- Visibility 503 Views
- Downloads 56 Downloads
- Permissions
- DOI 10.18231/j.ijceo.2025.010
-
CrossMark
- Citation
Effect of cyclopentolate on ocular biometric parameters
Abstract
Background: Accurate measurement of axial length (AL), anterior chamber depth (ACD) and corneal curvature (CC) is essential for the calculation of IOL power according to different formulas. Assessing ACD is important to determine whether there is enough room for the PC-IOLs. It is evident that a shallow ACD and/or narrow angle may increase the risk of iris pigment chaffing, particularly when posterior chamber hyperopic PC-IOLs are implanted. Overestimation of ACD may result in corneal endothelial cell damage. Cyclopentolate is a synthetic antimuscarinic cycloplegic agent available in 0.5% and 1% solutions. It is widely accepted drug for patients of all ages providing excellent short-term cycloplegia. This study aims to compare the effect of cyclopentolate 1% on ocular biometric parameters – Anterior chamber depth (ACD), Lens thickness (LT) and Axial length (AL) before and after dilatation.
Materials and Methods: In this observational study, 25 eyes of patients aged 45-75 years with significant cataract with nuclear sclerosis grading up to NO5NC5 C4 P4 (according to LOCS III) were included. The study was conducted for a duration of 3 months. Ocular biometric parameters ACD, LT and AL were measured using A-scan by immersion technique and compared before and after dilatation using 1% cyclopentolate and the data was analysed using paired T-test.
Results: Statistically significant difference (p value < 0.05) was observed in LT and ACD, while no significant difference was noted in AL post-cycloplegia.
Conclusion: Cycloplegia can significantly affect the ocular biometric parameters – deeper ACD and thinner LT. These changes in ocular biometric parameters should be considered in calculating IOL power to prevent refractive surprises after cataract surgery.
Introduction
Currently, cycloplegic agents like tropicamide, homatropine and cyclopentolate have both diagnostic and therapeutic applications. These clinical applications encompass procedures such as dilated fundus examination, cycloplegic refraction, treatment of uveitis, pharmacological penalization for amblyopia treatment[1] in children, in the treatment of accommodative esotropia and as a part of initial treatment in managing acute angle closure glaucoma.
Detailed evaluation of the anterior segment is crucial for evaluating the suitability for corneal refractive surgery, for diagnosis and monitoring of changes in patients with glaucoma, for calculating the intraocular lens (IOL), and in determining the optimal position of the lens in cataract surgery and phakic IOL implantation.[1], [2], [3]
Accurate measurements of axial length (AL), anterior chamber depth (ACD), and corneal curvature (CC) are crucial in determining appropriate values for the calculation of IOL power for cataract surgery according to different formulas.[4], [5] Ensuring precision in these measurements is essential to enhance postoperative visual outcomes and patient satisfaction.
Evaluating ACD is a critical aspect of preoperative assessments, to ascertain sufficient space for posterior chamber intraocular lenses (PC-IOLs). The consideration of angle dimensions becomes particularly important, especially for an anterior chamber angle (ACA) fixated lens. It is evident that a shallow ACD and/or narrow-angle may pose potential risks, notably an increased likelihood of iris pigment chaffing, especially in cases when involving the implantation of posterior chamber hyperopic PC-IOLs.[6], [7] Through examination of these factors is essential to mitigate complications and optimize the overall success of intraocular implantation procedures.
When ACD is overestimated, there is a potential risk of causing damage to the corneal endothelial cells. This may contribute to adverse effects on the delicate endothelial cell layer of the cornea.[2] [3]
Cyclopentolate is a synthetic antimuscarinic cycloplegic agent which is available in 0.5% and 1% solutions for various diagnostic procedures and therapeutic purposes in ophthalmology.[8] It induces mydriasis by relaxing the circular muscle of the iris and prevents contraction of the radial ciliary muscle, induces relaxation of suspensory ligaments, and therefore the lens capsule producing cycloplegia.[9]
Cycloplegic effects of cyclopentolate begin at 25-75 minutes after administration of the drop and recovery time is approximately 6–24 hours. It’s essential to note that the duration of effects produced by cyclopentolate may vary, and patients may experience blurred vision and sensitivity to light during this time. Ocular side effects may include irritation, lacrimation, allergic blepharoconjunctivitis, conjunctival hyperemia and increase in intraocular pressure. Some of its systemic side effects are drowsiness, ataxia, disorientation, incoherent speech, restlessness, and visual hallucinations. It is essential to consider individual patient factors and potential contraindications to ensure safe and effective use.
As cyclopentolate is useful in various clinical settings with rapid onset of action allowing efficient examination with a relatively shorter duration of action without prolonged effects, and an established safety profile, it is widely preferred as a drug of first choice for all age groups in achieving excellent short-term cycloplegia, which is essential for accurate assessment of refraction and various eye examinations.[9]
This study was aimed at comparing the effect of cyclopentolate 1% on ocular biometric parameters – Anterior chamber depth (ACD), Lens thickness (LT) and Axial length (AL) before and after dilatation.
Materials and Methods
A prospective observational study was conducted at the department of Ophthalmology, Alluri Sitarama Raju Academy of Medical Sciences, Eluru, Andhra Pradesh. The study was conducted over a period of 3 months from June 2023 to August 2023. Prior to the study, the Institutional research committee and ethics committee approval was obtained. All the patients who gave informed consent and fulfilled the inclusion and exclusion criteria were included in the study.
Sample size
A total of 25 eyes of 25 patients meeting the inclusion and exclusion criteria were included in the study. The study population consisted of both males and females between 45-75 years of age group.
Inclusion criteria
Patients belonging to the above-mentioned age group having visually significant cataract with nuclear sclerosis grading up to NO5NC5 C4 P4 according to LOCS III (Lens Opacities Classification System III) were included in the study. Patients with clear central cornea and patients with cataract with no ocular and systemic diseases were included in this study.
Exclusion criteria
Patients with previous history of refractive corneal surgeries, previous history of ocular trauma, corneal ectasia, and co-existing corneal or ocular pathology were not included to be a part of this study.
Study procedure
All the patients meeting the inclusion and exclusion criteria underwent visual acuity assessment (Snellen’s charts), detailed anterior segment evaluation using slit lamp biomicroscope, Dilated fundus examinations using slit lamp biomicroscope with the help of +90 D or +78 D lens, and anterior segment OCT (Optical Coherence Tomography) to rule out corneal abnormalities.
Ocular biometric parameters - Axial length (AL), Lens thickness (LT), and Anterior chamber depth (ACD) were measured using A-scan ultrasonography (BIOMEDIX) by using an immersion technique.
All the patients selected for the study were assessed for the above-mentioned parameters initially pre-dilatation after a detailed evaluation of the eye and then assessed for similar parameters post-dilatation using the following technique and the parameters were compared using statistical methods.
Ocular biometric parameters were initially assessed pre-dilatation. Cyclopentolate 1% (Dilate Eye Drops, MICRO LABS) was instilled one drop every 10 minutes for three applications and maximum cycloplegic effect is seen between 45 and 90 min following the final eye drop administration. The parameters were re-assessed post-dilatation after instillation of last drop after 30 minutes with a pupil dilatation equal to 7-8 mm.
All the measurements were done under the supervision of an experienced optometrist who did not have access to the pre and cycloplegic data, to prevent any bias or error.
Statistical analysis
The data was analysed using a Microsoft Excel data sheet with Statistical Package for Social Sciences (SPSS) 20 version. All descriptive statistics were expressed as mean ± standard deviation. A Paired sample t-test was used for comparing the effect of Cyclopentolate before and after dilatation. A p-value < 0.05 was considered statistically significant.
Results
A total of 25 eyes of 25 patients were evaluated in the study. The mean age of the patients in the study was 61.96 ± 7.38 with a range of 45-75 years. The patients were divided according to the sex distribution in the [Table 1] based on the percentage.
|
Sex distribution |
Number |
Percentage (%) |
|
Male |
12 |
48% |
|
Female |
13 |
52% |
|
Total |
25 |
100% |
Among total 25 patients about 48% are males and 52% are females. ([Table 1])
The changes in specific ocular biometric parameters before and after dilatation are depicted in a [Table 2].
|
Ocular biometric parameters |
Status of the eye |
Mean ± Standard Deviation |
95% Confidence Interval |
p value |
|
Axial length |
Pre-dilatation |
23.016±0.823 |
22.67 to 23.35 |
0.112 |
|
Post-dilatation |
23.069±0.840 |
22.72 to 23.42 |
||
|
Lens thickness |
Pre-dilatation |
4.027±0.557 |
3.79 to 4.26 |
0.004 |
|
Post-dilatation |
3.957±0.50 |
3.75 to 4.17 |
||
|
Anterior chamber depth |
Pre-dilatation |
3.13±0.449 |
3.06 to 3.43 |
0.0001 |
|
Post-dilatation |
3.248±0.447 |
3.06 to 3.43 |
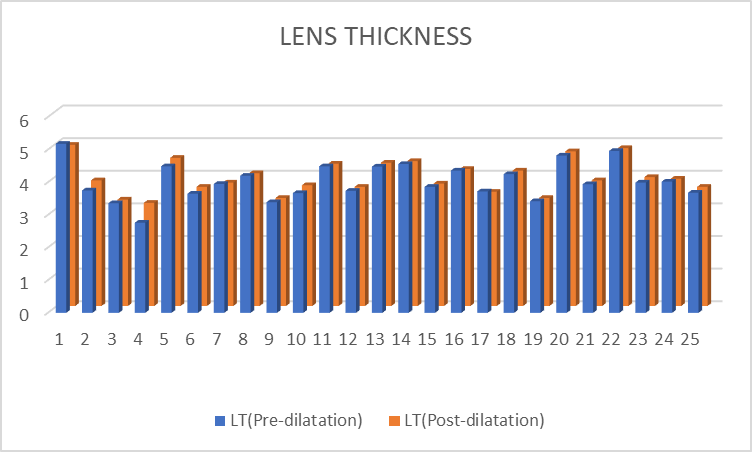
The Mean change in the lens thickness post-dilatation was 3.957±0.50 compared to pre-dilatation which was 4.027±0.557. Statistically significant difference was observed post-dilatation in the Lens thickness (LT) with a p-value of 0.004.([Figure 1])
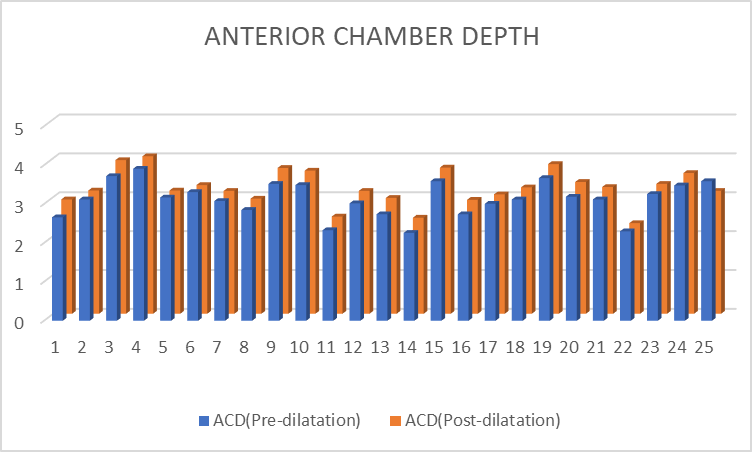
The mean change in the Anterior Chamber Depth (ACD) post-dilatation was 3.248±0.447 compared to pre-dilatation which was 3.13±0.449. A Statistically significant difference was observed post-dilatation in the Anterior Chamber Depth (ACD) with a p-value of 0.0001. ([Figure 2])
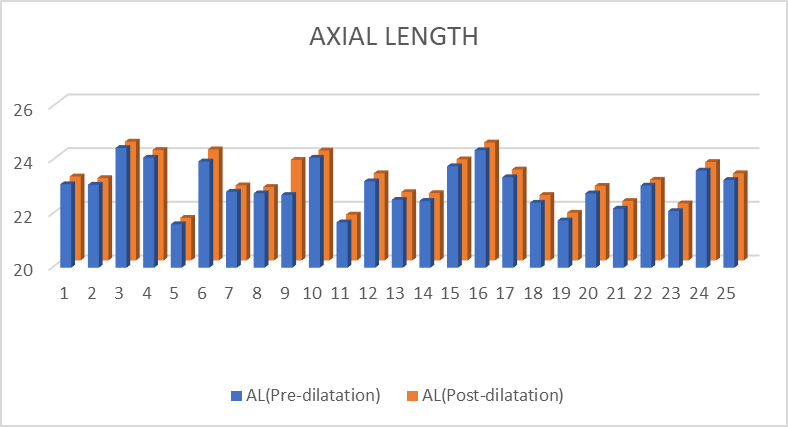
While there is no statistically significant difference observed in the Axial length post-dilatation with a mean change in the Axial Length (AL) 23.016±0.823, 23.069±0.840 pre-dilation and post-dilatation, respectively with a p-value of 0.112. ([Figure 3])
Discussion
In the current study, we have compared the mean change in the ocular biometry components following cycloplegia. The results from this study showed a significant increase in the anterior chamber depth after producing cycloplegia using cyclopentolate 1%. As reported, accurate measurement of ACD is an important factor for precise calculation of IOL power for cataract surgery, and can lead to corneal endothelial cell damage after IOL implantation, so imprecise measurement may lead to undesirable refractive errors after cataract surgery, and to avoid IOL-cornea touch which can affect the patient’s visual outcome and satisfaction, and in the diagnosis of primary angle closure glaucoma (PACG) and individuals at risk which is crucial for timely intervention and preventing complications like optic nerve damage.[1], [2], [10]
Rodriguez-Raton et al[11] found that ACD and IOL power, calculated using the Haigis formula (ACD is used in this formula) after the application of tropicamide and phenylephrine underscore the sensitivity of this formula to specific cycloplegic agents. Remarkably, the unaffected IOL power calculation based on SRK/T formula suggests formula-specific responses to the cycloplegic agents. This emphasizes the importance of selecting an appropriate IOL power calculation formula based on the potential impact of specific pharmacological interventions.
The study showed a significant decrease in the lens thickness after producing cycloplegia using cyclopentolate 1%. Similar to the present study findings, several studies have reported a reduction in the LT after inducing cycloplegia.[10], [11], [12], [13] Ocular accommodation causes the ciliary muscle to contract, leading to an increase in the lens thickness and forward movement of the lens occurs,[14] while the ciliary muscle undergoes temporary paralysis leading to an increase in ACD by flattening the crystalline lens resulting from reduced tension on the zonular fibres and by backward displacement of the geometrical centre of the lens.[15], [16] Arriola-Villalobos et al. reported that there is no statistically significant change in the lens thickness following pupil dilation using tropicamide 1% in an elderly cataract population (mean age, 74.71 ± 53).[17] While tropicamide primarily targets pupillary dilatation by affecting the iris sphincter muscle, its impact on lens thickness might be less pronounced, especially in elderly individuals with existing cataracts.
The study showed no statistically significant difference in the axial length after producing cycloplegia using cyclopentolate 1%. On the contrary, there are studies that reported statistically, significant changes in AL following cycloplegia, but the absence of clinically significant changes induced by homatropine 2% and cyclopentolate 1%.[10]
Currently, cataract surgery has evolved into a refractive surgery, driven by advancements in the quality of intraocular lens. The prediction of refractive error after cataract surgery involves multiple reasons, which include a selection of appropriate intraocular lens power formula, which depends on various factors like patient age, axial length, corneal power, and surgeon preference, and the accuracy of the various devices used to measure the ocular biometric parameters.[18] Advancements in IOL technology and the use of premium IOLs, accurate ocular biometry measurements, and IOL power calculation, contributing to more reliable predictions have become crucial in reaching the target refraction after cataract surgery. Due to inaccurate biometric measurements, clinicians may face less than desirable refractive outcomes.[19]
Can et al. reported the impact of cycloplegia on IOL power calculations, which was negligible except for an increase of power >0.50 D in two cases among healthy volunteers with a mean age 33.12 ± 9.2 years obtained using SRK/T formula with AL-Scan optical biometer.[20] This observation emphasizes the importance of considering individual variability and potential formula-specific responses when implementing cycloplegic agents. Precise determination of keratometry and biometric parameters, coupled with the use of accurate IOL power calculation formulas, is integral to contemporary cataract and refractive surgery. Ensuring the meticulous execution of these measures is imperative to not only meet the increasing expectations of the patients but also to attain desired target refractive outcomes.[21]
Cycloplegia has a certain effect on ocular biometric parameters of the eye which will further affect the accuracy of optometric measurements and refractive surgery, for example, calculating the power of intraocular lens. The effects of cycloplegia on biometric parameters varies across different age groups which should be taken into consideration during calculation of intraocular power of lens according to different formulas.
Limitations
We have considered a small sample size with 25 eyes of 25 patients. Including a larger sample size might affect the results which should be considered into account.
Comparative analysis of ocular biometric parameters pre-dilatation and post-dilatation using a single drug (Cyclopentolate) offer valuable insights into the drug-specific effects. However, comparing the results using other cycloplegic agents like atropine, tropicamide or phenylephrine is essential to note varying degrees of cycloplegia and distinct changes in ocular biometric parameters which might give a different result. Variations in drug potency, duration of action and individual patient responses can contribute to differences in outcomes.
Conclusion
The impact of cycloplegia on ocular biometric parameters – deeper ACD and thinner LT should be taken into consideration while calculating intraocular lens (IOL) power for cataract surgery. These changes in ocular biometric parameters can influence the effective lens position, which is a crucial factor in determining the appropriate IOL power to achieve desired postoperative visual outcome. The awareness of cyclopentolate-induced changes in ocular biometric parameters underscores the importance of meticulous preoperative assessments in cataract surgery. Advanced biometry techniques and accurate measurements become imperative in this context, ensuring precision in IOL power calculations and minimizing the risk of postoperative complications related to refractive errors.
Source of Funding
Nil.
Conflicts of Interest
Nil.
References
- Arici C, Turk A, Ceylan O, Kola M, Hurmeric V. Effects of 1% cyclopentolate hydrochloride on anterior segment parameters obtained with Pentacam in young adults. Arq Bras Oftalmol. 2014;77(4):228-32. [Google Scholar]
- Niyaz L, Can E, Seymen Z, Eraydin B. Comparison of anterior segment parameters obtained by dual-Scheimpflug analyzer before and after cycloplegia in children. J Pediatr Ophthalmol Strabismus. 2016;53(4):234-7. [Google Scholar]
- Guler E, Guragac F, Tenlik A, Yagci R, Arslanyilmaz Z, Balci M. Influences of topical cyclopentolate on anterior chamber parameters with a dual-Scheimpflug analyzer in healthy children. J Pediatr Ophthalmol Strabismus. 2015;52(1):26-30. [Google Scholar]
- Huang J, Mcalinden C, Su B. The effect of cycloplegia on the lenstar and the IOLMaster biometry. Optom Vis Sci. 2012;89:1691-1697. [Google Scholar]
- Arriola-Villalobos P, Díaz-Valle D, Garzon N, Ruiz-Medrano J, Fernández-Perez C, Alejandre-Alba N. Effect of pharmacologic pupil dilation on OLCR optical biometry measurements for IOL predictions. Eur J Ophthalmol. 2014;24(1):53-7. [Google Scholar]
- Gimbel H, Norton N, Amritanand A. Angle-supported phakic intraocular lenses for the correction of myopia: three-year follow-up. J Cataract Refract Surg. 2015;41(10):2179-89. [Google Scholar]
- Kamiya K, Shimizu K, Igarashi A, Kitazawa Y, Kojima T, Nakamura T. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol. 2018;102(2):177-81. [Google Scholar]
- Bartlett J. Administration of and adverse reactions to cycloplegic agents. Am J Optom Physiol Opt. 1978;55(4):227-33. [Google Scholar]
- Waller D, Sampson A, Waller D, Sampson A. 50 - The eye. Medical Pharmacology and Therapeutics. 2018. [Google Scholar]
- Bhatia J. Effect of tropicamide and homatropine eye drops on A-scan parameters of the phakic normal eyes. Oman Med J. 2011;26(23):25-5. [Google Scholar]
- Rodriguez-Raton A, Jimenez-Alvarez M, Arteche-Limousin L, Mediavilla-Pena E, Larrucea-Martinez I. Effect of pupil dilation on biometry measurements with partial coherence interferometry and its effect on IOL power formula calculation. Eur J Ophthalmol. 2015;25(4):309-14. [Google Scholar]
- Arriola-Villalobos P, Gomez J, Garzon N, Ruiz-Medrano J, Fernández-Pérez C, JM. Effect of pharmacological pupil dilation on measurements and IOL power calculation made using the new swept-source optical coherence tomography-based optical biometer. J Fr Ophtalmol. 2016;39(10):859-65. [Google Scholar]
- Higashiyama T, Iwasa M, Ohji M. Changes in the anterior segment after cycloplegia with a biometer using swept-source optical coherence tomography. PLoS One. 2017;12(8). [Google Scholar]
- Malyugin B, Shpak A, Pokrovskiy D. Accommodative changes in anterior chamber depth in patients with high myopia. J Cataract Refract Surg. 2012;38(8):1403-7. [Google Scholar]
- Chang S, Lo A, Su P. Anterior segment biometry changes with cycloplegia in myopic adults. Optom Vis Sci. 2016;93(1):12-8. [Google Scholar]
- Özyol P, Özyol E, Baldemir E. Changes in ocular parameters and intraocular lens powers in aging cycloplegic eyes. Am J Ophthalmol. 2017;173:76-83. [Google Scholar]
- Arriola-Villalobos P, Díaz-Valle D, Garzòn N, Ruiz-Medrano J, Fernández-Perez C, Alejandre-Alba N. Effect of pharmacologic pupil dilation on OLCR optical biometry measurements for IOL predictions. Eur J Ophthalmol. 2014;24(1):53-7. [Google Scholar]
- Kane J, Chang D. Intraocular lens power formulas, biometry, and intraoperative aberrometry: A review. Ophthalmology. 2021;128(11):94-114. [Google Scholar]
- Ozcaliskan S, Yenerel N. The effect of cycloplegia on biometric measurements using swept-source optical coherence tomography-based biometry. Clin Exp Optom. 2019;102(5):501-5. [Google Scholar]
- Can E, Duran M, Çetinkaya T, Arıtürk N. The effect of pupil dilation on AL-Scan biometric parameters. Int Ophthalmol. 2016;36:179-83. [Google Scholar]
- Sahin A, Hamrah P. Clinically relevant biometry. Curr Opin Ophthalmol. 2012;23(1):47-53. [Google Scholar]
How to Cite This Article
Vancouver
Haritha T, Pakalapati P. Effect of cyclopentolate on ocular biometric parameters [Internet]. Indian J Clin Exp Ophthalmol. 2025 [cited 2025 Nov 04];11(1):53-57. Available from: https://doi.org/10.18231/j.ijceo.2025.010
APA
Haritha, T., Pakalapati, P. (2025). Effect of cyclopentolate on ocular biometric parameters. Indian J Clin Exp Ophthalmol, 11(1), 53-57. https://doi.org/10.18231/j.ijceo.2025.010
MLA
Haritha, Thamatam, Pakalapati, Pradeep. "Effect of cyclopentolate on ocular biometric parameters." Indian J Clin Exp Ophthalmol, vol. 11, no. 1, 2025, pp. 53-57. https://doi.org/10.18231/j.ijceo.2025.010
Chicago
Haritha, T., Pakalapati, P.. "Effect of cyclopentolate on ocular biometric parameters." Indian J Clin Exp Ophthalmol 11, no. 1 (2025): 53-57. https://doi.org/10.18231/j.ijceo.2025.010
