Introduction
Infection with herpes virus may cause widespread or localised systemic illness. Ocular involvement may occur as primary infection or a reactivation of latent disease resulting in a spectrum of ophthalmic inflammation.1 Herpes Simplex Virus (HSV) 1 and 2 are known to cause ophthalmic involvement. The interaction between viral activity and the immune response of the host determines the extent of disease.2
Case Report
An 89-year-old male patient presented to the emergency department with complaints of fever for 2 days associated with chills and rigors, defective vision, history of multiple episodes of fall due to difficulty in walking, with involuntary movements in the right side of his body. He also had complaints of hiccups for 2 days associated with aphasia for 1 day. He was a known case of systemic hypertension for 2 years with history of treatment for pulmonary aspergillosis, bronchial asthma and mood disorder and was newly diagnosed with type 2 diabetes mellitus.
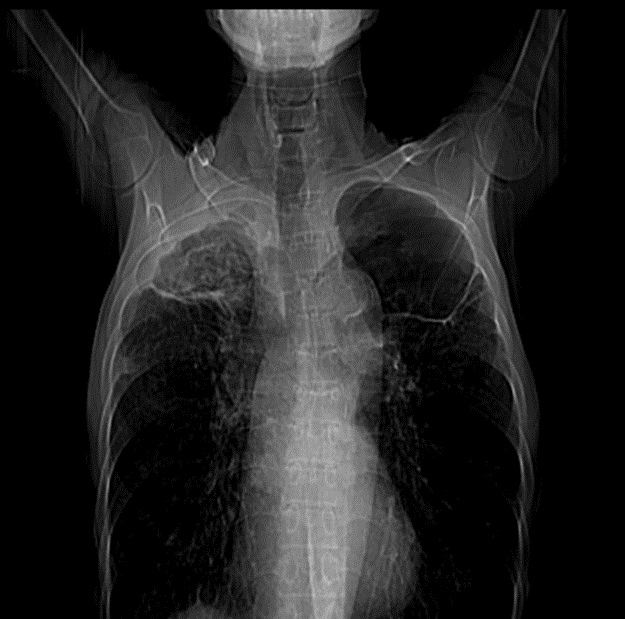
He was admitted in the intensive care unit for management and observation. Blood investigations revealed hyponatremia, hypokalaemia and anaemia (haemoglobin of 8.8g/dl). Total white blood cell counts were 3780 per mm3 with platelets of 1 lakh per mm3. Magnetic resonance imaging of the brain showed T2/Flair hyperintensity and gyral oedema with diffusion restriction in the left temporal lobe, hippocampus, extending into the left insular cortex, left external capsule and mild effacement of the temporal horn of left lateral ventricle all findings raising the possibility of herpes simplex encephalitis. Patient was started on intravenous antimicrobial injections of 1gram meropenam twice daily and polymyxin E 2 million international units. For his convulsions, intravenous injection brivaracetam 100mg twice daily and sodium valproate 500mg IV thrice daily was given. Injection acyclovir 500mg thrice daily and tablet voriconazole 400mg twice daily was initiated as antiviral antifungal treatment respectively. Nebulisation with budecort twice daily and ipratropium bromide 2cc per nasal thrice daily was also given. His Glasgow Coma Scale was monitored. Patient was intubated in view of respiratory distress and underwent tracheostomy due to worsening of his systemic condition. Computed tomography scanogram was done (Figure 2). The apical segment of right upper lobe shows a bronchiectatic cavity with an attached curvilinear soft tissue density lesion with crenated margins. Surrounding the cavity, there is extensive fibrosis with bronchiectasis and few parenchymal calcific specks and adjacent pleural thickening – possibility of cavity with fungal component within (chronic pulmonary Aspergillosis).
Ophthalmic examination was performed prior to lumbar puncture to rule out disc oedema. The patient was drowsy and intubated during examination and hence the bedside vision, colour vision and extra ocular movements were not reliable. Anterior segment showed pseudophakia in both eyes with nasal pterygium in the right eye. Pupils were round, briskly reactive, no relative afferent pupillary defect was present and digital intraocular pressure was normal in both eyes. Fundus evaluation in both eyes showed pale optic disc, circumferential retinal infiltrates at the periphery, vitritis and patchy sheathing along arteries (Figure 1). A provisional diagnosis of herpetic retinitis was made and he was advised to continue intravenous acyclovir.
Figure 1
Active retinal infiltrates with vasculitis and vitritis with corresponding fundus fluorescein angiography

Figure 2
Computed tomography scanogram showing cavity in upper lobes suggestive of chronic pulmonary aspergillosis
On review after 24 hours, fundus showed creamy choroidal patches suggestive of aspergillus endophthalmitis and a combined aetiology for the retinitis was considered. On the third review the vitritis appeared to be settling with better definition of retinitis but his systemic status continued to deteriorate.
Discussion
Acute retinal necrosis (ARN) occurs commonly due to herpes simplex virus and varicella zoster virus. The viral inflammation is characterised by arteritis, vitritis and peripheral retinal necrosis.3
A presentation of herpetic encephalitis and retinal necrosis due to herpes simplex type 2 is rare. Encephalitis can occur either due to a retrograde spread of the virus from the eye to the brain or a reactivation in the brain. ARN has a poor prognosis unless treated early and aggressively to prevent involvement of the other eye. The presence of severe vitritis and opacification in association with central and peripheral retinal lesions posed a challenge and a diagnosis of superadded aspergillosis endophthalmitis was made based on the possibility of systemic dissemination of pulmonary aspergillosis. This we thought was due to the immunocompromised state of the patient. The violent reaction is probably also due to release of inflammatory mediators by the immune system due to viral invasion. Acute retinitis with arteritis can result in retinal detachment.4 Poor vision is due to complications such as extensive ischemia, optic atrophy or retinal detachment.5 The patient was started on systemic intravenous infusion of antivirals along with co-trimoxazole and local therapy with steroid and cycloplegic eye drops. The unique feature in this case was the simultaneous multiple organismal culture. Optic disc oedema is not a typical feature of acute retinal necrosis. The criteria provided in the classification includes peripheral retinal necrosis, positive polymerase chain reaction (PCR) assay of intraocular fluid, retinal sheathing and vitritis. This clinical classification is useful for both clinical and research purposes.6 The association between neurological herpetic infections and ARN has been reported in immunocompromised and rarely in immunocompetent patients.7 Toxoplasma retinochoroiditis mimicking retinal necrosis has been reported.8 However, a co-existence of infection with fungal invasion causing Aspergillus endophthalmitis has never been reported. Vitrectomy and surgical management may be challenging because of the systemic status.
Conclusion
This case highlights the importance of clinical suspicion of simultaneous multiple retinal inflammatory diseases due to diverse organisms. The risk of neurological involvement increases even in immunocompetent patients and worsens both ocular with visual and systemic prognosis. Early systemic medical intervention is key in the management.


