- Visibility 169 Views
- Downloads 14 Downloads
- DOI 10.18231/j.ijceo.2020.055
-
CrossMark
- Citation
Comparision of surgical induced astigmatism between sics superior and sics temporal
- Author Details:
-
Kunjan Patel
-
Vikas Patel *
-
Nikunj Patel
Introduction
Now a day’s cataract surgery is considered as phaco refractive surgery, not to just removal of opaque lens. Without spectacle, Good postoperative vision is must to satisfy demanding people. The concept of surgically induced astigmatism has more focused on a unique dimension, the refractive aspect of cataract surgery.[1]
From centuries cataract surgery has evolved from couching to modern day manual Small Incision Cataract Surgery (SICS) and Phacoemulsification. Phacoemulsification has become the most favored procedure for cataract surgery in developed countries. In India like developing countries, we need faster, cost effective, high volume and machine non dependent technique like manual small incision cataract surgery, to deal larger population. The evolution and refinement of the small incision cataract surgery, just location and direction of the wound can still have significant impact on surgical outcome.
Small incision cataract surgery (SICS) through a sclerocorneal tunnel has come as a boon as it has been demonstrated that smaller the incision, lesser the number of sutures and valvular construction of wound would induce minimal astigmatism.[2]
In small incision cataract surgery (SICS) the most common incision taken is the superior one than temporal site, which is farthest from the visual axis and less likely to affect corneal curvature. The mean surgically induced astigmatic change is 1.75 diopters (D) following a superior surgical approach while, 0.75 D of astigmatism is induced following a temporal surgical approach.
In this context we under took a study designed to determine the significance and effects of various types of incisions like superior scleral incision V/S temporal incision over the postoperative induced astigmatism as well as to select ideal procedure to correct or reduce the existing astigmatism, aiming at emmetropia to fulfill visual demands.
Materials and Methods
This prospective interventional study was conducted in Department of Ophthalmology, Government Medical College, Surat between December 2012 to November 2014.
This is a study of 40 consecutive cases of cataract. Sampling technique was non-probability consecutive sampling. Among 40 cases, group A with 20 cases underwent MSICS with superior scleral incision and group B with 20 cases underwent MSICS with temporal scleral incision. Patients were admitted as in-patients for cataract surgery and they had post operative follow up as outpatient at the same hospital.
All patients were examined and selected for cataract surgery as per standard protocol.
Inclusion criteria
All Patients age> 18 years with age related immature cataract year giving informed written consent with Small Incision None Phaco cataract surgery and IOL implantation done
Uneventful and sutureless cataract surgery.
Exclusion criteria
Dislocated IOL.
IOL implant in traumatic cataract with corneal tear repair
Patients having combined procedure
Patients diagnosed as a case of corneal disease.
Patients having irregular or oblique astigmatism
Previous history of any surgery in same eye
Procedure
Patients fulfilling inclusion and exclusion criteria were included in the study. All the cases were admitted one day before the surgery. Detailed history about symptoms and systemic complaints was taken. Drug history and history of previous ocular surgeries and other relevant aspect was noted. General systemic examination was done to rule out systemic illness and relevant investigations carried out. Patients were explained about the details of the procedure and probable complications in their local language and an informed consent of the patients and their attainders was taken.
In ocular examination proper, anterior segment evaluation was done with slit lamp biomicroscope. Posterior segment was evaluated using both direct and indirect ophthalmoscopy. Visual acuity (both near and distant) was recorded and preoperative refraction was done. Intra ocular pressure was recorded using Non contact tonometer. Lacrimal syringing was done in necessary cases, one day prior to the surgery. Keratometry readings were recorded using Bausch & Lomb Keratometer and A-scan biometry (using Biomedix Echorule II) was done in all cases with SRK II formula and PCIOL power was determined.
Surgical procedures
All surgeries were performed under Peribulbar anesthesia with (6-7cc) anesthesia of Lignocaine 2% with Bupivacaine 0.5% along with Hyaluronidase 5 IU/ml.
Surgeries were performed under sterile and strict aseptic precautions. After preparing the eye for surgery, superior rectus bridle suture was put(in temporal SICS, lateral rectus bridle suture was taken), fornix based conjunctival flap was taken (between 10 o’clock and 2o’clock for superior SICS ,from 7 o’clock to 12o’clock in right eye and from 12 o’clock to 5o’clock in left eye for temporal SICS) down to bare sclera and gentle cautery was done. A straight scleral incision of about 6 mm was placed 2mm behind the limbus using 11 No. B.P blade. The location of incision was superior in group A and temporal in group B. Temporal incision does not differ much from superior incision but needs some modifications of surgical steps. The surgeon needs to sit on the temporal side of the eye to be operated and corresponding shift of operating microscope. Dissection of sclera-corneal tunnel was undertaken with 2.6 crescent blade up to 1mm inside the clear cornea. Side port was made around 3 clock hours away from the main port and anterior capsule was stained with trypan blue in case of mature cataract, viscoelastic was introduced into anterior chamber and continuous curvilinear capsulorrhexis was done through the side port. Anterior chamber entry was done through the main port using 2.8 mm keratome and incision was extended laterally. The internal opening was made 1-2 mm larger than the external opening, thorough hydro dissection was done using 26 gauge cannula and nucleus was prolapsed into the anterior chamber. Delivery of the nucleus done with using vectis. Anterior chamber was maintained throughout the procedure by injecting viscoelastics into anterior chamber. After delivering the nucleus, remaining cortex was aspirated using Simcoe I & A cannula. A posterior chamber PMMA single piece lens of 6 mm (overall 12.5 mm) optics was inserted in the bag and remaining viscoelastic was removed. Anterior chamber was reformed with BSS through side entry and sealed by stromal hydration. Conjunctiva is closed using cautery, Minor intraoperative complications like iris prolapse, difficulty in delivering the nucleus and premature entry and button holing etc were managed accordingly. Any case requiring the suturing of the tunnel or side port was excluded from the study.
Post operative work up
Postoperatively, patients in both the groups were treated with antibiotic-steroid combination
A detailed post operative examination was done on 1st day, 7th day, 2nd week and 6th week postoperatively, anterior segment and posterior segment examination was done and visual acuity was recorded. Keratometery was done using Bausch and Lomb Keratometer and refraction was done on each visit and parameters noted. The follow up lasted for 2 months; patients were finally examined for residual surgically induced astigmatism and final prescription of corrective spectacles given at that time.
Complications in the course were noted and treated accordingly. The results of two series were compared with regard to post-operative astigmatism.
Statistical analysis
Unpaired ‘t’ test was used to compare mean astigmatism induced by the two groups. Results were analyzed as mean, standard deviation and percentages. Analysis of the results was done by paired two tailed t test, chi square test and EPI INFO software. P-value of <0.05 was considered significant.
Observations and Results
In the present study, the majority of the patients who underwent MSICS were in age group of 51-80 years.
| Type of Astigmatism | SI | TI | Total |
| WTR | 4 | 2 | 6 |
| ATR | 3 | 8 | 11 |
| NEUTRAL | 13 | 10 | 23 |
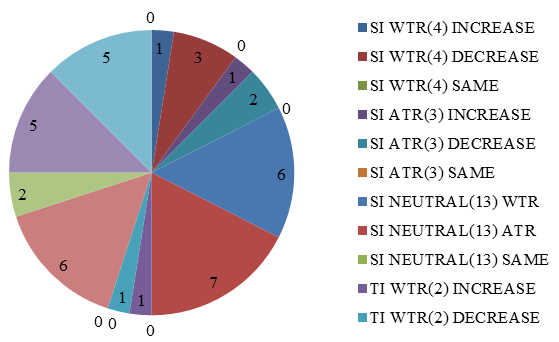
In the present study, there was a gradual decrease in the amount of WTR astigmatism in superior incision group from 1st post-operative day to 42nd post-operative day, whereas in temporal incision group there was gradual increase in the amount of WTR astigmatism from 1st post operative day to 42nd post-operative day.
In present study, in SI group majority (85%) converted to ATR astigmatism and In TI group; majority (60%) patients had WTR astigmatism. After 6 weeks post-operatively, the difference in the amount of ATR astigmatism in both groups was statistically significant (Fischer exact test, p <0.05). Superior incision induced post-operative ATR drift (75%) and temporal incision induced WTR astigmatism (70%). In the present study the visual rehabilitation was similar in both the groups.
It has been observed in the present study that superior incision causes more ATR shift than the WTR, as the incision on the superior meridian causes flattening of the vertical meridian and steepening of the horizontal meridian leading to more ATR shift post-operatively, where as in temporal incision the shift of astigmatism was more towards WTR astigmatism This was due to temporal incision causes flattening of horizontal meridian and steepening of the vertical meridian leading to more WTR shift. This is advantageous as most of the patients in older age will have ATR astigmatism.
In the present study, SI group showed mean SIA more on the first day (1.28 ±0.79D) compared to TI group (1.06±0.649D) which was statistically not significant. (t=0.967, p>0.05).
| Type of SIA | SI | TI | ||
| Mean | SD | Mean | SD | |
| WTR | 1.52 | 0.34 | 0.84 | 0.52 |
After4 weeks, the mean SIA in SI group was 1.64± 0.37D and in TI group the mean SIA was 0.93±0.5396D. After 4 weeks, the difference between two groups was found to be statistically significant (t =3.82, p<0.05).
In the present study, on first post-operative day, The visual acuity pattern is similar in both the groups, Hence, there is no statistical significance (x2=1.464, p>0.05).
The reduced visual acuity on the first day is due to the corneal/eyelid edema, anterior chamber reaction and greater amount of surgically induced astigmatism.
After 6 weeks, improvement in visual acuity in temporal group is better than the SI group, and the difference is statistically significant (x2=13.54, p<0.05). The UCVA was better in TI as compared to SI group. In our study, 65% patients in TI group had visual acuity of ≥ 6/12 while 60% patients in SI group had visual acuity of ≥ 6/12.
The early improvement in visual acuity in TI is due to early stabilization of the astigmatism and better wound healing as compared to the superior incision. Less than 1 D of SIA was seen in 50% patients undergoing superior scleral incision and in 75% patients undergoing temporal scleral incision in our study.
Discussion
In India, according to a recent survey in the Rapid Assessment of Avoidable Blindness (RAAB) study, cataract was responsible for 77.5% of avoidable blindness.[3] Due to economical burden, majority of older people are under cared and neglected. In spite of health care facilities, health system has to go nearer to patients for treatments particularly eye care system. To fulfill these requirements Camps are often conducted to fetch the patients. So, just they choose free camp surgeries, they have equal right to get best uncorrected visual equity as a patient. Manual SICS is considered an alternative to Phacoemulsification which can correct pre operative astigmatism up to certain level and also take care of bulk patients as a time saving technique .
Ferrer-Blasco et al. studied prevalence of corneal astigmatism before cataract surgery and found that; in 13.2% of eyes no corneal astigmatism was present; in 64.4%, corneal astigmatism was between 0.25 and 1.25 diopters (D) and in 22.2%, it was 1.50 D or higher.[4] This finding implies that, when planning a surgery, both the spherical and the astigmatic components should be taken into account to achieve post-operative outcomes as close to emmetropia as possible.
Cornea flattens over any incision and this effect increases as incision approach near the visual axis thus superior incision results in postoperative ATR. This effect in terms of vital gain is beneficial to pre operative WTR case but unfavorable to cases with preoperative ATR. Therefore, the property of cornea to flatten along the incision can be used to flatten steeper horizontal meridian in cases of pre operative ATR astigmatism by placing temporal incision.
Zheng L, Merriam J C, Zaider M (1997) compared that incision size and location effect post-operative astigmatism. Induced astigmatism decreases with wound size, and only the 3 mm temporal incision is astigmatically neutral, the time for visual recovery increases with wound size.[5]
Oshika T, Sugita G, Tanabe T, Tomidokoro A, Amano S (2000) studied 174 eyes of 87 patients, concluded that superior incision induces slightly ATR astigmatism and temporal incision induces slight WTR astigmatism. [6] Similarly, Gokhale N S, Sawhney S shown that the amplitude of surgically induced astigmatism was higher in superior scleral incision than superotemporal scleral incision than in temporal incision in a study of 45 cases of MSICS in Mumbai in 2005.[7]
In a comparative study by RENU et al., a total of 100 eyes were operated for cataract by MSICS. 50 eyes were operated by superior scleral incision and 50 by temporal scleral incision in D Y Patil Hospital Pune in 2012. In study, after 3 months of surgery, out of 50 patients in superior scleral incision group 74% patients had ATR astigmatism and 16% patients had WTR astigmatism whereas in temporal scleral incision group 56 % of the patients had WTR astigmatism and 36 % had ATR astigmatism. The mean surgically induced astigmatism (SIA) in temporal incision group was significantly less than the superior incision group after 3 months postoperatively. They shown that temporal approach MSICS produces less postoperative astigmatism and has manifold advantages.[8]
Temporal incisions may have reduced astigmatic effect because of farther location of temporal limbus from visual axis and an additional effect exerted from eyelid.[9] Incision placement depending on the pre operative steep K readings is helpful in reducing surgically induced astigmatism.
Experience of resident doctors regarding abilities in various steps between SICS-Superior & SICS-Temporal.
In present study, temporal SICS with resident doctors, larger external scleral incision with larger internal opening was required for same grade of cataract due to elliptical cornea compare to SICS superior.
Bridle suture, scleral tunnel construction & capsulorrhexis were difficult which may be due to lack of forehead support. Intraoperative iris prolapse & difficulty in nucleus delivery were due to less tunnel valve effect because of thinner sclera temporally compared to superior part. It is difficult to do conjunctival cauterization in temporal approach surgery at the end.
In respect to difficulties in various surgical steps, SICS -Temporal is a challenging technique to learn and demands skill and patience from surgeons. It was emphasized that most of these limitations overcome with proper training, supervision and experience.
Limitations
The drawback of our study was small sample size, weakness of our study.
Manual sics is not effective to correct higher degree of preoperative astigmatism, toric IOL and peripheral relaxing incision on cornea can be effectively combined with cataract surgery/ phacoemulsification being more favoured in such cases.
Conclusion
Considering modern cataract extraction as Kerato-refractive surgery, post-operative best uncorrected visual acuity is must, it requires closer attention to surgically induced corneal shape alterations, both amount and axis of astigmatism must be given equal importance. In a centre where high volume of cataract surgeries performed and patients don’t afford premium lenses especially government set up, can reduce surgically induced astigmatism by proper selection of incision and give better visual rehabilitation.
Source of Funding
None.
Conflict of Interest
None.
References
- M K Rathore, Sujata Lakhtakia. . Temporal tunnel incision in sics small incision cataract surgery 2010. [Google Scholar]
- K P S Malik, R Goel. . Small incision cataract surgery: an introduction. Manual of small incision cataract surgery. 1st ed 2003. [Google Scholar]
- John Neena, Jose Rachel, Vashist Praveen, Gudlavalleti V. S. Murthy, . Rapid assessment of avoidable blindness in India. PLoS ONE 2008. [Google Scholar]
- Teresa Ferrer-Blasco, Robert Montés-Micó, Sofia C. Peixoto-de-Matos, José M. González-Méijome, Alejandro Cerviño. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg 2009. [Google Scholar]
- L Zheng, J Merriam, M Zaider. Astigmatism and visual recovery after “large incision” extracapsular cataract surgery and “small” incisions for phacoemulsification. Tr Am Ophth Soc 1997. [Google Scholar]
- Tetsuro Oshika, Gentaro Sugita, Tatsuro Tanabe, Atsuo Tomidokoro, Shiro Amano. Regular and irregular astigmatism after superior versus temporal scleral incision cataract surgery13The authors have no commercial or proprietary interest in any of the companies, products, or methods described in this article.. Ophthalmol 2000. [Google Scholar]
- NikhilS Gokhale, Saurabh Sawhney. Reduction in astigmatism in manual small incision cataract surgery through change of incision site. Indian J Ophthalmol 2005. [Google Scholar]
- R M Magdum, A Gahlot, R D Maheshgauri, K Patel. A comparative study of surgically induced astigmatism in superior and temporal scleral incision in manual small incision cataract surgery. National J Med Res 2012. [Google Scholar]
- A T Comez, Y Ozkurt, Michael Goggin. . Surgical correction of astigmatism during cataract surgery. Astigmatism – Optics, Physiology and Management 2012. [Google Scholar]
