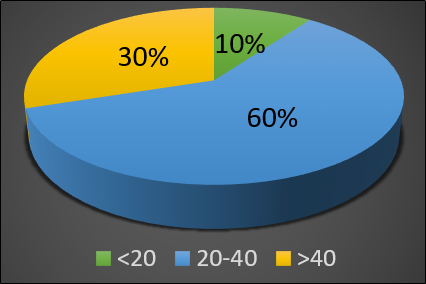
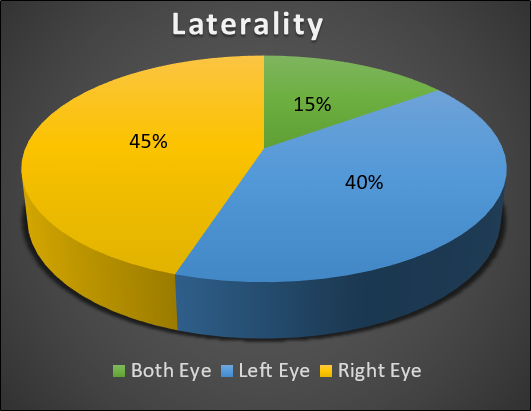
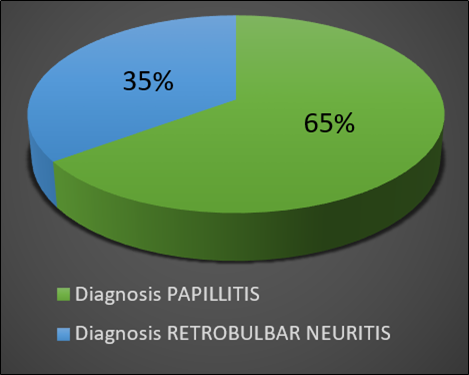
Results: Patients had a mean age was 34.7±13.5 years. 60% presented in age group of 20-40years. Male preponderance was seen (65% of cases). Papillitis (65% of eyes) was more common than retrobulbar neuritis (35% of eyes). Unilateral involvement was seen in 85% of cases with Bilateral presentation seen in only 15% cases. Baseline visual acuity in 10(43%) patients was in the range of Counting fingers to <6/60, 3(13%) patients had vision>= 6/60, 5(22%) patients had Hand movements positive and 5(22%) had Perception of light positive. Periocular pain was seen in 8(40%) of the cases. 13(56%) patients had defective colour vision. 16(70%) patients had Grade 3-4 RAPD while the remaining had grade 1-2 RAPD. One patient was diagnosed with multiple sclerosis (MS). Recurrence was seen in 1 patient (5%). After treatment with 3 doses of 1gm IV Methylprednisolone 15 patients (74% of eyes) showed improvement in vision, 7 eyes (35%) had improvement in colour vision, 4 eyes (20%) had improvement in pupillary reaction after 3 doses of IV Methylprednisolone.
Conclusion: Optic neuritis is idiopathic in nature. Papillitis is the commonest presentation when compared to Retrobulbar neuritis.
Introduction
Optic neuritis (ON) is an acute inflammatory disorder of the optic nerve. It presents as sudden onset diminution of vision and may be unilateral or bilateral with or without associated periocular pain.[1], [2] As a rule most cases present between 15-45 years of age.[3], [4] Clinically patients present with decreased visual acuity, relative afferent pupillary defect, decreased contrast sensitivity and dyschromatopsia. Most cases are idiopathic in nature. However, in the western countries Multiple sclerosis is most common etiology.[4] Our hospital being the regional institute of the state has patient input from all over the state being referred by other hospitals. This study was done to examine and evaluate the clinical profile and visual outcome of optic neuritis (ON) patients presenting to our hospital.
Materials and Methods
This is a retrospective study which was conducted at a tertiary eye care centre, in patients diagnosed with optic neuritis. Records of 20 consecutive patients with Optic neuritis were evaluated from the period of 2013 to 2018.
Optic neuritis was diagnosed on basis of history of sudden onset, unilateral or bilateral loss of vision, with or without associated pain less than 4 weeks duration. History of any previous attack and history of any other neurological symptoms were noted. Clinical examination included visual acuity testing by Snellen’s chart, presence of relative afferent pupillary defect, dyschromatopsia and normal or swollen optic disc on fundus examination. Full Blood Picture, Erythrocyte Sedimentation Rate (ESR), Antinuclear Antibody (ANA), Venereal Disease Research Laboratory (VDRL), Rheumatoid Factor (RhF), Mantoux test, chest X-ray and Magnetic Resonance Imaging (MRI) of the brain/orbit to know underlying aetiology. Other Investigations included Humphreys visual field wherever possible and visual evoked response.
Other optic neuropathies, such as ischemic, infective, traumatic, toxic, hereditary and compressive were excluded from the study. Patients under the age of 15 were excluded from the study.
For all patients 1gm Methylprednisolone in 200ml of 5% dextrose solution was given intravenously over 30 min for three consecutive days after obtaining physician clearance and ruling out systemic contraindications. Improvement in Visual acuity, pupillary reaction, colour vision was recorded every day for three days. Results were documented at end of three days. Analysis included descriptive data of demographic profile, clinical presentation, and visual outcome.
Results
Total of 20 patients with Optic neuritis were evaluated
Male predominance was seen in our study with 13(65%) males, and 7(35%) females. ([Figure 1])
12(60%) of affected individuals were in 20-40years age group, 2(10%) were below 20 years and 6(30%) above 40 years. ([Figure 2])
The mean age group of the study population was 34.7±13.5 years
3(15%) patients had both eyes affected, 8(40%) had optic neuritis in left eye and 9(45%) had optic neuritis in right eye. ([Figure 3])
15(65%) eyes had Papillitis, while 8(35%) had Retrobulbar Neuritis. ([Figure 4])
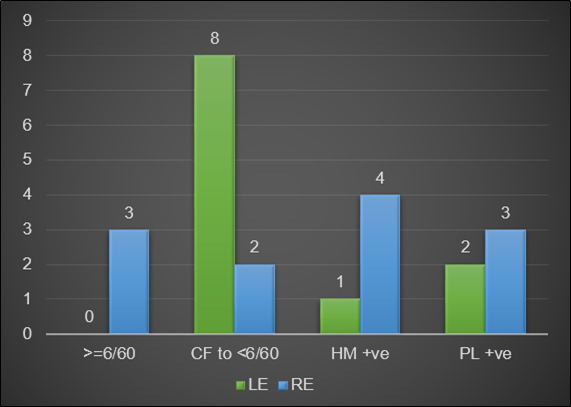
Initial vision on presentation were as follows: 3(13%) eyes had vision >= 6/60, 10(43%) eyes had in range of CF to <6/60, 5(22%) eyes had Hand movements positive and 5(22%) eyes had Perception of light positive. ([Figure 5])
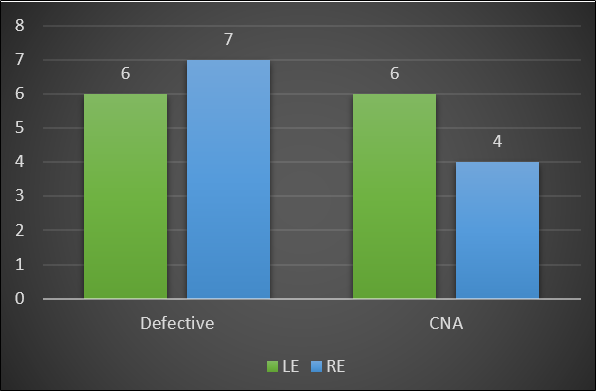
13(56%) eyes had defective colour vision, while in 10(44%) eyes it could not be determined due to poor vision([Figure 6])
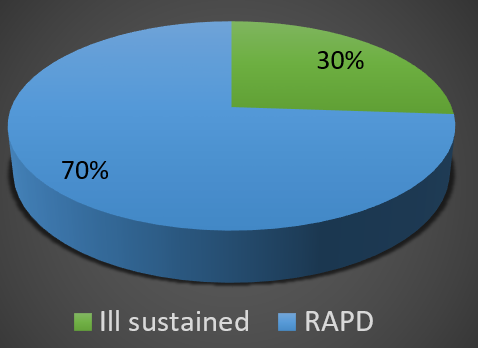
7(30%) eyes presented with Grade 1-2 RAPD or ill sustained pupillary reaction and 16(70%) eyes had grade 3-4 RAPD pupillary reaction ([Figure 7])
Results of the hemogram, total and differential white blood count; erythrocyte sedimentation rate, chest X ray, Mantoux test, serology for syphilis, toxoplasmosis and toxocariasis were normal in all cases.
16 eyes (70%) showed improvement in vision after treatment with 3 doses of IV Methylprednisolone. ([Table 1])
| Affected Eye | Initial Vision | Final Vision | Improved? | ||
| RE | LE | RE | LE | ||
| BE | 6/24 | CF 1MT | 6/24 | 6/24 | One Eye |
| LE | CF CF | CF 2MT | Yes | ||
| RE | CF 1/2MT | CF 3MT | Yes | ||
| LE | CF CF | CF 1MT | Yes | ||
| LE | CF 1MT | CF 3MT | Yes | ||
| RE | PL +ve | CF 3MT | Yes | ||
| BE | PL +ve | PL +ve | PL +ve | PL +ve | No |
| RE | HM +ve | 6/60 | Yes | ||
| LE | CF CF | CF CF | No | ||
| LE | PL +ve | CF CF | Yes | ||
| RE | HM +ve | CF 3MT | Yes | ||
| LE | CF 1/2MT | CF 1/2MT | No | ||
| RE | 6/36 | 6/18 | Yes | ||
| RE | 6/60 | 6/60 | No | ||
| LE | CF CF | CF 3MT | Yes | ||
| LE | CF CF | CF CF | No | ||
| RE /OLD LE | HM +ve | 6/6 | 6/12 | 6/6 | Yes |
| RE | CF 2MT | CF 5MT | Yes | ||
| BE | HM +ve | HM +ve | CF 3MT | CF 3MT | Yes |
| RE | PL +ve | CF2MT | Yes |
6 eyes (26%) had improvement in colour vision after 3 doses of IV Methylprednisolone. ([Table 2])
| Affected Eye | Colour Vision (Initial) | Colour Vision (After Treatment) | Improved? | ||
| RE | LE | RE | LE | ||
| BE | defective | defective | defective | wnl | One eye |
| LE | wnl | CNA | wnl | CNA | No |
| RE | defective | wnl | wnl | wnl | Yes |
| LE | wnl | defective | wnl | defective | No |
| LE | wnl | defective | wnl | defective | No |
| RE | CNA | wnl | CNA | wnl | No |
| BE | CNA | CNA | CNA | CNA | No |
| RE | CNA | wnl | wnl | wnl | Yes |
| LE | wnl | CNA | wnl | CNA | No |
| LE | wnl | CNA | wnl | wnl | Yes |
| RE | CNA | wnl | CNA | wnl | No |
| LE | wnl | defective | wnl | defective | No |
| RE | defective | wnl | wnl | wnl | Yes |
| RE | defective | wnl | defective | wnl | No |
| LE | wnl | defective | wnl | wnl | Yes |
| LE | wnl | defective | wnl | defective | No |
| RE /OLD LE | CNA | wnl | wnl | wnl | No |
| RE | defective | wnl | Defective | wnl | No |
| BE | defective | defective | defective | defective | No |
| RE | CNA | wnl | defective | wnl | No |
Eyes (17% had improvement in pupillary reaction ([Table 3])
| Affected Eye | Pupil (Initial) | Pupil (After Treatment) | Improved? | ||
| RE | LE | RE | LE | ||
| BE | Ill sustained | Ill sustained | Ill sustained | Ill sustained | No |
| LE | wnl | RAPD | wnl | Ill sustained | Yes |
| RE | RAPD | wnl | RAPD | wnl | No |
| LE | wnl | RAPD | wnl | RAPD | No |
| LE | wnl | RAPD | wnl | RAPD | No |
| RE | RAPD | wnl | RAPD | wnl | No |
| BE | Ill sustained | Ill sustained | Ill sustained | Ill sustained | No |
| RE | RAPD | wnl | wnl | wnl | Yes |
| LE | wnl | RAPD | wnl | RAPD | No |
| LE | wnl | RAPD | wnl | RAPD | No |
| RE | Ill sustained | wnl | Ill sustained | wnl | No |
| LE | wnl | RAPD | wnl | RAPD | No |
| RE | RAPD | wnl | RAPD | wnl | No |
| RE | RAPD | wnl | RAPD | wnl | No |
| LE | wnl | RAPD | wnl | RAPD | No |
| LE | wnl | RAPD | wnl | RAPD | No |
| RE /OLD LE | RAPD | wnl | wnl | wnl | Yes |
| RE | RAPD | wnl | RAPD | wnl | No |
| BE | Ill sustained | Ill sustained | Ill sustained | Ill sustained | No |
| RE | RAPD | wnl | Ill sustained | wnl | Yes |
Discussion
Optic neuritis is an acute inflammatory disorder of the optic nerve. It is characterised by sudden onset unilateral or bilateral loss of vision, often accompanied with peri-ocular pain.[2]
Most cases are seen between 15-45 years of age.[3], [4]
30-75 % are idiopathic in nature.[2], [3] In the West however, the commonest single cause of optic neuritis is Multiple Sclerosis and data suggests that at least 50% of patients with Optic Neuritis will eventually develop Multiple Sclerosis.[1], [2], [4]
Various other underlying causes of Optic Neuritis include viral infections, granulomatous infections such as tuberculosis, syphilis, Lyme disease or cryptococcal meningitis and autoimmune diseases such as SLE, Wegner’s Granulomatosis or sarcoidosis. Contagious spread of inflammation from orbit, meninges and sinuses as well as intraocular inflammation involving retina, uvea, and sclera is also known to present as the inflammation of optic nerve.[2]
Clinically, patients present with decreased visual acuity, relative afferent pupillary defect, decreased contrast sensitivity and dyschromatopsia.
Indian Studies by Saxena R,[1] Jain IS[4] concluded the mean age of presentation was 27.6 ± 8.8 years and 20-40 years respectively. Studies done by Shatriah I[3] on Malaysian population and by Lim S A on Singaporean[5] population concluded majority (26.9% and 58.2% respectively) of patients were between 21-30years and 21-40years. Studies in Japan suggested 36.3years as mean age group.[6] These results are consistent with results from our study, in which majority of patients were in the 20-40year age group, with a mean age group of 34.7±13.5 years.
Various studies showed a female preponderance.[1], [2], [3], [5], [6] However, in our study we found a male preponderance, which was also reported by Wang et al[7] and Jain et al,[4] Tandon R et al[8] in their studies.
Unilateral involvement is more common when compared to bilateral involvement.[1], [3], [4], [8] In adult’s simultaneous bilateral acute optic neuritis has been considered rare particularly in individuals without known systemic inflammatory or autoimmune disorders.[9], [10]
Bilateral optic neuritis is usually thought to affect children, often following a viral syndrome, and is not typically associated with subsequent multiple sclerosis. In our study 85% of cases were unilateral.
Pain in case of optic neuritis is thought to be due to traction of the inflamed nerve by the rectus muscles or related to the inflammation or swelling in the adjacent meninges or sheaths of the optic nerve.[4] The infrequent pain in few cases can be explained on the basis that the inflammation is in the anterior part of the optic nerve.
In our study 8 (40%) patients presented with pain. Pain on ocular movement was observed in varying percentages of patients in different studies 92.2% [2] 31.7%.[3] The Optic Neuritis Treatment Trial reported 92% of patients experienced pain. 56% of the patients Studied by Wakakura M et al[6] in Japan reported ocular or periocular pain and more than 40% of patients in a Chinese studies had symptoms of pain during the attack.[11], [12]
Vision loss in Optic neuritis reaches its maximum deficit over 1–7 days and recovery is significant regardless of the treatment.[9]
In our study majority of patients had vision in range of 6/60 to Counting fingers at presentation. Studies by Shatriah I3 on Malaysian population showed that 73.3% of 41 involved eyes had visual acuity equal to 6/60 or worse on presentation. Studies by Saxena R[2] showed 92 out of 99 eyes (93%) presenting with VA <20/40 and 37 eyes (37.3% of eyes) had VA <20/200 and studies by Jain IS4 showed 51 (75%) eyes with visual acuity reduced to Counting finger less than 1 meter at the onset.
On fundoscopy Papillitis was seen more common than retrobulbar neuritis.[1], [2], [3], [4], [8]
The most common finding on visual field observed by Shatriah I.[3] was a paracentral scotoma. Wakakura[6] found centroceacal defect in 12.5% of patients while 37% showed a diffuse depression. Diffuse depression was documented as the highest by Lim et al,[5] Jain et al,[4] Chang YC.[12] In our study, in patients in whom automated perimetry was possible a majority of patient showed a diffuse depression. However, automated perimetry could not be done in all cases due to poor vision, which is a limitation in our study.
All patients had defective colour vision and contrast sensitivity at the time of presentation in the study by Foroozan, R et al.[13] In our case 56% eyes had impaired colour vision and in the rest it could not be assessed due to poor vision.
MRI was not possible in all cases due to financial constraints in our study. Previous Indian studies showed multiple sclerosis in 37.5%,[1] 24.1%,[2] 7.14%,[4] 2.5%[8] of their patients. 3.2% developed multiple sclerosis in the Malaysian population[3] and 5.6% in the Japanese patient. Lim et al[5] reported 25.5% being diagnosed with Multiple sclerosis. We acknowledge that there is a possibility of underestimation of MS in our study given the fact that MRI was not performed in all cases; however, other reports from the south eastern region also show low incidence of MS in the population from this part of the World.[1]
Studies by Saxena R showed a recurrence rate of Optic neuritis as 16%[1] and 9.5% in studies by Jain IS.[4] A 29.1% recurrence rate was documented in Singaporean patients,[5] 28.0% in the ONTT, while Chang et al observed a higher percentage of recurrence.[12] In our study a single case of recurrence of optic neuritis was seen.
All adult patients were treated with intravenous methylprednisolone and oral corticosteroid as recommended by the Optic Neuritis Treatment Trial.[3] The Optic Neuritis Treatment Trial showed that high-dose intravenous methylprednisolone followed by oral prednisone accelerated visual recovery but did not improve the 6-month or 1-year visual outcome compared with placebo, whereas treatment with oral prednisone alone did not improve the outcome and was associated with an increased rate of recurrences of optic neuritis. An unexpected finding was that those who received intravenous corticosteroids followed by oral corticosteroids had a temporarily reduced risk of development of a second demyelinating event consistent with MS compared with subjects who received oral placebo or treatment with oral corticosteroids only. [7], [8]
In our study, 16 eyes (70%) showed improvement in vision, 6 eyes (26%) had improvement in colour vision and 4 eyes (17%) had improvement in pupillary reaction after 3 doses of IV Methylprednisolone. Intravenous methylprednisolone is considered the standard treatment to enhance the recovery of visual function in optic neuritis, In a study done by Sethi H results where patients were treated with dexamethasone instead of methylprednisolone due to financial constraints showed Statistically significant improvement began within 24 hours of administering IV dexamethasone, for distance (P = P = 0.006) Colour vision and contrast sensitivity showed statistically significant improvement after 3 days (P = P = 0.013 for contrast sensitivity). RAPD and visual fields were slower to recover. Statistically significant improvement was seen by 1 month (P = 0.005).[8]
Conclusion
The majority of Optic Neuritis attacks were unilateral, in males, in the age group of 20-40years with visual acuity of 6/60 or worse at presentation. Optic neuritis is idiopathic in nature and Papillitis is the commonest type of Optic neuritis.
Source of Funding
None.
Conflict of Interest
None.
References
- Saxena R, Phuljhele S, Menon V, Sharma P, Sinha A, Gadaginamath S. Clinical profile and short-term outcomes of optic neuritis patients in India. Indian J Ophthalmol. 2014;62(3). [Google Scholar]
- Saxena R, Phuljhele S, Menon V, Gadaginamath S. Profile of Optic Neuritis Patients in India. Neuro Ophthalmol Session. 2010. [Google Scholar]
- Shatriah I, Hitam WW, Nor-Idahriani M, Jakiyah D, Zunaina E. Clinical profile and aetiology of optic neuritis in Hospital Universiti Sains Malaysia--5 years review. Med J Malays. 2012;67(2):1-7. [Google Scholar]
- Jain IS, Munjal VP, Dhir SP, Gangwar DN. Profile of optic neuritis in Chandigarh and surrounding areas. Indian J Ophthalmol. 1980;28:195-200. [Google Scholar]
- Lim S, Goh K, Tow S, Fu E, Wong T, Seah A. Optic neuritis in Singapore. Singapore Med J. 2008;49(9):667-71. [Google Scholar]
- Wakakura M. Baseline Features of Idiopathic Optic Neuritis as Determined by a Multicenter Treatment Trial in Japan. Jpn J Ophthalmol. 1999;43(2):127-32. [Google Scholar]
- Beck RW, Gal RL. Treatment of Acute Optic Neuritis. Arch Ophthalmol. 2008;126(7):994-5. [Google Scholar]
- Tandon R, Sethi HS, Menon V, Sharma P, Khokhar S. Visual outcome after intravenous dexamethasone therapy for idiopathic optic neuritis in an Indian population: A clinical case series. Indian J Ophthalmol. 2006;54(3):177-83. [Google Scholar]
- Cruz Jdl. Clinical profile of simultaneous bilateral optic neuritis in adults. Br J Ophthalmol. 2006;90(5):551-4. [Google Scholar]
- Lana-Peixoto MA, Andrade GCd. The clinical profile of childhood optic neuritis. Arq de Neuro-Psiquiatria. 2001;59(2B):311-7. [Google Scholar]
- Du Y, Yang J, Li JJ. Unilateral optic neuritis in a Chinese population in three centers. J Clin Neurosci. 2011;18:902-4. [Google Scholar]
- Chang YC, Wu WC, Tsai RK. Prognosis of Taiwanese patients with isolated optic neuritis after intravenous methylprednisolone pulse therapy. J Formos Med Assoc. 2007;106:656-63. [Google Scholar]
- Foroozan R, Buono LM, Savino PJ, Sergott RC. Acute demyelinating optic neuritis. Curr Opin Ophthalmol. 2002;13(6):375-80. [Google Scholar]
How to Cite This Article
Vancouver
A A, Gupta P, M V. A clinical study of patients with optic neuritis in a tertiary eyecare centre [Internet]. Indian J Clin Exp Ophthalmol. 2020 [cited 2025 Oct 20];6(3):400-405. Available from: https://doi.org/10.18231/j.ijceo.2020.086
APA
A, A., Gupta, P., M, V. (2020). A clinical study of patients with optic neuritis in a tertiary eyecare centre. Indian J Clin Exp Ophthalmol, 6(3), 400-405. https://doi.org/10.18231/j.ijceo.2020.086
MLA
A, Anuradha, Gupta, Priyam, M, Vidyadevi. "A clinical study of patients with optic neuritis in a tertiary eyecare centre." Indian J Clin Exp Ophthalmol, vol. 6, no. 3, 2020, pp. 400-405. https://doi.org/10.18231/j.ijceo.2020.086
Chicago
A, A., Gupta, P., M, V.. "A clinical study of patients with optic neuritis in a tertiary eyecare centre." Indian J Clin Exp Ophthalmol 6, no. 3 (2020): 400-405. https://doi.org/10.18231/j.ijceo.2020.086
