- Visibility 127 Views
- Downloads 34 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2020.049
-
CrossMark
- Citation
Sutureless and glue-free pterygium surgery done by residents: Post-operative outcomes
- Author Details:
-
Hardik Kiri
-
Lipa Mohanty *
-
Ajay Purohit
-
Seemal Goyal
Abstract
Purpose: To assess the results of sutureless and glue-free blood clot fixation of conjunctival autograft after primary pterygium excision.
Materials and Methods: A total of 94 eyes of 91 patients were operated by 3 residents. All eyes underwent primary pterygium excision followed by conjunctival autografting. The recipient bed was encouraged to achieve natural haemostasis and blood clot was used as tissue adhesive to secure conjunctival autograft. Graft adherence and positioning was examined after 15 min.
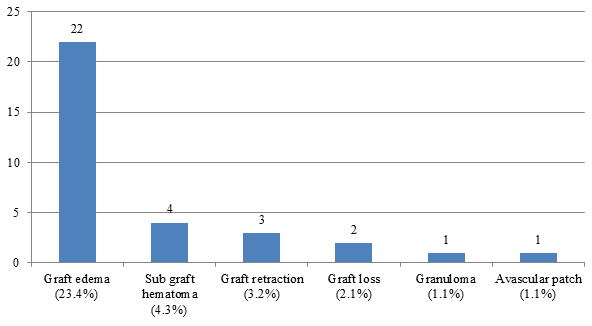
Results: After surgery, out of total 94 eyes (n), graft edema developed in 22 eyes (23.4%), sub graft hematoma in 4 eyes (4.3%), graft loss in 2 eye (2.1%), granuloma formation in 1 eye (1.1%), and avascular patch in 1 eye (1.1%).
Conclusions: Sutureless and glue-free pterygium excision with autologous conjunctival autograft is a simple and safe surgery even in the hands of residents. It provides excellent cosmesis and reasonable patient satisfaction.
Introduction
The training of residents is greatly enhanced by incorporating the six Accreditation Council for Graduate Medical Education(ACGME) elements‑medical knowledge, patient care, interpersonal and communication skills, professionalism, practice‑based learning and improvement, and systems‑based practice.[1] Pterygium excision being an extra ocular surgery can be given to residents in their early training period and practiced under supervision.
The term ‘pterygium’ derived from Pterygos (ancient Greek word meaning wing),[2] is a non-malignant, slow growing, wing shaped proliferation of the fibrovascular tissue, which arises from the subconjuctival tissue, and may extend over the cornea.[3] The main histopathological feature of pterygium is elastotic degeneration of conjunctival collagen.[4] Pterygium can disturb vision by leading to tear film instability, corneal astigmatism or visual axis obscuration. Its presence also causes poor cosmesis. Recurrence rate (ranging from 24 to 89%) has been observed in cases of simple excision of pterygium leaving behind bare sclera.[5]
Pterygium’s prevalence varies from 0.7% to 31% in different geographical regions.[6] Pterygium mainly occurs on the nasal side, but it is not uncommon to encounter bi-headed pterygium in the “pterygium belt” region, located between 30°N and 30°S of the equator.[7]
Glue or sutures are used to fix the conjunctival autograft in order to prevent recurrence. A new technique of using patient’s blood available at the graft bed to fix the graft has been introduced.[8] Sutures and glue being foreign materials are associated with complications such as granuloma formation, infection, chronic inflammation, hypersensitivity reactions or recurrence.[9]
Materials and Methods
Institutional review board approval was obtained. In this retrospective study, data were collected from hospital medical records of a total of 94 eyes of 91 patients operated by 3 residents at a tertiary care hospital of southern Rajasthan during the period of March 2017 to November 2018. 89 nasal, 4 biheaded and 1 temporal pterygium were included in the study.
Patients of all ages and either sex presenting to the OPD of a tertiary care center with primary pterygium were included in study. Patients with recurrent pterygia and other ocular pathology requiring surgical intervention were excluded from the study.
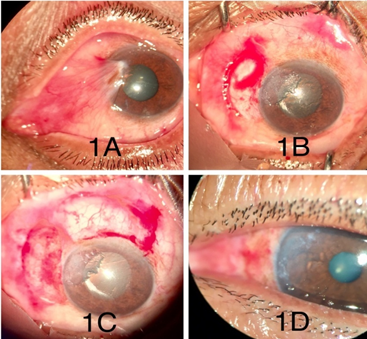
Preoperatively all the patients underwent complete ocular examination of anterior and posterior segment. Patients were examined on days 1,7,14; 1 month, 3 months and 6 months postoperatively. Examination findings of pre and post-operative visits were recorded. Surgical technique ([Figure 1]).
Under all aseptic precautions surgeries were done after peribulbar block anesthesia. Using a toothed forceps Pterygium was avulsed from cornea and then separated from underlying sclera and excised. Subconjunctival pterygium tissue was excised with Westcott scissors. Corneal and limbal scraping was done with crescent knife/ 15 no. blade. A thin film of blood clot was allowed to form over the bare sclera. The size of the defect was measured with castroviejo calipers. 0.5mm oversized graft was taken from the superior limbal conjunctiva devoid of Tenon’s capsule. Then the graft was slid over the bare sclera with limbal edge towards the limbus. A duration of ten minutes was allowed for the graft to settle over the scleral bed. The stabilization of the graft was tested centrally and on edges to ensure firm adherence to the sclera. The eye was patched overnight. Postoperatively, antibiotic-steroid eye drops (Moxifloxacin and Dexamethasone) were prescribed 4 times a day initially and tapered over 4 weeks. Carboxy methyl cellulose eye drops 0.5% were prescribed 4 times a day for 1 month.
Results
94(n) eyes with primary pterygium were operated by 3 residents with suture-less and glue free technique using autologous blood. Retrospective analysis was done. There were 51 male and 40 female patients. No significant intraoperative complications were noted. The following results were obtained post operatively.
Graft edema ([Figure 2]A) was the most common complication noted post operatively in 22 eyes (23.4%). Sub graft hematoma occurred in 4 eyes (4.3%), graft retraction in 3 eyes(3.2%), graft loss in 2 eyes (2.1%), granuloma formation ([Figure 2]C) in 1 eye(1.1%) and avascular patch ([Figure 2]D) in 1 eye(1.1%).
![Post operative complications; A): Graft edema on POD 1; B): edema resolved on POD 7 of same patient; C): Granuloma formation; D): Avascular patch [Arrow])](https://s3-us-west-2.amazonaws.com/typeset-media-server/7a638f29-1c59-4031-b3d8-d55cd043fde7image2.png)
| Complications | Sharma A et al 10 | Rathi G et al 11 | Kulthe S et al 8 | Our study |
| Graft loss | 0 | 1 (2%) | 2(2.5%) | 2(2.1%) |
| Sub graft hematoma | 26(32.5%) | 0 | 0 | 4(4.3%) |
| Granuloma | 0 | 0 | 0 | 1(1.1%) |
| Graft edema | 4(5%) | 2(4%) | 0 | 22(23.4%) |
| Recurrence | 1(1.25%) | 1(2%) | 0 | 0 |
| Avascular patch | 0 | 0 | 0 | 1(1.1%) |
| Graft retraction | 3(3.75%) | 0 | 1(1.2%) | 3(3.2%) |
Discussion
Graft edema and sub graft hematoma were the common complications post operatively. They resolved over a period of 2 weeks without any treatment ([Figure 2]B). In one case granuloma formation was observed which was excised and sent for histopathological examination. Avascular patch was treated by stopping the topical steroid eye drops.
The [Table 1] shows comparison of different studies of suture-less glue free pterygium surgeries. In our study graft edema was found in 22 cases which was high in number as compared with the others.
The major concern of the commercial fibrin glue is the cost and risk of transmitted infection.[9] Thus, in recent practice suture less and glue free limbal conjunctival autograft following pterygium excision has emerged as a safe, effective and economical option for the management of primary pterygium.
Suturing is the most common method of autograft fixation. Its demerits are prolonged operating time, postoperative irritation, buttonholing, suture-related infection and granuloma formation which usually requires a second operation for removal.[12]
Zheng K et al[13] compared pterygium surgery outcomes using conjunctival limbal autograft and other techniques. Recurrence rates after pterygium excision with conjunctival limbal autograft were observed to be lower as compared with the use of bare sclera, bulbar conjunctival autograft, or intraoperative mitomycin C.
Conclusion
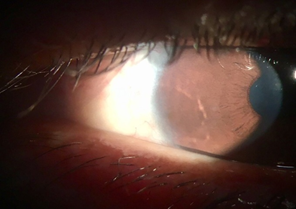
Pterygium excision with conjunctival limbal autograft using autologous blood is a simple, safe and cost effective surgery. It can even be performed by residents with relative ease. It provides excellent cosmesis ([Figure 4]) and reasonable patient satisfaction. Follow up at 6 months was satisfactory with no evidence of recurrence.
Source of Funding
None.
Conflict of Interest
None.
References
- Swanson AG. The genesis of the Coordinating Council on Medical Education and the Liaison Committee on Graduate Medical Education. Bull New York Acad Med. 1974;50(11). [Google Scholar]
- Duke-Elder S, Leigh AG. System of Ophthalmology. . 1965;8:573-85. [Google Scholar]
- Garg A, Toukhy E, Massaralla BA, Moreker S. Surgical and medical management of Pterygium. . 2009. [Google Scholar]
- Spencer WH. . Ophthalmic pathology. An Atlas and textbook. 1985. [Google Scholar]
- Jaros PA, DeLuise VP. Pingueculae and pterygia. Surv Ophthalmol. 1988;33(1):41-9. [Google Scholar]
- Asokan R, Venkatasubbu RS, Velumuri L, Lingam V, George R. Prevalence and associated factors for pterygium and pinguecula in a South Indian population. Ophthalmic Physiol Opt. 2012;32(1):39-44. [Google Scholar]
- Cameron ME. . Pterygium throughout the world. 1965. [Google Scholar]
- Kulthe S, Bhosale A, Patil P, Pandve H. Is the surgical technique of a sutureless and glue-free conjunctivolimbal auto graft after pterygium excision complications free?. Med J Dr. DY Patil Univ. 2015;8(3). [Google Scholar]
- Wit Dd, Athanasiadis I, Sharma A, Moore J. Sutureless and glue-free conjunctival autograft in pterygium surgery: a case series. Eye. 2010;24(9):1474-7. [Google Scholar]
- Sharma A, Raj H, Raina AV. Suture less and glue free limbal conjunctiva autografting following pterygium excision. JK Sci. 2015;17(2):68-72. [Google Scholar]
- Rathi G, Sadhu J, Joshiyara P, Ahir HD, Ganvit SS, Pandya NN. Pterygium surgery: Suture less glue less conjunctival auto grafting. Int J Res Med. 2015;4(1):125-8. [Google Scholar]
- Starck T, Kenyon KR, Serrano F. Conjunctival autograft for primary and recurrent pterygia: surgical technique and problem management. Cornea. 1991;10(3):196-202. [Google Scholar]
- Zheng K, Cai J, Jhanji V, Chen H. Comparison of pterygium recurrence rates after limbal conjunctival autograft transplantation and other techniques: meta-analysis. Cornea. 2012;31(12):1422-7. [Google Scholar]
How to Cite This Article
Vancouver
Kiri H, Mohanty L, Purohit A, Goyal S. Sutureless and glue-free pterygium surgery done by residents: Post-operative outcomes [Internet]. Indian J Clin Exp Ophthalmol. 2020 [cited 2025 Sep 14];6(2):227-230. Available from: https://doi.org/10.18231/j.ijceo.2020.049
APA
Kiri, H., Mohanty, L., Purohit, A., Goyal, S. (2020). Sutureless and glue-free pterygium surgery done by residents: Post-operative outcomes. Indian J Clin Exp Ophthalmol, 6(2), 227-230. https://doi.org/10.18231/j.ijceo.2020.049
MLA
Kiri, Hardik, Mohanty, Lipa, Purohit, Ajay, Goyal, Seemal. "Sutureless and glue-free pterygium surgery done by residents: Post-operative outcomes." Indian J Clin Exp Ophthalmol, vol. 6, no. 2, 2020, pp. 227-230. https://doi.org/10.18231/j.ijceo.2020.049
Chicago
Kiri, H., Mohanty, L., Purohit, A., Goyal, S.. "Sutureless and glue-free pterygium surgery done by residents: Post-operative outcomes." Indian J Clin Exp Ophthalmol 6, no. 2 (2020): 227-230. https://doi.org/10.18231/j.ijceo.2020.049
