- Visibility 199 Views
- Downloads 36 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2025.025
-
CrossMark
- Citation
A descriptive study of correlation between micro-coaxial phacoemulsification parameters and post-operative endothelial cell loss in noncomplicated phacoemulsification surgery
Abstract
Purpose: To study effect of micro-coaxial phacoemulsification on endothelial cell count in noncomplicated cataract surgery.
Materials and Methods: This was a prospective study, conducted on 150 eyes of cataract patients who underwent microcoaxial phacoemulsification. Clear corneal phacoemulsification was performed using Ozil torsional Technique. Phacoemulsification parameters after cataract surgery as well as pre and post-op endothelial cell count was recorded.
Results: The study included 150 cases of senile cataract with mean age of 64.5 years, 52% being male and 48% being females. Endothelial cell loss of 65-1675 cells/mm2 with (P < 0.001) was noted, which was of high statistical significance. The postoperative EC Loss% ranged from 3.63% to 16.42% with a median of 10.24% (4.32% to 14.67%). A significant +ve correlation (p<0.001) was found between the EC Loss% and different phacoemulsification parameters including CDE, tortional time and volume. Also, EC Loss% was significantly correlated with the grade of nuclear sclerosis (P = 0.045).
Conclusion: Higher grades of cataracts require more phacoemulsification power resulting in increased CDE and EC Loss. Increased aspiration time and the use of excessive amounts of irrigating fluid during phacoemulsification also ends with increased endothelial cell damage.
Introduction
Cataract is a leading cause of treatable blindness in the developing nations, affecting about 20 million people worldwide.[1], [2] Cataract extraction is the most commonly performed surgery in ophthalmic practice. With no associated comorbidity, uneventful cataract extraction with intraocular lens implantation (IOL) is capable of giving almost 100% functional recovery.[3]
The endothelium of cornea is a single layer of mesodermally derived cuboidal cells located at the back of the cornea.[4], [5] Stable morphology and well functioning endothelium is necessary to maintain the long-term transparency of the cornea.[6] Corneal endothelium forms a fluid barrier between the corneal stroma and the aqueous humor, which consists of ion pumps that maintains a relatively low level of stromal hydration.[4], [5]
Normally, Endothelial cell count decreases with age at rate of 0.6%/year. At birth it is around 4000 cells/mm2 which decreases to 2500 cells/mm2 by the age of 80 yrs.[7] At least 400-500 cells/mm2 are required to maintain endothelial pumping.[8] Studies show a variable degree of endothelial cell loss and corneal decompensation post cataract surgery.
Endothelial cells do not regenerate and their repair is accomplished by swelling (polymegatism) and spreading of neighbouring cells, resulting in deviation from the original hexagonal shape (pleomorphism) to maintain endothelial continuity.[5] Intraocular surgery causes additional cell loss due to both heat generated during phacosurgery and fluid turbulence in the anterior chamber.[9] With longer phacoemulsification time and use of excess irrigating fluid, higher EC loss is known to happen.
As compared to traditional longitudinal, Torsional phacoemulsification has proved to be more effective as a result of its side-to-side oscillating shear effect rather than the conventional jackhammer effect. The lens material is cut in both directions, not just during a forward stroke.[10] The tip moves at a frequency of 32 kHz in torsional phacoemulsification. Torsional phacoemulsification theoretically reduces thermal injury, decreases fluid usage, improves followability, and increases cutting efficiency while reducing dispersion of lens material. It achieves this by lowering the frequency and by reducing the frictional movements within the incision.
Therefore, the correlation between postoperative endothelial cell loss and various parameters of microcoaxial phacoemulsification was evaluated in the present study.
Materials and Methods
Present study was conducted on 150 eyes of 150 patients with senile immature cataract undergoing phacoemulsification.
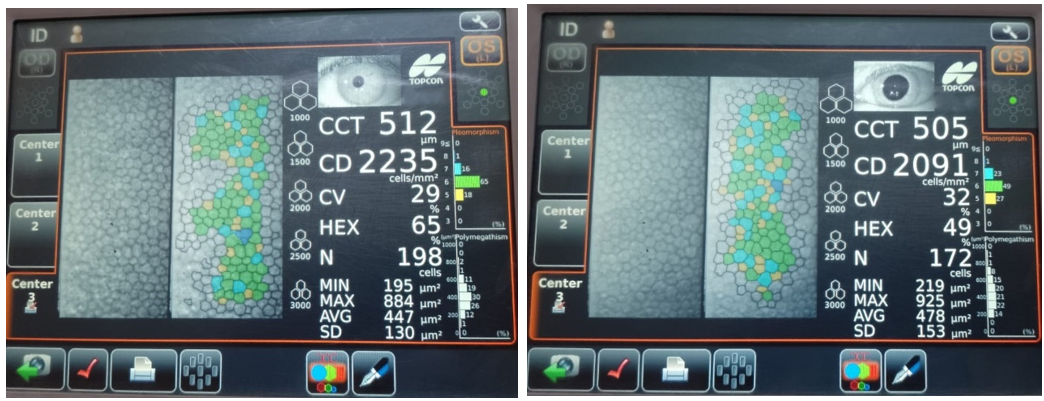
Ethical clearance from the Institutional ethical committee was taken. [IEC no: BV(DU) MC&H/Sangli/IEC/393/20]. After the requisite ethical clearance, written informed consent of the subjects participating in the study was taken. All patients with senile cataract and those willing to participate in the study were included. Patients with small pupil, Psuedoexfoliation, Corneal pathologies, traumatic cataract were excluded from the study. Detailed preoperative examination was carried out including grade of nuclear opalescence using LOCS III classification using slit lamp. Corneal endothelial cell count was measured using specular microscopy. Patients underwent phacoemulsification surgery performed by same experienced senior surgeon. Phacoemulsification parameters including cumulative dissipated energy, total ultrasound time, aspiration time and volume, was recorded. Corneal endothelial cell density using non contact specular microscopy was recorded at post op 1 month.
Preoperative examinations
A complete ophthalmic evaluation including intraocular lens (IOL) power calculation, and an endothelial cell count (ECC) was done. Central corneal ECC was measured using a noncontact specular microscope.
EC Loss% was calculated as follows:
EC Loss (%) = ([preoperative endothelial cell count - postoperative corneal endothelial cell count]/ preoperative endothelial cell count) x 100.
Anesthesia
Topical anesthesia was given to all patients using proparacaine eyedrops. Intracameral Lignocaine (preservative free) was used later in the surgery. Tropicamide + Phenylephrine Eyedrops were put topically pre-operatively to dilate the pupil.
Surgical technique
Micro-coaxial phacoemulsification was carried out with an Ozil Torsional Handpiece 45° Kelman Tip using the Infiniti vision device, with the Ozil IP platform. Phacoemulsification parameters were set according to grade of cataract so as to maintain anterior chamber stability. Two side ports were made. Trypan blue dye was injected and washed to stain the anterior capsule. A OVD, Hydroxyproplyl Methylcellulose Ophthalmic solution (2%), was injected into the anterior chamber. Sodium hyaluronate 1.4% w/v was used in cases of Grade IV and V cataract. Curvilinear capsulorrhexis was made using 26-gauge needle. A standard clear corneal incision was made (at the steep meridian) using a keratome blade. Hydrodissection was carried out. Phacoemulsification was performed. For nucleus management, stop and chop method was utilized and cortex was aspirated using bimanual I/A system. Hydrophilic foldable PCIOL was inserted in the bag. Then OVD was aspirated and side ports were hydrated.
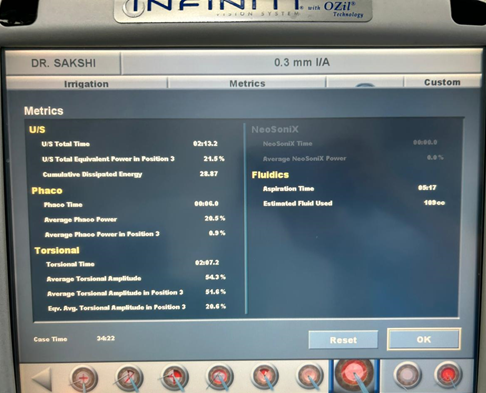
Postoperatively patient was started on: topical prednisolone acetate 1% eyedrops 2-hourly for the 1 day then tapered over next 4 weeks. Topical moxifloxacin drops given four times/day for a month. Nonsteroidal anti-inflammatory eyedrops (Nepafenac 0.1% w/v) was given in all cases for a week. At some point of surgery, the phacoemulsification parameters values had been calculated by the Infinity vision machine. The specific phacoemulsification parameters which were recorded were cumulative dissipated energy, power used in position 3, tortional time and volume of irrigating fluid used.
Statistical analysis
The statistical analysis was performed by SPSS 23.0 version. Continuous variables were described as mean and variation of each observation from the mean value (Standard deviation) represented as mean ± SD or Median (IQR) if they fail to follow normal distribution. Categorical variables were described by taking percentage. Unpaired continuous data for 3 or more than 3 groups following non-normal distribution was analyzed using Kruskal Wallis test. Correlation analysis was done using Spearman correlation test for non-parametric data. Variables with p value <0.05 was considered as statistically significant.
Results
Study was conducted on 150 patients whose mean age was 64.5 ± 10.58 years. 51.67% (77/150) of the group were men and 48.33% (73/150) were women. Majority of patients (65.1%) had grade 2 and 3 of nuclear opalescence as mentioned in [Table 1].
|
Baseline Data |
N=150 |
|
|
Age (Mean ± SD) |
64.5 ± 10.58 |
|
|
Sex Number (Percentage) |
Males |
77 (51.67%) |
|
Females |
73 (48.33%) |
|
|
Nuclear Opalescence |
1 |
8 (5.4%) |
|
2 |
47 (31.5%) |
|
|
3 |
51 (33.6%) |
|
|
4 |
32 (21.5%) |
|
|
5 |
12 (8.1%) |
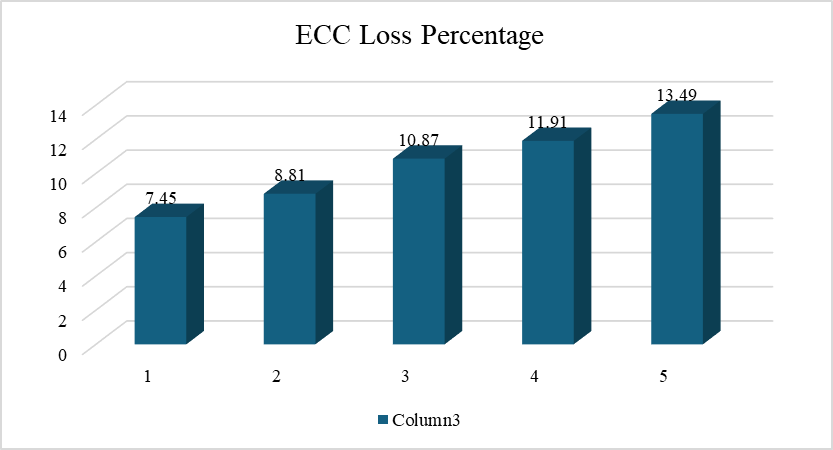
Postoperative EC Loss % ranged from 3.63% to 16.42% with a median (interquartile range) of 10.24% (4.32% to 14.67%) according to the grade of nuclear opalescence as shown in [Figure 3].
|
|
|
N=150 |
|
ECC Loss % |
Mean ± SD |
10.11 ± 6.86 |
|
Median (IQR) |
10.24 (4.32 – 14.67) |
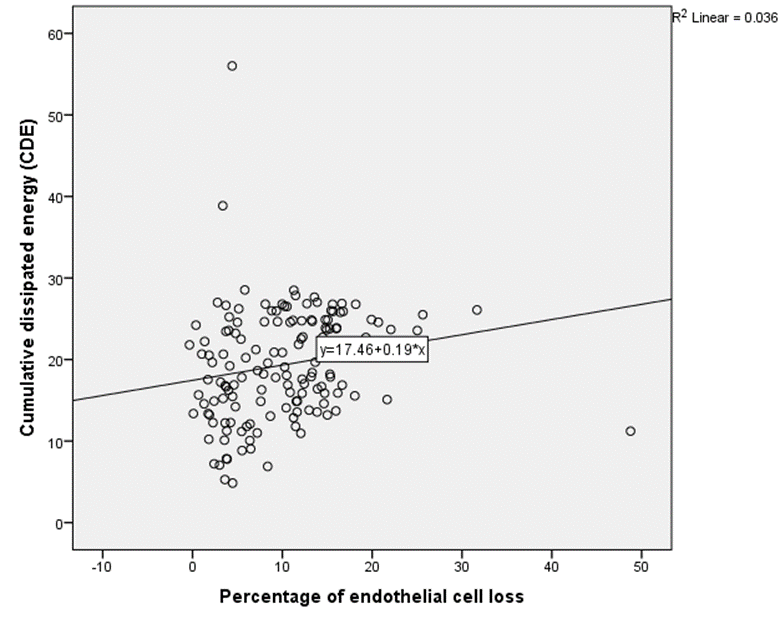
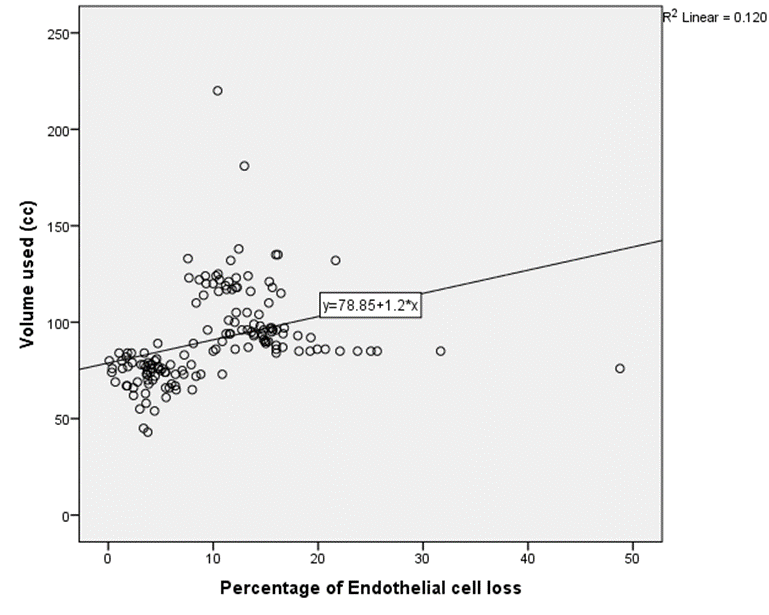
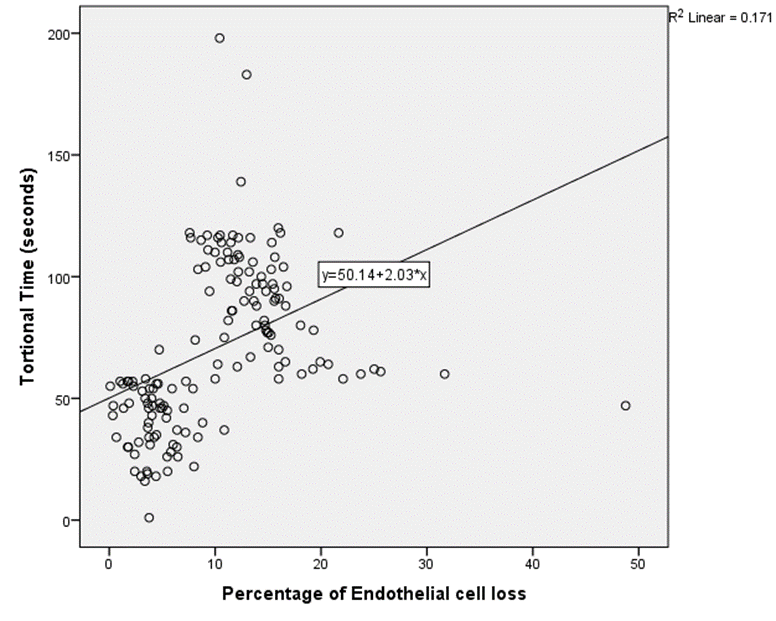
Various parameters including CDE and aspiration volume were recorded at the end of the surgery from metric readouts, details of which has been tabulated in [Table 3]. Correlation of these parameters with ECC was analyzed, p value was calculated and tabulated in [Table 4] and was charted on the graphs as shown in [Figure 4], [Figure 5], [Figure 6].
|
Phaco Parameters (Mean ± SD) |
N = 150 |
|
Power in POS 3 |
17.77 ± 4.39 |
|
CDE |
19.35 ± 6.78 |
|
Tortional Time (seconds) |
70.71 ± 33.75 |
|
Volume Used (cc) |
91.03 ± 23.84 |
|
Variables |
P value |
R value |
|
ECC Loss % vs Power in POS 3 |
<0.001 |
0.578 |
|
ECC Loss % vs CDE |
<0.001 |
0.31 |
|
ECC Loss % vs Tortional Time |
<0.001 |
0.604 |
|
ECC loss % vs Volume Used |
<0.001 |
0.602 |
Significant relationship was noted between grade of nuclear opalescence, CDE and ECC Loss%, with p value < 0.001, as tabulated in [Table 5], [Table 6].
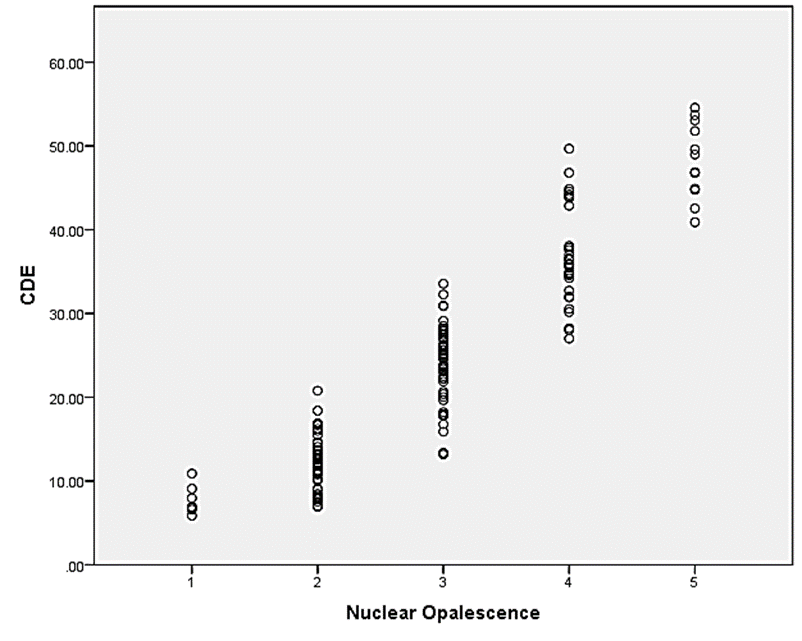
[Figure 7] plots CDE used according to 5 grades of nuclear opalescence. Higher EC Loss % was observed in higher grades of nuclear opalescence.
|
|
P value |
R value |
|
Nuclear Opalescence vs CDE |
<0.001 |
0.937 |
|
Nuclear Opalescence |
1 |
2 |
3 |
4 |
5 |
P value |
|
ECC Loss % |
7.45 |
8.81 |
10.87 |
11.91 |
13.48 |
0.045 |
|
Median (IQR) |
(3.63-14.92) |
(4 -13.86) |
(4.83-13.82) |
(8.45-16.42) |
(9.55-16.34) |
|
Discussion
The study was performed on 150 eyes of 150 patients with an average age of 64.5 years. Male to female ratio was 1.05. Studies such as that of Mohamed AE Soliman Mahdy et al[11] were conducted with similar demographic characteristics. [Table 1] summarizes the demographic characteristics of the patients, while [Table 2] presents the % loss of endothelial cells.
The results of our study showed that a significant percentage of EC loss was correlated with nuclear hardness and increased CDE, with previous studies presenting the same findings.
Bourne, Rupert R. A et al.[12] conducted a study that concluded phacoemulsification significantly increases the risk (OR: 3.7, P = 0.045) of severe endothelial cell loss in the 45 patients with hard cataracts compared to ECCE (52.6% vs. 23.1%; chi-square test, P = 0.041), although both procedures result in similar postoperative visual acuity outcomes. Similar to our study, mean nuclear opacity was shown related to the percentage of endothelial cell loss in the study by Lee et al.[13] Our study included a higher grade of nuclear opalescence (8.1% of our cases were class V) that might have led to the variance in the rate of EC loss. Also in the study by Lee et al,[13] CDE and BSS volume were positively correlated with the degree of nuclear hardness.
The results of M Zeng's[3] study show that Torsional with ultrasound power and fixed high torsional amplitude is both effective and safe for emulsifying hard nuclei with lower Ultrasound time and CDE, causing less corneal damage and promoting earlier recovery of visual acuity than the traditional method.
A strong positive correlation was established between the percentage of EC loss and various phacoemulsification parameters in our study, as shown in [Table 2], [Table 3] and [Figure 2], [Figure 3], [Figure 4]. Increased loss of corneal endothelial cells was found with higher CDE. Apart from that, the amount of BSS used during phacoemulsification was associated with increased EC loss.
As cataract density increased, lens removal required more time and larger volumes of Ringer's solution, causing fluid turbulence in the anterior chamber and thus more endothelial cell loss. A study by H. B Hwang[14] compared the loss of corneal endothelial cells after phacoemulsification according to different anterior chamber depths (ACDs)and reported that endothelial cell loss was significantly higher in ACD I (1.5 < ACD ≤ 2.5 mm) than in ACD III (3.5 < ACD ≤ 4.5 mm) in grades 3 and 4 cataract density groups, 2 months after phacoemulsification (p < 0.05), thus concluding that eyes with shallow ACDs, especially those with relatively hard cataract densities, can be vulnerable to more corneal endothelial cell loss in phacoemulsification surgery. In our study, anterior chamber depth remains a confounding factor, which wasn’t taken into account.
Study by Lucena[15] compared two intraocular irrigating solutions, Balanced Salt Solution Plus (BSS Plus) versus Lactated Ringer’s (Ringer), for the preservation of corneal integrity after phacoemulsification and reported that there were statistically significant correlations between ECD loss and phacoemulsification time (p<0.0001) and ECD loss and irrigation solution volume (p<0.0001) in the Ringer group, but not in the BSS Plus group.
Farahdina Rahmawati[16] conducted a similar study where both the groups (BSS and Ringers respectively) were evaluated for the endothelial cell reduction and corneal endothelial cell morphology change, along with postoperative inflammation. Conclusion of the study was conflicting than that of study by Lucena as all of the results regarding difference in density and corneal cell endothelium morphology between the two groups did not reveal any statistically significant difference (P>0.05) and inflammatory variable in the two groups were even.
The current study also showed a highly significant correlation between EC Loss % and tortional time (p <0.001) indicating that even in cases where energy is not used but the torsional and aspiration time is extended, it results in a higher consumption of irrigating solution, which in turn contributes to corneal endothelial damage.
Conclusion
The results of this study showed that phacoemulsification is associated with a 5-20% loss of corneal endothelial cells 1-3 months after surgery. Study concluded that the percentage of EC Loss was directly correlated with Hardness of cataract. This endothelial cell loss was mainly associated with increased CDE, increased aspiration time, and increased volume of fluid used during the surgical procedure. Even with torsional phacoemulsification, cataracts with increased nuclear hardness require a higher phacoemulsification power (because torsional power alone is not very effective in these cases which require additional longitudinal phacoemulsification power) and thus increased CDE, which can lead to more endothelial cell loss. All these factors must be carefully considered during phacoemulsification, especially in cases where the corneal endothelium is damaged which eventually might lead to corneal decompensation.
Limitations
Heat production, leading to wound burn can potentially damage corneal endothelium. Other entities such as Surge and Anterior chamber stability might also act as compounding factors in phacoemulsification, which has not been taken into account in this study.
Source of Funding
None.
Conflict of Interest
None.
References
- Kohnen T. Compromised corneal endothelium and cataract: how should we decide?. J Cataract Refract Surg. 2011;37(8):1377-8. [Google Scholar]
- Liu Y, Zeng M, Liu X, Luo L, Yuan Z, Xia Y. Torsional mode versus conventional ultrasound mode phacoemulsification: randomized comparative clinical study. J Cataract Refract Surg. 2007;33(2):287-92. [Google Scholar]
- Zeng M, Liu X, Liu Y, Xia Y, Luo L, Yuan Z. Torsional ultrasound modality for hard nucleus phacoemulsification cataract extraction. Br J Ophthalmol. 2008;92(8):1092-6. [Google Scholar]
- Davison J. Cumulative tip travel and implied followability of longitudinal and torsional phacoemulsification. J Cataract Refract Surg. 2008;34(6):986-90. [Google Scholar]
- Miyoshi T, Yoshida H. Ultra-high-speed digital video images of vibrations of an ultrasonic tip and phacoemulsification. J Cataract Refract Surg. 2008;34(6):1024-8. [Google Scholar]
- Wilczynski M, Drobniewski I, Synder A, Omulecki W. Evaluation of early corneal endothelial cell loss in bimanual microincision cataract surgery (MICS) in comparison with standard phacoemulsification. Eur J Ophthalmol. 2006;16(6):798-803. [Google Scholar]
- Werblin T. Long-term endothelial cell loss following phacoemulsification: model for evaluating endothelial damage after intraocular surgery. Refract Corneal Surg. 1993;9(1):29-35. [Google Scholar]
- Mencucci R, Ponchietti C, Virgili G, Giansanti F, Menchini U. Corneal endothelial damage after cataract surgery: microincision versus standard technique. J Cataract Refract Surg. 2006;32(8):1351-4. [Google Scholar]
- Storr-Paulsen A, Norregaard JC, Farik G, Tarnhoj J. The influence of viscoelastic substances on the corneal endothelial cell population during cataract surgery: a prospective study of cohesive and dispersive viscoelastics. Acta Ophthalmol Scand. 2007;85(2):183-7. [Google Scholar]
- Castro L, Dimalanta R, Solomon K. Bead-flow pattern: Quantitation of fluid movement during torsional and longitudinal phacoemulsification. J Cataract Refract Surg. 2010;36(6):1018-23. [Google Scholar]
- Mahdy M, Eid M, Mohammed M, Mohammed M, Hafez A, Bhatia J. Relationship between endothelial cell loss and microcoaxial phacoemulsification parameters in noncomplicated cataract surgery. Clin Ophthalmol. 2012;6:503-10. [Google Scholar]
- Bourne R, Minassian D, Dart J, Rosen P, Kaushal S, Wingate N. Effect of cataract surgery on the corneal endothelium: modern phacoemulsification compared with extracapsular cataract surgery. Ophthalmology. 2004;111(4):679-85. [Google Scholar]
- Lee K, Kwon H, Joo C. Microcoaxial cataract surgery outcomes: comparison of 1.8 mm system and 2.2 mm system. J Cataract Refract Surg. 2009;35(5):874-80. [Google Scholar]
- Hwang H, Lyu B, Yim H, Lee N. Endothelial Cell Loss after Phacoemulsification according to Different Anterior Chamber Depths. J Ophthalmol. 2015;2015. [Google Scholar]
- Lucena D, Ribeiro M, Messias A, Bicas H, Scott I, Jorge R. Comparison of corneal changes after phacoemulsification using BSS Plus versus Lactated Ringer’s irrigating solution: a prospective randomised trial. Br J Ophthalmol. 2011;95(4):485-9. [Google Scholar]
- Rahmawati F, Supartoto A, Gunawan W, Ekantini R, Prabowo R, Mahayana I. Density and morphology of corneal endothelial cell after phacoemulsification using Ringer lactate versus balanced salt solution as irrigating solutions. Int Eye Sci. 2018;18(2):207-12. [Google Scholar]
How to Cite This Article
Vancouver
Mandlik HR, Pandharikar AJ, Patil SR, Lanje KN, Joshi AK, Gotekar RB. A descriptive study of correlation between micro-coaxial phacoemulsification parameters and post-operative endothelial cell loss in noncomplicated phacoemulsification surgery [Internet]. Indian J Clin Exp Ophthalmol. 2025 [cited 2025 Oct 12];11(1):142-147. Available from: https://doi.org/10.18231/j.ijceo.2025.025
APA
Mandlik, H. R., Pandharikar, A. J., Patil, S. R., Lanje, K. N., Joshi, A. K., Gotekar, R. B. (2025). A descriptive study of correlation between micro-coaxial phacoemulsification parameters and post-operative endothelial cell loss in noncomplicated phacoemulsification surgery. Indian J Clin Exp Ophthalmol, 11(1), 142-147. https://doi.org/10.18231/j.ijceo.2025.025
MLA
Mandlik, Hanumant Rangnath, Pandharikar, Aishwarya Jayant, Patil, Sakshi Ravikant, Lanje, Kamlesh Najukram, Joshi, Ajit Kamalakar, Gotekar, Rajesh Balkrishna. "A descriptive study of correlation between micro-coaxial phacoemulsification parameters and post-operative endothelial cell loss in noncomplicated phacoemulsification surgery." Indian J Clin Exp Ophthalmol, vol. 11, no. 1, 2025, pp. 142-147. https://doi.org/10.18231/j.ijceo.2025.025
Chicago
Mandlik, H. R., Pandharikar, A. J., Patil, S. R., Lanje, K. N., Joshi, A. K., Gotekar, R. B.. "A descriptive study of correlation between micro-coaxial phacoemulsification parameters and post-operative endothelial cell loss in noncomplicated phacoemulsification surgery." Indian J Clin Exp Ophthalmol 11, no. 1 (2025): 142-147. https://doi.org/10.18231/j.ijceo.2025.025
