Introduction
Persistent hyperplastic primary vitreous (PHPV) is an innate manifestation of ocular anomaly that arises due to non absorption of embryonic primary vitreous or persistent vitreous proliferation during the embryogenesis.1 Structural manifestations include small corneas, shallow anterior chamber, retrolental membranes, glaucoma, persistent vitreous arteries and fundus abnormalities. PHPV presents unilaterally in majority of patients and exhibits sporadic inheritance without systemic associations.2
PHPV is classified into three sub divisions depending on the location of the affected ophthalmic features.3 Anterior PHPV is related with opacified lens, retrolental membrane and elongated ciliary body. Posterior PHPV is related with link between the vitreous vascular membrane and the optic nerve head, small globe and hypoplasia of the posterior pole and retina. In mixed PHPV, both anterior and posterior signs are present.
Long term sequalae of PHPV encompass vitreous hemorrhage, angle closure glaucoma and retinal detachment. PHPV is one of the primary etiology of infantile leukocoria and is misinterpreted as congenital cataract and mimicker of retinoblastoma.4 PHPV is generally diagnosed based on the investigative modalities namely optical coherence tomography (OCT), B-mode ultrasound or Doppler ultrasound.4, 5
This report describes presentation of a 12-year-old boy who complained of blurring of distant vision. A greyish band protruded into the vitreous cavity was detected on dilated fundus.
Case Report
A 12-year-old boy came for routine ophthalmic examination with no associated significant history. Bilaterally; uncorrected visual acuity was 6/12 on examination. Eyes were orthophoric and extra ocular movements were full and free. The anterior segment was within normal limits.
Figure 1
a,c): Slit lamp examination of the right eye. b,d): Slit lamp examination of the left eye. Both eyes show greyish band originating from optic disc and projecting into vitreous cavity on retro-illumination
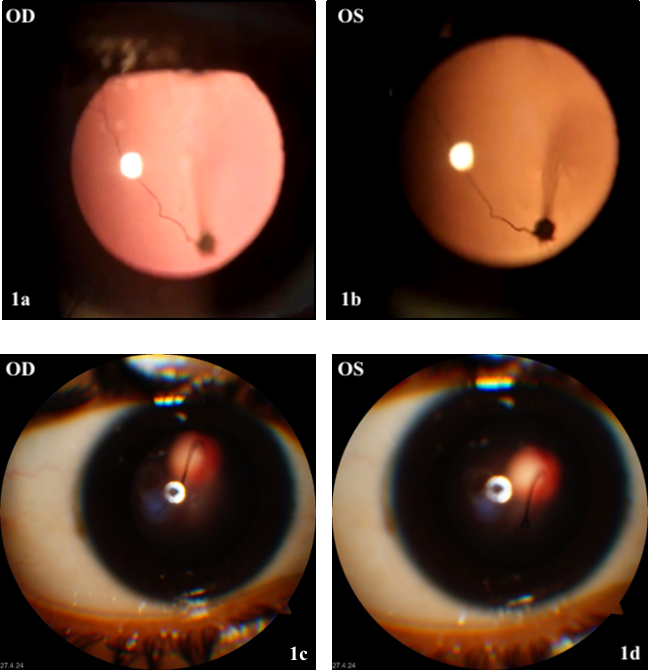
Dilated fundus photography of both eyes, showed an attached retina with well-defined vasculature; healthy macula; morphologically normal optic disc and a greyish band that emanated from optic nerve head projecting into the vitreous cavity on retro illumination.
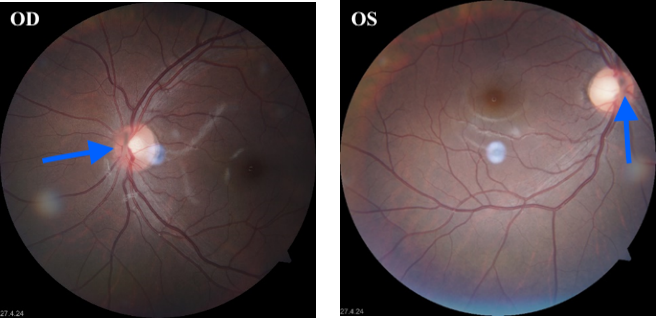
Figure 2
Fundus photography of both eyes showing a well attached retina and a greyish band emanating from the optic disc into the vitreous (Blue arrow)
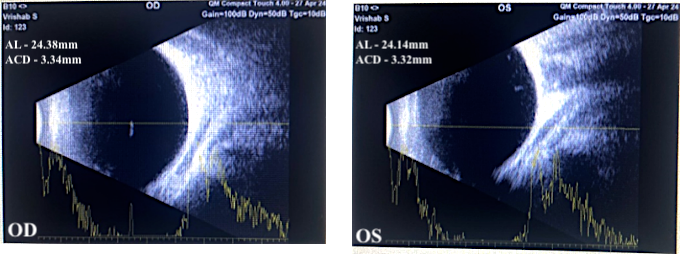
B scan (Figure 3) of right eye showed well defined hyperechoic lesion in the vitreous cavity suggestive of retrolental membrane. Left eye showed echogenic membrane attached to optic nerve head and thickening of chorioretinal layer.
In conformity with the above features, bilateral PHPV was diagnosed with nil associated systemic abnormalities. Cycloplegic refraction was done and best corrected visual acuity was 6/6 with myopic glasses.
Discussion
PHPV is an infrequent developmental congenital ocular anomaly primarily extensively described in 1955 by Reese AB.6 In 1997; Goldberg M rephrased Persistent Fetal Vasculature Syndrome (PFVS) as insistence of primary vitreous and embryonic hyaloid vasculature due to cessation in the process of their normal involution within the specific time.1 It results in wide range of ocular complications such as an angle closure glaucoma due to shallow AC, cataracts, ciliary processes elongation commonly in normal infants. As PHPV is a congenital ocular anomaly, dilated fundus evaluation of affected children is mandatory. Even though, fundus was adequately visible to see the entire band of vitreous on dilatation, majority of times media is opaque in presence of retrolental mass or cataract that necessitates further neuroimaging.7 Apart from diagnosing PHPV, it also divides it into anterior, posterior or mixed variety and aids in initiating further treatment. Nonetheless neuroimaging also excludes retinoblastoma, one of the major differentials with devastating sequelae.8 Despite the poor visual prognosis of PHPV, timely intervention is the most important determinant for final visual prognosis.9 Clinical manifestations include small eye balls, small corneas, shallow anterior chamber, retrolental membranes, glaucoma, persistent vitreous arteries and fundus abnormalities
Bilateral presentations of PHPV is rare and is usually associated with syndromes which was unlikely in our presentation.10 Thus, we report an atypical PHPV which exhibited distinct features:
Asymptomatic patient.
Fundoscopy revealed anomalous fibrovascular band originating from optic disc with clear vitreous and attached retina.
Both anterior and posterior segment findings would manifest in a typical PHPV. On the contrary; no anterior segment clinical manifestations was observed in this patient. Prominent fibrovascular band in the vitreous can be categorized as posterior PHPV, but this membrane structurally didn’t alter posterior segment anatomy.
Conclusion
PHPV with myopia represents unique sub-type of PHPV as they don’t manifest with typical clinical findings. Improvement of vision in this case of myopic PHPV suggests that a more conservative approach rather than surgical management to obtain the best corrected vision with glasses. This case was unique as it was not discovered until teenage as the patient was asymptomatic since birth.