Introduction
Binocular vision (BV) refers to the coordinated work of both human eyes in perceiving a unified three-dimensional image. It plays a crucial role in our daily activities by allowing us to perceive depth and understand object relationships, which is challenging with only one eye. Binocular vision anomalies can occur due to improper eye alignment or coordination, leading to insufficient information being sent to the brain. These disorders are categorized as either strabismic (manifest) or non-strabismic (latent). Binocular vision dysfunction has become one of the most common visual problems today. Vision Therapy (VT) involves activating and training the visual system, including the eyes and a portion of the brain. Depending on the patient's condition and availability, vision therapy can be conducted at home or in an office setting. Home-based vision therapy is cost-effective, requires fewer office visits and follow-up appointments, and does not necessitate specialized equipment. A comprehensive evaluation of binocular vision should include testing for accommodation and vergence characteristics and tracking and reading eye movement metrics. However, before beginning a BV testing, appropriate refractive correction and binocular balancing are the fundamental elements.1
Digital eye strain has become increasingly prevalent as the use of digital devices has risen globally. Individuals with poor vergence and accommodation parameters are at risk of experiencing symptoms when using digital devices. Therefore, in addition to assessing ocular surface and ergonomic factors, it is crucial to analyze binocular vision.2, 3 Unfortunately, many eye care professionals still hold the misconception that having 20/20 vision ensures optimal visual system performance. However, a healthy and integrated binocular vision system is also essential for effective visual functioning, alongside the integrity of the visual apparatus and monocular visual acuity.4, 5 Therefore, a thorough binocular vision assessment is necessary even without significant refractive defects when a patient complains of undiagnosed asthenopia symptoms. Binocular vision assessment is also required for conditions such as myopia, keratoconus, amblyopia, and anisometropia.6, 7
The pandemic resulted in changes to our daily lives, with a greater likelihood of non-strabismic binocular vision anomalies due to increasing near-vision-dependent tasks. While spectacles are the primary treatment for these issues, vision therapy complements office-based therapy, alleviating symptoms and improving the patient's quality of life. Non-strabismic binocular vision disorders have become increasingly common in recent years, with a high prevalence among school-aged children, ranging from 28.5 to 31.5 percent globally.1, 2 It has also been observed that children with convergence insufficiency may have impaired stereoacuity, emphasizing the need to identify and treat this condition.3 Accurate diagnosis and appropriate care are crucial for individuals with binocular vision anomalies.
To address the increasing prevalence of binocular vision anomalies, it is crucial to have more orthoptists and vision therapists available for screening. Additionally, awareness of Vision Therapy practice among practicing optometrists needs to be raised, as it is currently low. A study on "Barriers to Vision Therapy for Michigan Optometrists" reveals that poor insurance reimbursement and the time involved in managing and working with patients were cited as the main barriers to offering vision therapy. A study on “Pattern of optometry practice and range of services in India” concluded that there is a lower involvement in providing BV services.8 Evaluation of BV parameters is very important in today’s digital world. However, there is lower involvement in BV practice. This study aims to evaluate the knowledge, attitude, and binocular vision practice of optometrists with different modes of practice in different locations in India. Thus, through this study, we can assess the barriers in Vision Therapy practice and Spread Awareness among practitioners, which is crucial for more participation in BV practice. Also, we will get an idea of how many BV practitioners are there.
Materials and Methods
This was an observational cross‑sectional self‑administered questionnaire‑based survey on the current knowledge, attitude, and practice (KAP) of BV services among optometrists with a sample size of 209. The questionnaire was circulated through social media, namely WhatsApp, Telegram, Facebook, and email, and via different optometry councils & regulatory bodies. The Inclusion criteria for the study were all the practicing Optometrists from Hospitals, private practice, optical retail, and academia who are residing in India were included in this survey. The Exclusion criteria were Diploma/ Undergraduate optometry Students who are currently pursuing their course are excluded from the survey. The study was carried out in accordance with the ethical standards outlined in the Helsinki Declaration. Figure 1 presents the study methodology's flowchart.
Designing the KAP of the BV services survey questionnaire was done freshly and newly after reviewing a few articles. The questionnaire was validated by Senior Practitioners & Professionals in the Eye health care field.
Twenty-five questions on knowledge, attitude, and practice domains were finalized. The material was examined to avoid double-barreled, deceptive, or leading questions. This structured questionnaire included the demographic details of the participants; the next section of the questionnaire assessed the knowledge about VT on a scale of 1-3(1- Basic, 2-Advance, 3-Expert), and the next nine questions determined the clinical practice of VT along with the barriers faced by the practitioners and the last section of the questions ascertained the attitude and willingness toward VT practice for those who don't provide VT services.
Participants were categorized for statistical analysis based on their knowledge, educational background, and job sector. The qualification was sub‑classified as Diploma in Optometry, Bachelor in Optometry, Master in Optometry, and Ph.D. The practicing sector was sub-classified as Private Hospital-based, Optical Retail, Government Hospital-based, Private Practice, and Academics (Having a Binocular Vision setup). The number of years of clinical experience was sub‑classified as less than 1 year, with options between 1 to 35 years and 35 or more years of clinical experience.
Statistical analysis was carried out using the statistical package for social sciences software, version 20 (SPSS Inc., Chicago IL), and graphs were built in Microsoft® Excel 2021. The number of participants (n) and percentages were used to represent discrete data. Parametric or non-parametric tests that were appropriate were run after testing for normality.
Result
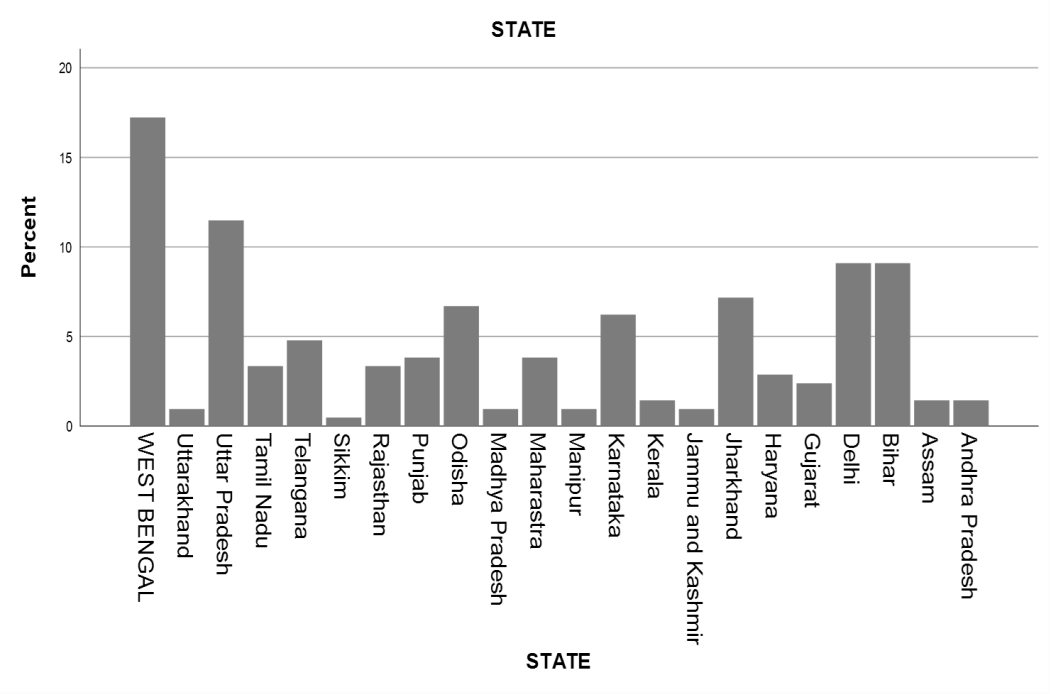
Total of 209 participants from 22 states in India completed the survey (Figure 2).
Among the participants, there were 108 males (51.7%) and 101 females (48.3%) (Table 1). The mean age of the practitioners was 26.26 ± 4.59 years.
Table 1
Male and female ratio
|
Gender |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
|
|
Valid |
Male |
108 |
51.7 |
51.7 |
51.7 |
|
Female |
101 |
48.3 |
48.3 |
100.0 |
|
|
Total |
209 |
100.0 |
100.0 |
Most respondents (57.9%) had a Bachelor's degree in optometry, while others had a Master's degree in optometry (37.8%). The participants' primary modes of practice included private hospital-based (62.7%), private practice (19.6%), optical retail (19.1%), government hospital-based (19.1%), and academics (15.8%).
Table 2
Qualification
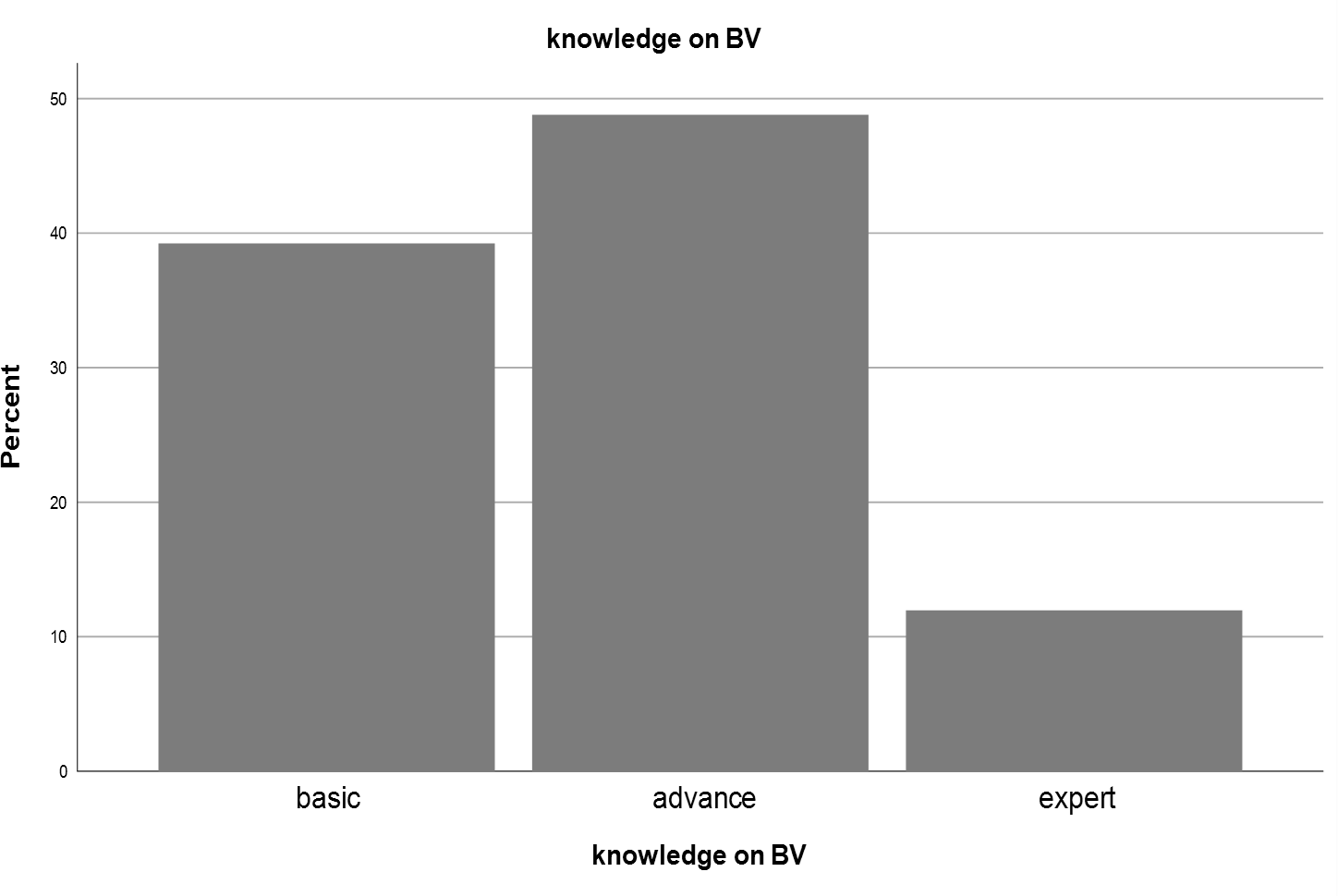
In this study, the participant’s knowledge of binocular vision and common binocular vision anomalies was classified as follows: 82 (39.2%) had basic knowledge, 102 (48.8%) had advanced knowledge, and 25 (12%) were considered experts in binocular vision (Figure 3). Regarding the years of practice, the majority of respondents reported 1 year (39.7%), followed by 2 years (18.2%) and 3 years (14.8%).
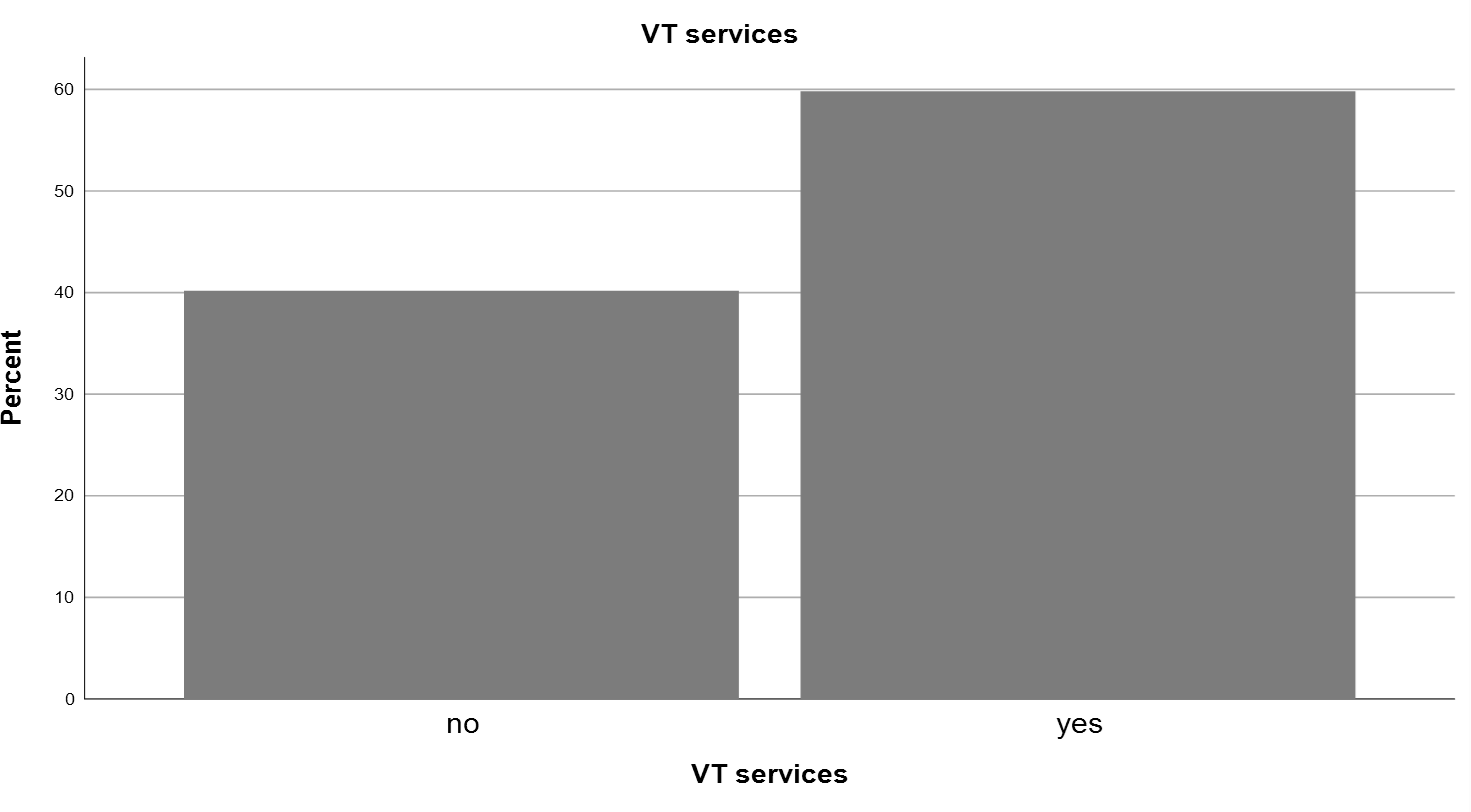
Among the 209 practicing optometrists, 125 (59.8%) provided vision therapy (VT) services, while the remaining 84 (40.2%) did not (Figure 4 ).
Out of the 125 practitioners who provided VT services, 100 (80%) stated that they had not completed any VT courses, while 25 (20%) had received training in VT. The weekly patient flow for VT services was categorized as follows: 62 (49.6%) had less than 5 patients, 33 (26.4%) had 5-10 patients, and 16 (12.8%) had 11-16% of patients.
The preferred modes of VT were combined (52.8%), home-based (24.8%), and office-based (22.4%). For the treatment of amblyopia, the VT techniques used included letter tracking with patching and home-based apps (56%), in-office and home-based VT software (40%), anti-suppression therapy using red and green filters (39.2%), patching only (38.4%), synoptophore (28.8%), monocular fixation in a binocular field (MFBF) (23.2%), therapy for eye-body coordination (23.2%), dichoptic treatment (19.2%), and cognitive therapy (17%).
Regarding vergence, the VT techniques employed were pencil push-up and dot card (79.2%), Brock string (54.4%), cat card (45.6%), in-office and home-based VT software (32.8%), life saver card (28.8%), synoptophore (27.2%), aperture ruler (20%), barrel card (19.2%), vectograms (18.4%), and stereograms (14.4%).
For accommodation, the VT techniques included distance/near Hart chart (72.8%), +/- lens flippers (67.2%), added lenses (30.4%), in-office and home-based VT software (29.6%), lens rock (25.6%), lens sorting (20%), aperture ruler (16%), and vectograms (15.2%).
Among the 125 VT practitioners, 48 (38.4%) were unwilling to disclose the charges per session. Of the remaining respondents, 31 (24.8%) charged less than 200, 20 (16%) charged between 201 and 400, 13 (10.4%) charged between 401 and 600, 6 (4.8%) charged between 601 and 800, 5 (4%) charged between 801 and 1000, and 2 (1.6%) charged more than 1000.
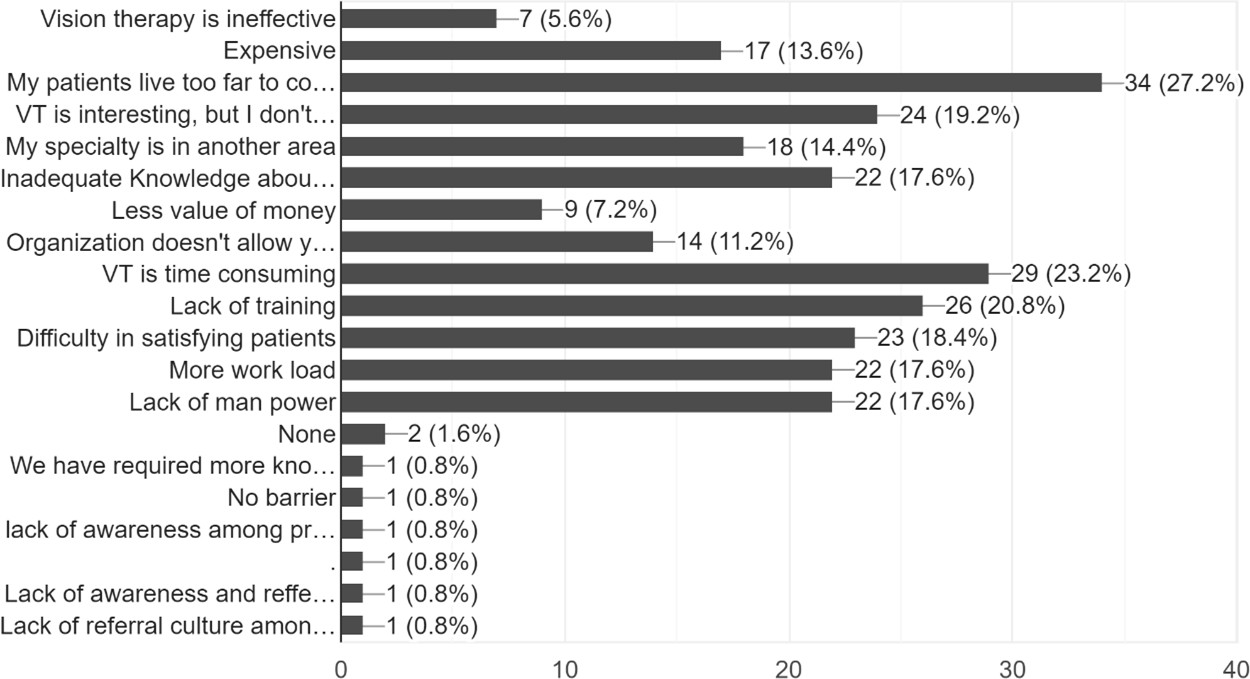
The major barriers faced by VT practitioners were patients living too far for weekly appointments (27.2%), time-consuming nature of VT (23.2%), lack of training (20.8%), unavailability of VT aids and equipment (19.2%), difficulty in satisfying patients (18.4%), increased workload (17.6%), insufficient manpower (17.6%), inadequate knowledge about vision therapy (17.6%), specialization in another area (14.4%), high cost (13.6%), organizational restrictions (11.2%), low value for money (7.2%), and perceived ineffectiveness of vision therapy (5.6%) (Figure 5).
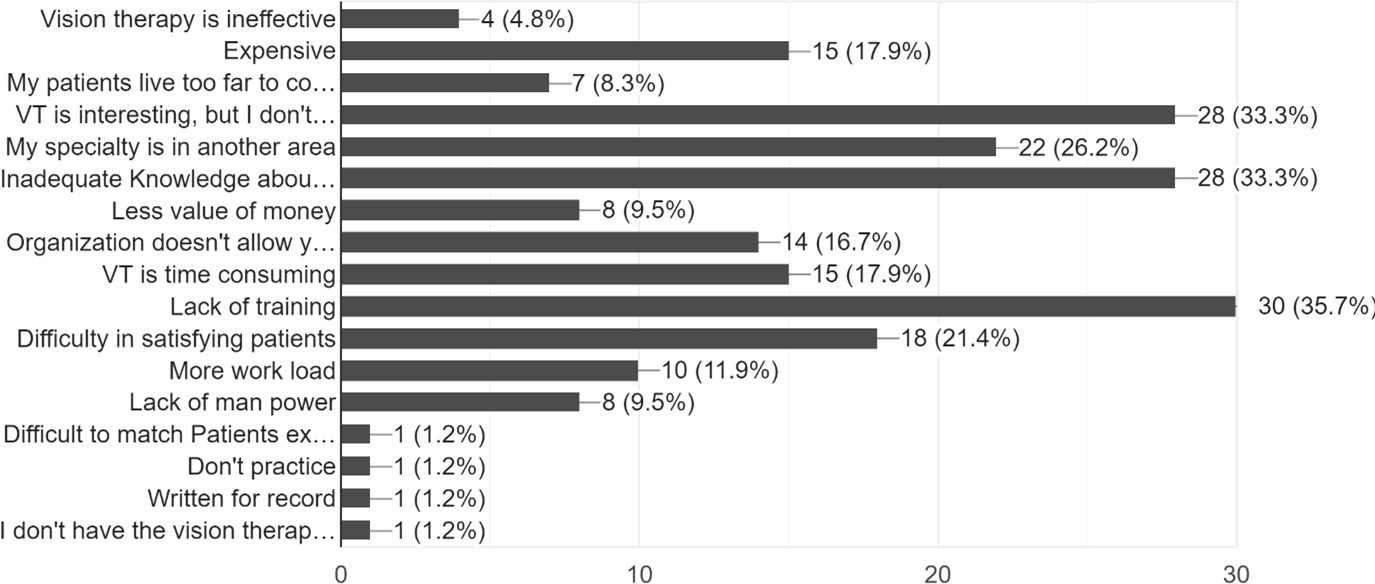
Among the 84 practitioners who did not practice VT, 67 (79.8%) referred patients for VT, while 17 (20.2%) did not. The preferred referral was to vision therapy specialists (optometrists) (83.8%), followed by ophthalmologists (16.2%). The barriers for not practicing VT included lack of training (35.7%), unavailability of VT aids and equipment (33.3%), inadequate knowledge about vision therapy (33.3%), specialization in another area (26.2%), difficulty in satisfying patients (21.4%), time-consuming nature of VT (17.9%), high cost (17.9%), organizational restrictions (16.7%), increased workload (11.9%), insufficient manpower (9.5%), low value for money (9.5%), patients living too far for weekly appointments (8.3%), and perceived ineffectiveness of vision therapy (4.8%) (Figure 6).
Among these practitioners, 66.7% expressed interest in starting VT practice in the future, and 97.6% showed a willingness to learn VT.
On doing the chi-square test, there was no association between knowledge, VT practice, and barriers to not practicing VT (p>0.05) (Table 3).
Table 3
Chi-square test between knowledge, VT practice, and barriers to not practicing VT
|
Chi-Square Tests |
|||
|
Value |
df |
Asymptotic Significance (2-sided) |
|
|
Pearson Chi-Square |
3.093a |
2 |
.213 |
|
Likelihood Ratio |
3.109 |
2 |
.211 |
|
Linear-by-Linear Association |
.725 |
1 |
.395 |
|
N of Valid Cases |
84 |
|
|
The Spearman Correlation test revealed negligible correlations between VT practice and different modes of practice (r=0.069) (Table 4), VT practice and different locations (r=0.070) (Table 5), and knowledge and qualification (r=0.69).
Discussion
The increased digital time and lifestyle changes contribute to the rising prevalence of BV anomalies.9 To address these issues effectively, more VT practitioners are required. However, there has been a lack of studies examining VT's knowledge, attitude, and practice among practicing optometrists in India. In this study, we present findings based on 209 participants from 22 states in India, revealing that 59.8% of optometrists practice VT. The educational qualifications of the respondents were primarily Bachelor's in optometry (57.9%) and Master's in optometry (37.8%). The predominant practice setting for these practitioners was private hospital-based (62.7%). Regarding knowledge of BV, the practitioners demonstrated varying levels of proficiency: basic (39.2%), advanced (48.8%), and expert (12%). Most 80% reported not having undergone any VT training, and the most preferred mode of VT was combined vision therapy (52.8%). For amblyopia, the primary VT techniques provided were letter tracking with patching and home-based apps (56%); for vergence, pencil push-up, and dot cards (79.2%); and accommodation, distance/near Hart charts (72.8%). The top three barriers faced by VT practitioners were patients living too far for weekly appointments (27.2%), the time-consuming nature of VT (23.2%), and lack of training (20.8%).
Among the practitioners who did not practice VT (40.2%), a majority (79.8%) referred their patients for VT, primarily to vision therapy specialists (optometrists) (83.8%). The main barriers to not practicing VT included lack of training (35.7%), unavailability of VT aids and equipment (33.3%), and inadequate knowledge about vision therapy (33.3%). Interestingly, 66.7% of non-practicing optometrists expressed an interest in starting VT practice in the future, and 97.6% indicated a willingness to learn VT. These findings highlight a very positive attitude towards VT practice. In a study conducted by Thite et al., it was observed that there is limited involvement in providing BV services, with the major job profiles being hospital-based (44.8%), academia (42.8%), and optical retail (33.0%).8 Another study by Pearson et al. reported that only 39% of practitioners incorporate VT into their practice, indicating a favorable attitude towards VT. 10 The primary barriers to not offering VT services, as identified by Fordyce et al., were poor reimbursement through insurance and time constraints associated with managing and working with patients.11
Conclusion
Practitioners possessed both basic and advanced knowledge of binocular vision (BV). More than 50% of them actively practice vision therapy (VT), while those who do not practice VT display a positive attitude, with 97.6% expressing willingness to learn and begin practicing it. The primary barrier preventing non-practitioners from engaging in VT is the lack of proper training. The Convergence Insufficiency Treatment Trial (CITT) has extensively established the scientific validity of vision therapy through specific and compelling findings, demonstrating its efficacy when implemented using a systematic approach.12 Eye care professionals must embrace evidence-based practice patterns and remain open to exploring innovative solutions that can significantly improve patient compliance. Thanks to affordable local instruments, clinicians can now easily assess and treat binocular vision problems. In the modern digital era, evaluating binocular vision parameters is important.13, 14, 15, 16 Several articles have highlighted a decline in engagement within the field of binocular vision (BV) practice, emphasizing the need for a deeper understanding of the barriers contributing to this reduced involvement.12, 17 To effectively address BV-related issues and develop a comprehensive understanding of the current BV practitioner population, it is crucial to increase the number of BV and vision therapy (VT) practitioners.18 Promoting awareness of vision therapy among practitioners plays a vital role in encouraging greater participation in delivering binocular vision services.
Limitation
The limitations of this study include limited response. One primary reason was the target population's reluctance to participate. Additionally, the survey link often failed to reach the intended audience. Some survey responses remained incomplete because certain questions were difficult to understand.