- Visibility 59 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijceo.2025.028
-
CrossMark
- Citation
Acute-onset isolated oculomotor nerve palsy due to pituitary apoplexy
Introduction
Pituitary apoplexy (PA) is a vision- and potentially life-threatening condition caused by an acute haemorrhage or infarction within the pituitary adenoma. It is characterised by an array of symptoms that include acute-onset headaches, altered consciousness, vomiting, vision loss, and diplopia.[1] Diplopia has been documented in 6-48% of PA patients[1], [2] due to an abrupt expansion of the pituitary tumour, causing compression on the adjacent cranial nerves (i.e., the third, fourth, and sixth cranial nerves). However, isolated oculomotor/third nerve palsy as a first sign of pituitary apoplexy is rare.[3] We report three cases of pituitary apoplexy that presented as an isolated oculomotor nerve palsy. Consent was taken from all the patients.
Case Series
Case 1
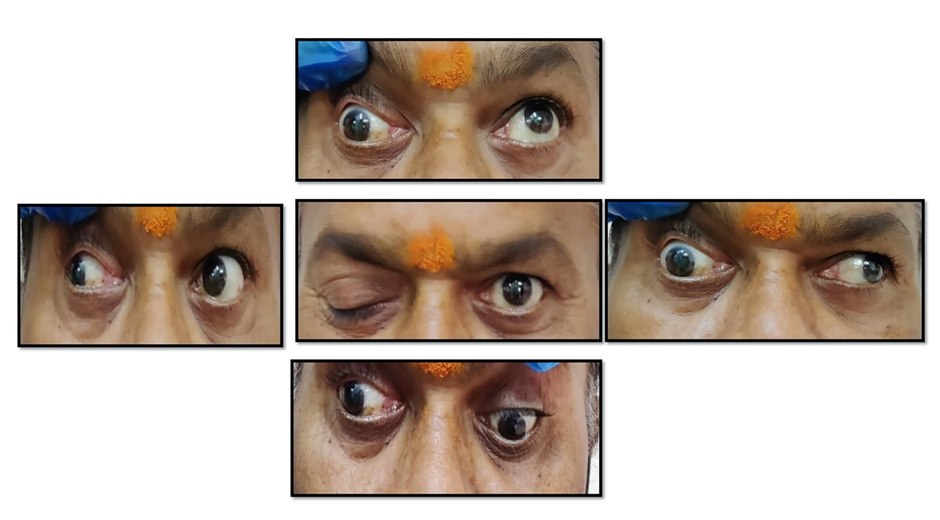
A 53-year-old man who was not diabetic or hypertensive came to our emergency department with a sudden drooping of the right eye upper lid and double vision after elevating that lid for the past two days. He had associated severe headaches and vomiting. He did not give any history of trauma, fever, altered consciousness, weakness of limbs, convulsions, or reduced vision. He was systemically stable at the presentation and had a 15/15 GCS. Both eyes had best-corrected visual acuity (BCVA) of 6/24 and N8, corresponding to senile immature cataracts. Both eye-fundus examinations were normal. Visual field confrontation examination revealed bitemporal hemianopia. On examination, the right eye showed complete ptosis with a -4 limitation of adduction, depression, and elevation ([Figure 1]). Extraocular movements were full in the left eye. The right eye’s pupil measured 5 mm and reacted sluggishly to both direct and consensual light reflexes. The pupil in the left eye measured 3 mm and reacted briskly to direct and consensual reflexes. A ruptured posterior communicating artery aneurysm was suspected as the source of the patient’s severe headache and oculomotor nerve palsy, requiring an emergency CT scan.
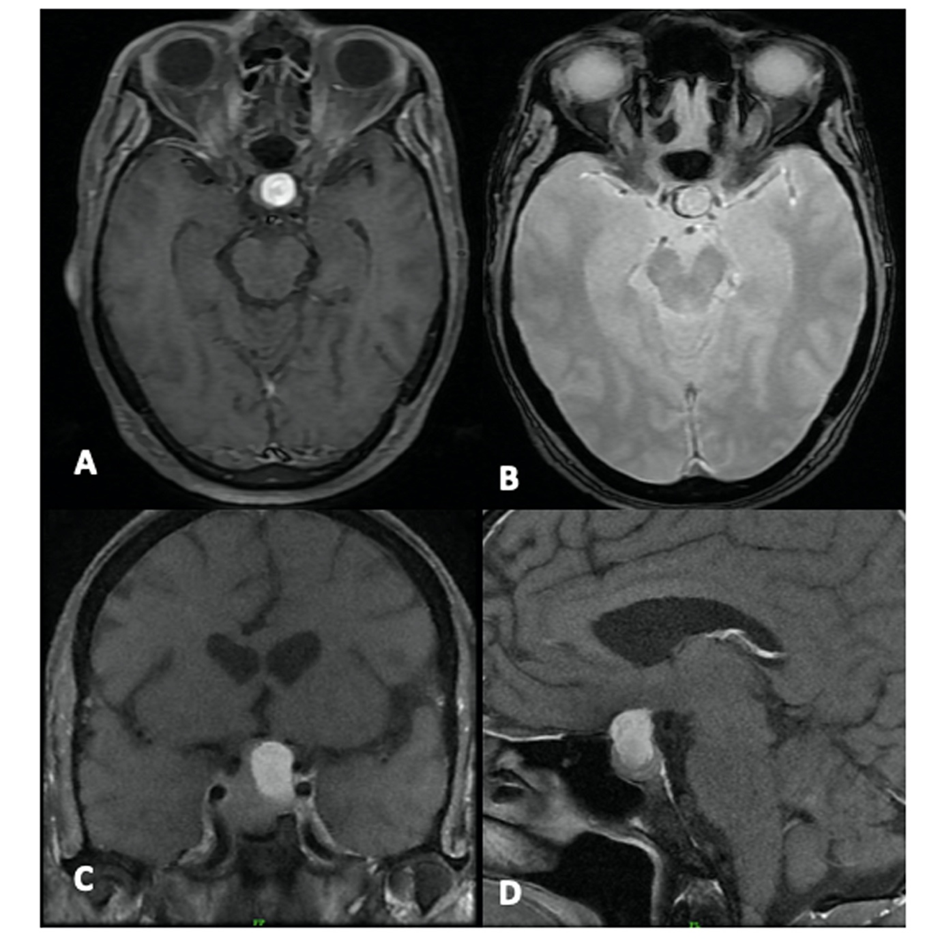
The CT scan showed a mass lesion in the sellar, suprasellar, and parasellar regions. The lesion measured 29 x 28 x 17 mm and had a lobulated and heterogeneously enhancing soft tissue density. There was a peripheral rim of hyperdensity seen on the right side, suggesting a haemorrhage within the tumour ([Figure 2]). A contrast-enhanced magnetic resonance imaging (MRI) of the brain revealed a well-defined, lobulated, and heterogeneous lesion in the sella that extended into the suprasellar area. The lesion was isointense on T1W and mildly hyperintense on T2W/STIR scans, with no diffusion restriction and homogenous moderate enhancement on post-contrast imaging. On GRE T2*WI (gradient recalled echo), a T1/T2 hyperintense area with peripheral blooming was observed, indicating a haemorrhage within the lesion. Superiorly, the lesion abutted and displaced the optic chiasma and pituitary stalk. It encompassed the right internal carotid artery as it expanded laterally into the right cavernous sinus ([Figure 3]). His pre-operative pituitary hormone levels were normal.

He underwent an endoscopic trans-nasal trans-sphenoidal excision of the lesion. During surgery, the tumour appeared greyish, moderately vascular and contained areas of haemorrhage and necrosis. The lesion was almost entirely excised. A histopathological analysis of the tissue revealed a pituitary adenoma with bleeding and necrosis, confirming the diagnosis of apoplexy. His postoperative course was uneventful, with a complete resolution of ptosis and mild mydriasis after one month.
Case 2
A 47-year-old non-diabetic, non-hypertensive man presented with sudden-onset headaches for five days, followed by drooping of the left eyelid for four days and drooping of the right eyelid for a day. The patient was conscious during the examination (GCS: 15/15). His BCVA in the right eye was 6/9; in the left eye, it was CF-1 meter. He had complete ptosis with elevation, adduction, and depression limitations in both eyes. The right eye pupil was 3 mm in size and light-responsive, while the left eye pupil was 4 mm in size and unresponsive. The rest of the anterior segment and fundus findings were normal. Other cranial nerve examinations were normal, with no evidence of sensory or motor impairment.
A plain and contrast brain MRI identified a large mass lesion in the sella, measuring 17x26x28mm. It appeared to be iso-intense on T1 and hyperintense on T2-weighted imaging. After contrast, the lesion showed peripheral enhancement, with a large central non-enhancing area that suggested haemorrhagic components. Laterally, the lesion abutted both cavernous sinuses and partially enclosed both ICAs. Superiorly, the lesion displaced the infundibular stalk and optic chiasm.
Pre-operative electrolytes and pituitary hormone levels were normal. The pituitary tumour was removed via an emergency transcranial excision. Intraoperatively, the lesion appeared greyish and moderately vascular, with multiple areas of haemorrhage and necrosis within the tumour. The lesion was excised entirely. The postoperative period was uneventful. He was discharged on the tenth day following surgery. Following surgery, the right-side oculomotor nerve palsy wholly resolved in one week and the left side in three weeks.
Case 3
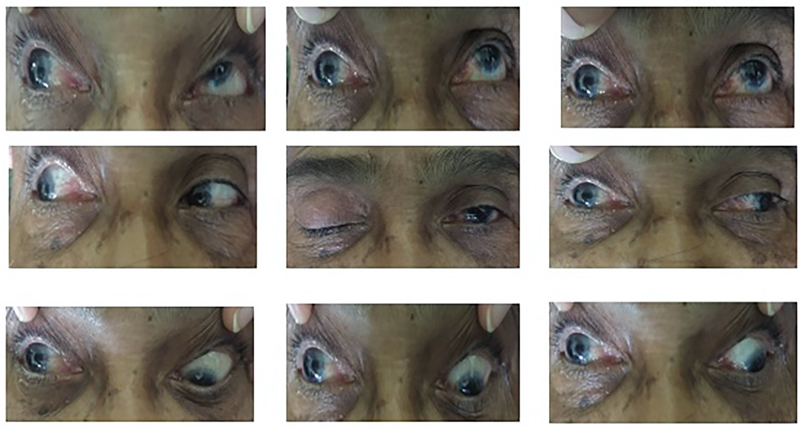
A 56-year-old man who had previously undergone trans-sphenoidal excision of a pituitary macroadenoma four years ago presented with sudden drooping of the right eyelid, double vision, and a mild headache. On admission, he was conscious and systemically stable. In both eyes, his best-corrected vision was 6/9. On the right side, he had severe ptosis. The right eye was down and out, and extraocular movements in adduction, elevation, and depression were restricted ([Figure 4]). His left eye was moving normally. Both the pupils measured 3 mm in diameter and reacted to light. The remaining cranial nerve functions were normal.
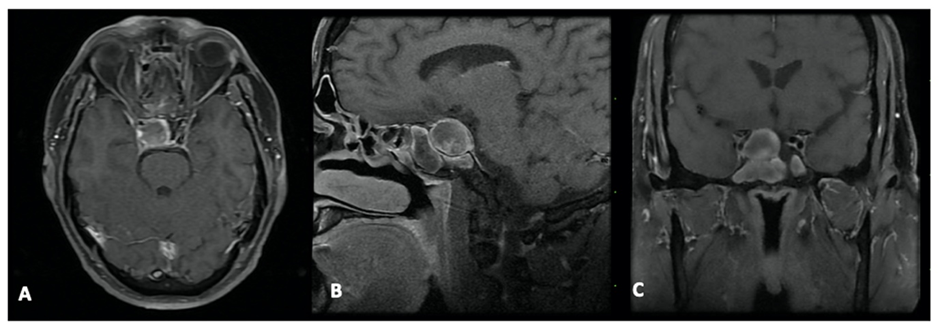
The MRI brain (plain and contrast) revealed a lobulated, heterogeneously enhancing soft tissue lesion (20x22x26 mm) in the sellar region that showed hyperintensity on both T1 and T2-weighted imaging. An area of non-enhancement with blooming on the GRE suggested a haemorrhage within the tumour. The lesion extended into the suprasellar region, compressing the optic chiasma ([Figure 5]). It also spread inferiorly into the sphenoid sinus. It abutted the cavernous sinus laterally and encased sections of the right internal carotid artery. Pre-operative hormone analysis showed hypothyroidism, for which an endocrinology opinion was sought, and hormonal supplements were given. Other pituitary hormones were normal.
Despite being advised to have surgery as soon as possible, the patient experienced a 25-day delay due to the fear and anxiety caused by the COVID-19 outbreak. When the conditions improved, he underwent trans-nasal, trans-sphenoidal excision of the lesion. The pituitary adenoma was removed almost entirely. Histopathology revealed a pituitary adenoma with necrosis consistent with apoplexy. Following surgery, the patient developed meningitis, which was successfully treated. At the 10-day follow-up, the right eye ptosis and extraocular movements were fully recovered. A subsequent MRI of the brain revealed no remaining adenoma.
Discussion
Pituitary apoplexy (PA) is a clinical diagnosis that is usually caused by a haemorrhagic pituitary adenoma, though tumour infarctions can also be the cause.[1] PA is more common in macroadenoma and non-functioning adenomas, which are larger in size at diagnosis due to their non-secretory nature and thus more prone to infarction or haemorrhage.[4] The classic clinical manifestations of PA are acute headaches, nausea, vomiting, hormonal dysfunction, and visual disturbances. Most PA patients develop vision loss or visual field abnormalities secondary to superior tumour enlargement, which compresses the optic nerve or optic chiasm. Diplopia results from the lateral extension of these tumours into the cavernous sinus, which causes multiple cranial nerve palsies.[3], [4], [5], [6] Isolated oculomotor nerve palsy is a rare presenting sign of PA. We describe three patients who presented with sudden oculomotor nerve palsy and were later identified as having PA.
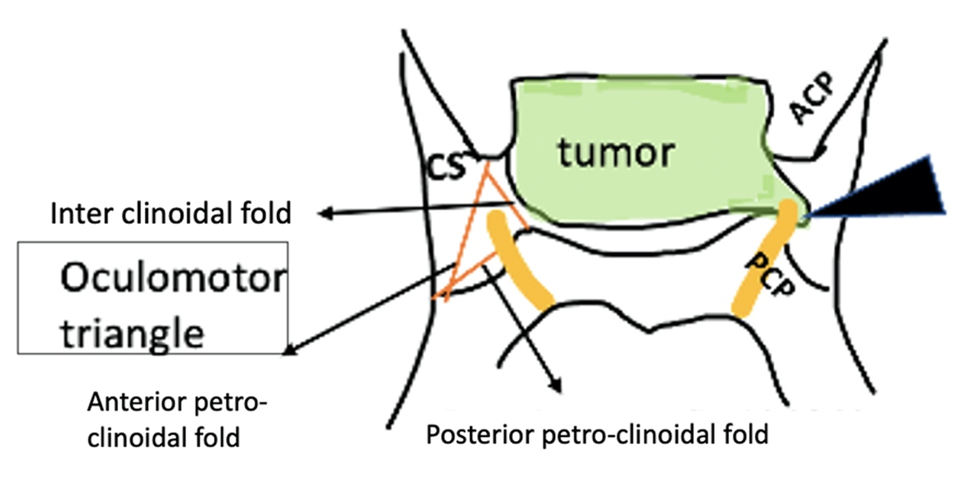
Oculomotor nerve palsy is more common in PA patients than 4th and 6th cranial nerve palsies due to its horizontal location in the same plane as the pituitary gland. The oculomotor nerve passes via a region of dural weakness called the “Oculomotor Triangle (Hakuba’s Triangle),” which is formed by the anterior petroclinoid dural fold, the interclinoid dural fold, and the posterior petroclinoid dural fold. ([Figure 6]). A sudden increase in pituitary pressure caused by an acute haemorrhage or infarction can easily be transmitted to the oculomotor nerve in this triangle.[5] A decrease in the blood flow to the nerve produced by compression of the vasa nervorum from the internal carotid artery can also result in acute oculomotor nerve palsy.[6] The fourth and sixth cranial nerves are less affected as they run via the tentorial fold and the dural porus in the clivus (Dorello's canal), respectively, preventing impingement.[5]
Oculomotor nerve palsy can be identified by ptosis, mydriasis, and ophthalmoparesis. Ischemic lesions, such as diabetes mellitus or hypertension, frequently result in an isolated, complete third nerve palsy with normal pupillary function. Ischemic lesions usually affect the inner core that controls oculomotor functions, leaving the peripheral pupillary fibres intact. In contrast, compressive lesions, such as a posterior communicating artery aneurysm or tumour, affect both peripheral and central fibres, causing pupillary dilation. Even though oculomotor nerve compression was observed in Case 3, pupils were unaffected. Several theories attempt to explain why pupils in compressive aetiologies can be spared. The most frequently accepted theory is that the pupillary fibres are not equally distributed on the surface of the nerve but rather form a separate bundle on the dorsomedial aspect. As a result, compression forces acting in different directions can damage somatomotor neurons while sparing this bundle. Furthermore, the bundle’s placement may differ for some people, rendering compressive forces applied in the usual directions ineffective.[7]
Isolated oculomotor nerve palsy is often caused by compression of the basilar part of the nerve. Acute-onset, isolated oculomotor nerve palsy with severe headaches is usually due to direct compression of the nerve from a posterior communicating artery aneurysm or secondary to subarachnoid haemorrhage.[8] Therefore, while CT is used in an emergency to rule out subarachnoid or intraparenchymal haemorrhages, an MRI with or without gadolinium enhancement is preferred in PA as it provides useful anatomic details.
The definitive treatment for pituitary apoplexy is neurosurgical excision of the lesion using a transnasal-transsphenoidal or transcranial technique, particularly in patients with altered sensorium, visual impairment, or extraocular palsies.[1], [4], [9] To prevent a secondary adrenal crisis, intravenous steroids must be administered until surgery. Our patients underwent early surgery and recovered completely, indicating that the condition is reversible. Early surgical decompression has been shown to improve visual and endocrine outcomes when compared to conservative treatment.
Conclusion
Pituitary apoplexy is one of the crucial differential diagnoses in patients who have isolated oculomotor nerve palsy and ptosis. Atypical presentations may result in significant delays in diagnosis and treatment. Early detection and timely neurosurgical intervention can result in a successful recovery from oculomotor nerve palsy.
Source of Funding
None.
Conflict of Interest
None.
References
- G Barkhoudarian, DF Kelly. Pituitary Apoplexy. Neurosurg Clin N Am 2019. [Google Scholar]
- X Zhu, Y Wang, X Zhao, C Jiang, Q Zhang, W Jiang. Incidence of pituitary apoplexy and its risk factors in Chinese people: A database study of patients with pituitary adenoma. PLoS One 2015. [Google Scholar]
- M Rosso, S Ramaswamy, H Sucharew, A Vagal, Y Anziska, SR Levine. Isolated Third Cranial Nerve Palsy in Pituitary Apoplexy: Case Report and Systematic Review. J Stroke Cerebrovasc Dis 2021. [Google Scholar]
- N Muthukumar. Pituitary Apoplexy: A Comprehensive Review. Neurol India 2020. [Google Scholar]
- H Kobayashi, M Kawabori, S Terasaka, J Murata, K Houkin. A possible mechanism of isolated oculomotor nerve palsy by apoplexy of pituitary adenoma without cavernous sinus invasion: A report of two cases. Acta Neurochir 2011. [Google Scholar]
- M Cahill, J Bannigan, P Eustace. Anatomy of the extraneural blood supply to the intracranial oculomotor nerve. Br J Ophthalmol 1996. [Google Scholar]
- B Ajtai, EJ Fine, N Lincoff. Pupil-sparing, painless compression of the oculomotor nerve by expanding basilar artery aneurysm: a case of ocular pseudomyasthenia. Arch Neurol 2004. [Google Scholar]
- B Diyora, N Nayak, S Kukreja, H Kamble. Sudden onset isolated complete third nerve palsy due to pituitary apoplexy. Oman J Ophthalmol 2011. [Google Scholar]
- M Tu, Q Lu, P Zhu, W Weng. Surgical versus non-surgical treatment for pituitary apoplexy: A systematic review and meta-analysis. J Neurol Sci 2016. [Google Scholar]
