Introduction
Dry eye disease (DED) is a common ocular condition characterized by insufficient tear production or excessive tear evaporation, leading to discomfort and visual disturbances.1 It affects approximately 10% to 20% of adults worldwide.2 Epidemiological research has reported global estimates of DED ranging from 5% to 50%.3 In India, the prevalence of DED is even higher, varying from 18.4% to 54.3%, surpassing the global prevalence.4, 5
DED is characterized by subjective symptoms such as ocular pain, dryness, visual impairment, and soreness. Objective symptoms include tear film instability, ocular surface irritation, and hyperosmolarity.6, 7 Aqueous deficiency, resulting in lower tear production, and evaporative dry eye, causing increased tear film evaporation, were the two prevalent classifications for DED.8, 9 Artificial tears and topical lubricants are the primary treatment options for aqueous deficient DED, providing relief by supplementing and stabilizing the tear film.10, 11 Carboxymethyl cellulose (CMC) and Hyaluronic acid (HA) are the most frequently prescribed and utilized artificial tear formulations, despite the existence of numerous other viable alternatives.12 However, there have been reports suggesting that Polyethylene glycol and Propylene glycol (PEG-PG) combination lubricating eye drops was superior to CMC for DED cases.13 In a well-defined and homogeneous group of individuals with DED, sodium hyaluronate (SH) has shown a positive impact on the conjunctival epithelium, recommending it as an effective treatment option for dry eyes.14
Large-scale clinical trials have demonstrated the effectiveness of both CMC and HA in reducing the signs and symptoms of DED. Various techniques, such as tear break-up time, corneal or conjunctival staining, Schirmer test, and dry eye symptom score, have been used in studies to assess the efficacy of CMC and HA, aiming to determine the most successful therapy.12, 15, 16, 17 While some studies suggested that CMC and HA were equally effective in treating DED, other studies have shown that one treatment option outperforms the other. Additional studies have compared the safety and efficacy of sodium hyaluronate (SH) with CMC, as well as the effects of polyethylene glycol and propylene glycol (PEG-PG) with hydroxypropyl guar in hyperosmotic stress-based explant models for mild to moderate DED treatment.12, 18, 19 Physicians should be aware of the active ingredients of artificial tear formulations to guide their initial selection and potential later transition to products containing additional biologically active chemicals or belonging to different classes with different active ingredients.
The current questionnaire-based survey examined the prevalence of DED and the prescription practices of the artificial tear formulations for the treatment of mild, moderate, severe, or very severe DED cases in Indian settings.
Materials and Methods
We carried out a cross-sectional, multiple-response questionnaire based survey among clinicians specialized in treating dry eye disease (DED) patients in the major Indian cities from June 2022 to December 2022.
The questionnaire booklet titled DESQ (Dry Eye Study Questionnaire) study was sent to the physicians who were interested to participate. The DESQ study questionnaire included questions on the current practices, preferences, clinical observations, and experiences related to the use of artificial tear formulations in routine settings, for the management of DED. The study was conducted after receiving approval from Bangalore Ethics, an Independent Ethics Committee which is recognized by the Indian Regulatory Authority, Drug Controller General of India.
An invitation was sent to leading ophthalmologists in managing DED in the month of March 2022 for participation in this Indian survey. 54 doctors from major cities of all Indian states representing the geographical distribution shared their willingness to participate and provide necessary data. Physicians were asked to complete the questionnaire without discussing with peers. A written informed consent was obtained from each ophthalmologist prior initiation of the study.
The data were analyzed by using descriptive statistics. Percentages were used to represent categorical variables. The frequency and percentage distribution was used to represent the distribution of each variable. Pie and bar charts were made using Excel 2013 (16.0.13901.20400).
Result
Out of the 54 respondents, 59% reported that dry eye disease (DED) was prevalent in both genders. However, the gender-specific distribution indicated increased preponderance in women (29.63%) compared to men (11.11%). Nearly half of the respondents reported that professionals with computer exposure were more commonly affected by dry eyes. Around 38.88% of respondents disclosed that individuals who spend a significant amount of time working on computers or other digital devices as part of their profession suffer from dry eyes. Approximately 7% of respondents stated that housewives at home also suffer from the same disease.
According to the data, the majority of participants (62.96%) reported that individuals within the age group of 25 to 40 years were more frequently affected by DED. Approximately 29% and 7% of the participants reported the occurrence of the disease in the age groups of more than 40 years and 15 to 25 years, respectively. Around 37.04% of the respondents reported that the diagnosis of dry eyes relies on the Schirmer score, while 29.63% of them indicated that a slit lamp examination was used for diagnosis. In some cases, a comprehensive diagnosis of dry eyes may require utilizing all of the mentioned techniques, as reported by 14.81% of the respondents.
Around 48.15% of the respondents reported diagnosing approximately 26-50% of individuals with aqueous-deficient dry eye. Additionally, 31.48% of them reported diagnosing 51-75% of individuals with the same disease. Around 51.85% of respondents reported that the proportion of subjects noted with evaporative dry eye syndrome was between 26-50%, while 22.22% of respondents reported its occurrence in 51-75% of patients as depicted in (Table 1).
Table 1
Patients with DED diagnosed with aqueous-deficient and evaporative dry eyes
Around 77.77% of respondents denoted the sensation of burning or stinging in the eyes as a major symptom of aqueous-deficient dry eyes in patients previously diagnosed with DED. Symptoms such as itchy eyes, eye pain, and the occurrence of all the above-mentioned symptoms were reported by a minor proportion of respondents.
Approximately 51.85% of the participants recommended CMC at a concentration of 0.5% as the first-line treatment for dry eyes, while 27.77% of individuals favored CMC at a higher concentration of 1.0%. For managing moderate dry eyes, around 44.44% of individuals preferred combination eye drops containing PEG-PG as the first-line treatment.
Nearly 68.52% of the responders preferred prescribing SH eye drops as the first-line treatment for patients with severe dry eyes. Around 27.77% of responders prescribed combination eye drops containing PEG-PG as shown in (Table 2 ).
Table 2
Preferred first-line of treatment choices based on the severity of DED
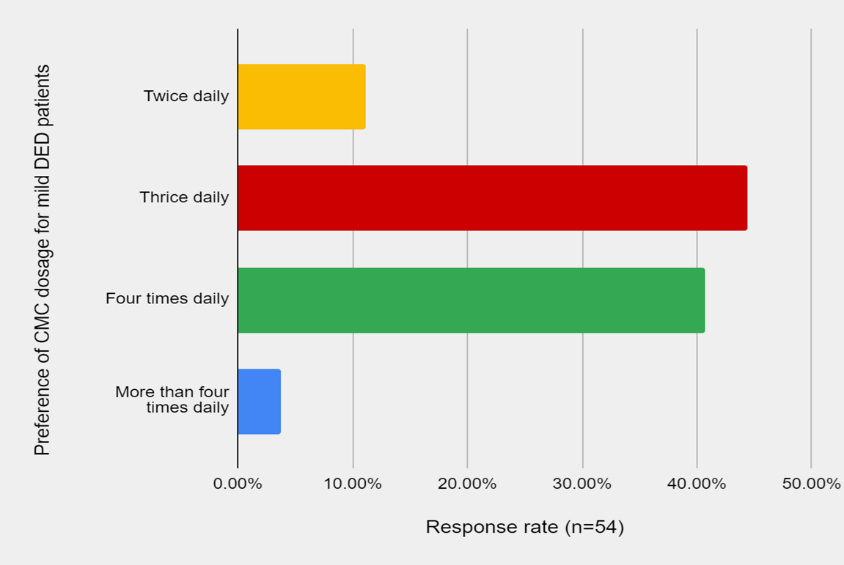
The majority of the respondents (92.59%) reported achieving good clinical outcomes by adopting a comprehensive approach that includes regular use of prescribed medication, minimizing digital exposure, following the 20-20-20 rule, and considering lifestyle factors such as diet and exercise. Approximately 5.55% of respondents reported good clinical outcomes by following the 20-20-20 rule alone. Around 44.44% recommended the use of CMC eye drops three times a day as treatment for mild DED. Around 40.74% of respondents advocated CMC eye drops four times a day, while 11.11% preferred using the eye drops twice daily (Figure 1).
Approximately 44.44% of responders stated the need for patient educator sessions every three months, while 31.48% reported their need on a monthly basis. Around 14.81% of respondents reported the need for the session every two months, and 9.26% reported the need for it once every six months. Approximately 48.15% of clinicians reported that they may advise to switch from CMC eye drops to SH eye drops. About 31.48% of responders may recommend patients to switch from CMC 0.5% to a higher concentration of 1.0%. However, 14.81% of them reported that they may switch the medication from CMC to a Trehalose-based eye drop (Figure 2).
Figure 2
Preferred treatment strategy for patients who fail to respond to carboxymethylcellulose 0.5% eye drops for managing dry eyes
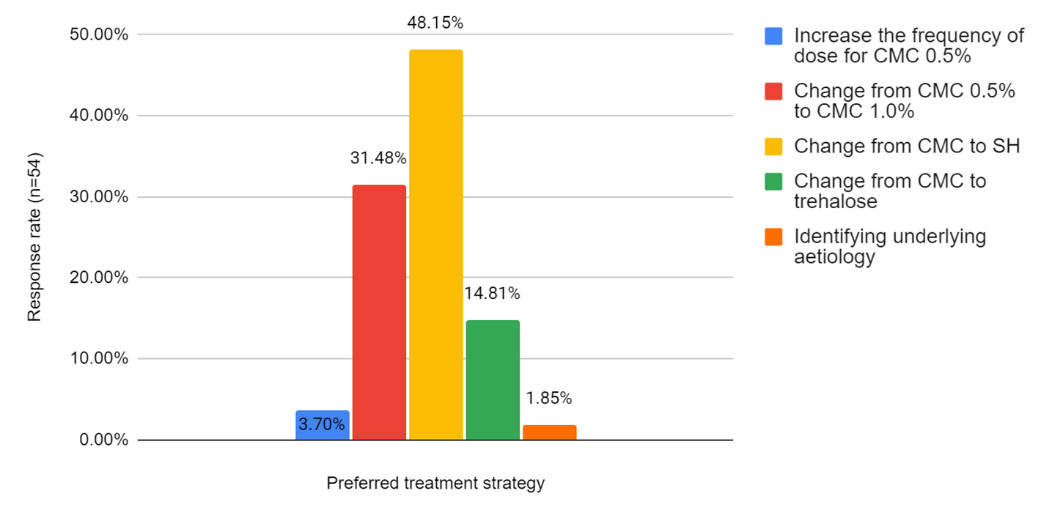
Table 3
Recommendation of artificial tear formulations for the management of DED based on severity
The majority of the respondents (62.96%) recommended the combination of PEG and PG to patients with moderate DED, while 29.62% of the respondents stated that they would recommend this combination specifically to patients with severe DED. Approximately half of the responders preferred hydroxypropyl Methyl cellulose eye drops for patients with mild DED, while 37.03% of responders preferred them for patients with moderate DED. About 64.91% of responders recommended SH eye drops to patients with the severe DED. Approximately 18.52% and 16.66% of responders recommended SH eye drops for patients with moderate and severe to very severe DED respectively (Table 3).
Discussion
The current study sheds light on the perspectives of clinicians regarding the treatment of DED in an Indian context. The findings were obtained through a rigorous and validated questionnaire-based survey, which allowed experts to provide recommendations based on best practices supported by data. The majority of the current study respondents emphasized the importance of medication adherence as a crucial factor in achieving successful therapeutic outcomes in DED. By offering customized treatment options, it is possible to optimize therapeutic benefits and enhance patient satisfaction in managing DED.
A notable finding from the study was that a significant number of participants recommended the use of 0.5% CMC eye drops for patients with mild DED. Additionally, a considerable number of participants also recommended the use of 1% CMC eye drops and SH eye drops for patients with moderate DED. It was worth mentioning that a previous study has reported CMC to be more effective than HA in treating dry eye conditions. This data further underscores the efficacy of 0.5% CMC eye drops as a potential therapeutic option for patients with mild DED, emphasizing the importance of tailored strategies based on the severity of the condition to achieve optimal therapeutic outcomes. 20
By moisturizing the eyes and providing lubrication, the combination of PEG-PG has shown to be more effective than CMC in treating individuals with DED.19 The current study suggests the use of PEG-PG combination eye drops for patients with moderate DED, while SH eye drops for those with severe DED. Artificial tears containing PEG+PG 400 have been shown to significantly reduce corneal staining, indicating a decrease in the severity of dry eye symptom. 21 Aguilar et al. found that the use of PEG+PG-based artificial tears increased goblet cell density, reduced corneal and conjunctival staining, and improved tear film break-up time in individuals with DED. 22 Previous studies has demonstrated the beneficial effects of PEG/PG-formulated artificial tears in alleviating signs and symptoms of dry eyes including photo phobia, conjunctival hyperemia, burning, tearing, foreign body sensation, and ocular surface injury.13, 23, 24, 25
Nearly half of the respondents in the study recommended switching from CMC to SH eye drops. This recommendation aligns with previous research indicating that SH-based ophthalmic treatments can normalize clinical parameters and alleviate symptoms in individuals with DED.26 Several studies have reported significant improvement in patients with mild and severe DED after using sodium hyaluronate, supporting the effectiveness of this treatment option.27, 28, 12 However, some respondents suggested switching from CMC 0.5% to a higher concentration of 1.0%. Lee et al. found that both SH and CMC were effective in treating mild to moderate DED patients.12 Another study by Lee et al. showed that CMC therapy significantly improved mild to moderate DED.12 By considering these findings, healthcare professionals can make well-informed decisions regarding the most effective treatment options, ultimately leading to improved patient outcomes in the management of DED.
By focusing on a specific population, the study offers context-specific information that can be relevant for healthcare professionals working with DED patients in similar settings. The study highlighted the significance of medication adherence and customized treatment options for DED. The study's rigorous methodology, context-specific insights, and emphasis on personalized care contribute to its strength and relevance in the field of DED research and clinical practice. It is important to acknowledge certain limitations of the study. The relatively small sample size used in this study may limit the generalizability of the results to a larger population of individuals with DED. A larger and more diverse sample could provide a more accurate representation of the entire DED population. Additionally, the reliance on expert judgment in the study introduces the potential for bias, as different perspectives and preferences may have influenced the reported findings. It is essential to consider these limitations when interpreting the results and to conduct further research to validate and expand upon the findings.
Conclusion
Experts recommended the use of CMC eye drops to provide short-term relief from irritation and pain caused by eye dryness, wind exposure, or sun exposure. Additionally, ophthalmologists strongly recommend the prescription of CMC at a concentration of 0.5% to patients with mild DED, to be administered three times daily. For patients with moderate DED or those who have not responded well to a lower dosage, a higher concentration of 1.0% may be prescribed. However, further research is needed to elucidate the precise mechanism of action of CMC in the treatment of DED.