Introduction
Cataract surgery is most commonly performed intraocular surgery in the world.1 Manual small incision cataract surgery is frequently performed surgery in developing countries. Technical refinements in past 2 decades have led to faster visual recovery and better postoperative care, still post-operative endophthalmitis has been reported with an incidence of 0.04% to 0.41%.2 Endophthalmitis is characterized by marked inflammation of intraocular tissues with inflammatory exudation into the vitreous.3
Cluster endophthalmitis is termed when 5 or more cases of endophthalmitis occur on a particular day, in a single operating room at one centre.4 The incidence of post-cataract surgery endophthalmitis has decreased over time due to better standards of operation theatre sterilization, improved preoperative patient work-up, refined surgical techniques, and better postoperative care.5, 6, 7 Despite declining numbers of endophthalmitis, situations like cluster endophthalmitis have occurred which is a challenging situation for patients as well as doctors/clinicians/organisers to manage. It is possible, to salvage the eye with early diagnosis and appropriate management.8
The final outcome in endophthalmitis depends on various factors like time of presentation, etiology, quick diagnosis and initiation of treatment. Proper management may salvage the eye but can still result in poor visual outcome. The sequelae of endophthalmitis affect the quality of life of patient because of blindness and disfigurement. Therefore, the responsibility as caregivers does not end at diagnosis and treatment but also to properly identify and manage the operational difficulties related to eye healthcare delivery, starting from home-based care to tertiary care, that influence the visual outcome.
Materials and Methods
A retrospective study done on 64 cases presented with features of endophthalmitis out of 94 patients operated for cataract surgery in an eye camp setting which took place in Central India in Madhya Pradesh in November 2015. Demographic details, detailed history, clinical presentation, management and final outcome was evaluated in these 64 patients who presented with features of endophthalmitis after getting operated in a high-volume cataract surgery camp over three days. The study was approved by the Institutional Ethical Committee (IEC no. SAIMS/IEC/2017/02/06) and in adherence to the tenets of Declaration of Helsinki.
Data collection: The case records were collected from the institutional medical records between 3rd November 2015 to 30th November 2015 which was the duration of presentation of 64 patients. Treatment charts of patients were retrieved using patients’ registration card number which was found in database system. The information was first observed and analysed. It was further discussed with healthcare service providers at local level. All important information was collected by the health care service providers after theoretical and practical orientations.
Clinical presentation: 64 out of 94 cases operated for cataract surgery presented at tertiary care center from 7th to 30th postoperative day with signs and symptoms consistent with diagnosis of endophthalmitis. The chief complaints at presentation included no improvement in visual acuity after surgery or deterioration in vision after cataract surgery associated with ocular pain, redness and excessive watering of eyes. All patients underwent detailed ophthalmic assessment including visual acuity, slit-lamp examination, dilated fundus evaluation and B-scan ultrasonography (USG).
Microbiological investigation: Samples from each patient were collected for microbiological examination. The samples included vitreous aspirate, aqueous, conjunctival swabs, corneal scrapings, IOL and eye drops of the patient. A total of 123 samples were collected. All samples were processed for gram stain, 10% KOH smear, bacterial culture on blood agar and MacConkey agar while fungal culture on Sabouraud dextrose agar with and without chloramphenicol.
Intervention: Intervention was done on the basis of EVS study. Depending on clinical status and investigative results, the intervention modality was decided which included – intravitreal antibiotics, intravitreal injection of antifungal agent, vitrectomy with silicone oil, re-suturing of the open wound, anterior chamber wash, IOL explanation, and evisceration. Intravitreal antibiotics was given to all patients without waiting for culture and sensitivity reports as recommended by the EVS.8
All eyes received intravitreal vancomycin (1 mg in 0.1 ml) and ceftazidime (2.25 mg in 0.1 ml). All 64 cases were admitted in isolation ward and given intravenous ceftriaxone with sulbactam in a dose of 1.5 gm every 6 hourly, intravenous vancomycin in a dose of 500 mg every 6 hourly along with supportive medications. Topical medications were prescribed which included fortified tobramycin 1.4% every hourly, fortified cefazolin 5% every hourly and atropine 1% 8 hourly. Antifungal therapy was started in cases with positive KOH smear and/or culture. Systemic intravenous voriconazole in a loading dose of 6 mg/kg every 12 hours and then switched to maintenance dose of 4 mg/kg every 12 hours. Intravitreal injections of voriconazole (100 µg in 0.1 ml) and voriconazole 1% eye drop hourly were given.
The patients were closely monitored for response to the treatment. Patients with severe anterior segment involvement were first taken for anterior chamber wash while few patients required IOL explantation. Patients with no clinical improvement by intravitreal injection were taken for pars-plana vitrectomy with or without silicon oil insertion. Topical and systemic medications were continued for four weeks. At the time of discharge, the best-corrected visual acuity was recorded for each patient. They were advised topical medications with one weekly follow-up.
Results
A total of 64 cases consistent with features of endophthalmitis were studied. The present study showed mean age of 60 ± 15.3 years which had 31(48.4%) males and 33(51.6%) females. The period between onset of symptoms and presentation was variable from 7th to 30th day and cause of delay in presentation was analysed with detailed history and leading questions attributing to various problems faced by the patient during this period (Table 1). No patient reported till 7th postoperative day. A note of most frequently encountered problems were noted as shown in Table 1. 31(48.4%) cases out of all 64 cases reported in 2nd post-operative week from 8-14th postoperative day due to attitudinal barriers. 19(29.6%) cases reported in 3rd week from 15-21st postoperative day. 14(21.8%) cases reported in 4th week due to ignorance of alarming signs and causing time-lapse and delay in presentation.
Table 1
Day of presentation and the most common reasons for delay in presentation
The visual acuity of all 64(100%) cases at presentation was extremely poor, out of which 59(92.2%) patients had only handed movement to perception of light while 5(7.8%) denied perception of light. All 64(100%) patients presented with diminution of vision as compared to their preoperative visual status or no improvement in vision after the surgery with redness in 64(100%) patients and pain in 45(70.3%) patients. There were associated symptoms of watering, discharge and foreign body sensation as shown in Table 2.
Table 2
Clinical presentation with variable symptomatology
|
Symptoms |
No. of patients |
Percentage |
|
Diminution of vision |
64 |
100% |
|
Pain |
45 |
70.3% |
|
Red eye |
64 |
100% |
|
Watering |
21 |
32.8% |
|
Discharge |
9 |
14.1% |
|
Foreign body sensation |
16 |
25% |
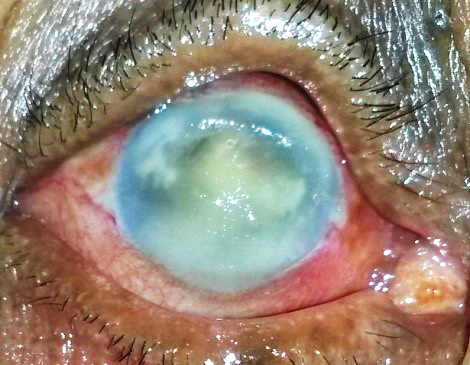
The detailed ophthalmic examination showed various features which included anterior segment inflammation with extensive corneal involvement (Figure 1), wound gape (Figure 2), scleral melt (Figure 3), hypopyon, exudates over the IOL and in the pupillary area. The extensive corneal involvement was a limitation for posterior segment examination. Fundus evaluation was possible only in 15(23.4%) patients thus dilated fundus examination of patients did not yield any additional information. Corneal edema, endothelial plaques and exudates on IOL were major barriers obstructing visibility for complete clinical examination.
Ultrasonography was performed for posterior segment examination. B-scan showed multiple small echogenic mobile opacities scattered in vitreous cavity showing low to medium reflectivity suggestive of vitritis. However, no patient had retinal detachment or choroidal detachment. The detailed clinical features are shown in Table 3.
Table 3
Clinical features with variable signs on presentation
The detailed evaluation of cornea at presentation was important to understand the response of treatment. As corneal involvement caused visibility issues therefore surgical management was a big challenge. All cases (100%) have variable corneal involvement at presentation as shown in Table 4.
Table 4
Corneal status of patients at presentation
A total of 123(100%) samples were collected. Gram stain showed pus cells in 63.4% of samples. It showed gram-positive cocci in 50(40.6%) samples and 3(2.4%) samples had presence of gram-negative bacilli. 10% KOH smear showed branching septate fungal hyphae in 75(60.97%) specimens.
The cultures were positive in 43(67.18%)cases. Fungal growth (Aspergillus fumigatus) was reported in 31(48.43%) patients. Bacterial growth was seen in 12 (18.75%) cases which reported gram-positive cocci (Staphylococcus epidermidis n = 6, Staphylococcus aureus n = 4) and gram-negative bacteria (Klebsiella pneumoniae n=2).
All patients received intravitreal injections of vancomycin and ceftazidime as the first line of management (Table 5). Three (4.7%) patient showed clinical improvement with a single dose of intravitreal antibiotic injection. 44(68.75%) cases tested positive with confirmed fungal filaments on microscopy and culture report showed presence of Aspergillus fumigatus. Intravitreal injection of voriconazole was given to them. 12(18.7%) patients required multiple intravitreal injections.
Vitrectomy was possible only in 30(46.9%) cases due to poor visibility. There were few other limitations for restricted surgical intervention like corneal haze and exudates in the anterior chamber, wound gaping at incision site, and scleral melting. Poor visualization permitted only limited vitrectomy and the endpoint of vitrectomy was optic nerve head visualization. Inflamed blood vessels and exudates adhering to the retina were seen in cases that allowed visualization (6.7%). Silicone oil was injected in 28(93.33%) out of 30 cases.
Table 5
Showing types of intervention strategies for management of cluster endophthalmitis
The final outcome showed clinical improvement in all the cases. The final visual outcome showed improvement in 6(9.4%) patients with better than Hand movement (HM) but less than 6/60. There were 5(7.8%) patient presented with no perception of light and later had a downhill course had to undergo evisceration eventually. Rest 59(92.2%) patients had only marginal improvement in vision from baseline, but all 64(100%) patients showed clinical and symptomatic improvement at the time of discharge as shown in Table 6 .
Discussion
Cataract is still the most prevalent cause of blindness in India despite availability of cost-effective treatment.9 Eye camps are successful in combating ocular morbidity load of society. However, the major concern in high volume surgical eye camps is cluster endophthalmitis. There have been incidences in past with poor outcomes affecting lives from such devastating tragedies.10 It is prudent for eye care provider to analyse, rectify mistakes, short comings with a motive to develop and adapt standard management and administrative protocols to improve upon their surgical eye camp delivery system. This study was aimed to assess the clinical features and manage postoperative endophthalmitis and to identify operational difficulties in surgical eye camp setting.
One of the most feared complications after cataract surgery is postoperative endophthalmitis. Timely detection and prompt management can salvage eye and restore vision, but still endophthalmitis may have a grave prognosis on visual outcome which depends on various factors.11 The unfavourable visual outcomes may range from decreased visual acuity to less than 20/200 or even warrant evisceration/enucleation in hopeless cases. There is no doubt that endophthalmitis elicits distress and loss in quality of life and also increases burden on patients and healthcare system/organizations.
The incidence of endophthalmitis post cataract surgery in the Indian scenario is 0.05%.12 The incidence of post-operative endophthalmitis has decreased over time with efficient health care delivery system, awareness, better standards of operation theatre sterilization, improved preoperative patient workup, cautious surgical techniques and meticulous postoperative care.13 However, cluster endophthalmitis still remains a dreaded complication of cataract surgery despite the advancements and developments which is devastating for patients, surgeons and health care system.
In present study, 94 patients underwent small incision cataract surgery at primary camp setting of which 64 patients reported with endophthalmitis at tertiary care centre. A retrospective observational study done at Aravind Eye Hospital found a higher incidence of endophthalmitis after manual SICS (0.12%) than after phacoemulsification (0.03%).7 In current study, the patients patients had variable time of onset of symptoms and varying time of presentation, from 7th to 30th postoperative day, at tertiary care centre. All cases had corneal involvement that caused difficulty in ocular examination and surgery. Out of 64 cases, fundus examination was possible in 15 cases (23.4%) and in remaining 49 (76.6%) patients B-scan ultrasonography was used to assess the posterior segment. There are various factors implicated for the severity of endophthalmitis which include time-lapsed between onset of symptoms and intervention, delay in early intervention, polymicrobial etiology and postoperative care and hygiene.14 An early intervention in terms of microbiological sampling and intravitreal injection could have improved the quality of care.8
Treatment of infected eyes was on the lines of endophthalmitis vitrectomy study (EVS) recommended standard of care.15 Accordingly, outcome was depended on early intervention, the speed of instituting treatment, a good vitrectomy and susceptibility of infecting microorganism. According to EVS, 94.1% of cases are caused by gram-positive bacteria and 5.9% by gram-negative bacteria.8 Indian studies have reported 10-54% cases with gram-positive cocci, 26-42% with gram-negative bacteria and fungal etiology in 16-22% cases of postoperative endophthalmitis.16, 17, 18 In present case series, fungal etiology (Aspergillus fumigatus) was the leading cause of endophthalmitis (n=44, 68.75%) followed by gram-positive bacteria (Staphylococcus). Aspergillus causes a more aggressive disease compared to yeasts and has a poor prognosis.19, 20, 21 Although, exogenous aspergillus endophthalmitis is rare but is identified as most common form of postoperative fungal endophthalmitis.22, 23 Literature from past have shown that fungal endophthalmitis is always difficult to treat and has a dismal visual prognosis. In the present study, positive microbial culture was found in 25(39.06%) vitreous samples. Studies have shown that culture positivity is not possible in all cases of endophthalmitis due to various reasons such as duration of presentation, improper sample collection, initiation of treatment before sampling and inaccessibility to the laboratory on time. Only 41.66-69.3% cases of suspected endophthalmitis turn positive on culture report. Similarly, in present study we found low level of culture positivity despite encountering situation of cluster endophthalmitis. In cluster endophthalmitis source of infection is exogenous and multifactorial.4, 12 In a recent meta-analysis most common source identified was intraocular inoculation of infective agent.24 In endophthalmitis, virulence of the organism plays an important role in determining the visual outcome.12 In current case series , the root cause behind the major mishap could not be traced because of the lack of proper microbiology and laboratory services in the vicinity of the area where the surgeries were performed.
According to EVS, management of post-operative endophthalmitis is primary vitrectomy in cases with profound visual deterioration (less than HMCF) and intravitreal antibiotic injection after intraocular fluid aspiration for culture and sensitivity for cases with visual acuity equal to or greater than HMCF.8 In a previous study,45 eyes were managed by primary vitrectomy, vitreous tap and intravitreal injections at the first presentation. None of the eyes needed evisceration or enucleation and all were salvaged with good visual outcomes.25 In the present study, all patients(100%) received intravitreal injections of vancomycin and ceftazidime as the first line of management at tertiary care center. The surgeries were performed depending on the day of presentation. 30(46.9%) out of 64 cases did not respond to intravitreal antimicrobial injections and required vitrectomy with or without silicone oil tamponade. Poor visualization permitted only limited vitrectomy and the endpoint of vitrectomy was optic nerve head visualization. Silicone oil was used liberally in 93.33% of eyes which underwent vitrectomy to control intraocular infection due to its antimicrobial property.26 Some patients required re-vitrectomy, anterior chamber wash with removal of IOL. However, five patients had to be eviscerated because of the worsening of endophthalmitis to panophthalmitis despite intervention.
The post-treatment outcome in endophthalmitis depends on several factors. One of the significant determinants of outcome is the time of first point of intervention from diagnosis.8 As reported by EVS, patients who present early have a better visual outcome in post-cataract surgery endophthalmitis. In our study, the patients were treated according to the guidelines but still, the visual outcome was dismal, only 6(9.3%) patients showed symptomatic visual improvement. This can be attributed to various factors including early intervention in terms of prompt intravitreal injection, delay in reporting, delay in arrival to tertiary care hospital and polymicrobial etiology of endophthalmitis.
The purpose of the current retrospective study was also to assess the operational difficulties and problems faced by the patients and caregiver. Timely intervention could have made the outcome better. We found delays related to decision making, identifying and reaching health care services, and receiving adequate and appropriate care. There could be several reasons for this poor visual outcome apart from delay which include aggressive nature of Aspergillus fumigatus infection, polymicrobial nature of intraocular infection, severe corneal involvement causing difficulty in visualization of intraocular structures and poor patient compliance to follow up as the patients were from tribal background, hailing from remote areas with poor accessibility, and had very low socio-economic status.
India is a diverse country with distant connectivity. It has a wide geographical area and peculiar terrain like Himalayan region, North East areas, remote areas of central India and islands like Andaman have a difficult outreach. Ophthalmic problems also vary according to the geographical terrain. The lack of connectivity and trained staff in areas of difficult outreach is one major lacking in connecting remote areas with standard medical care and can affect patients even after successful outreach of an eye camp.27 This also creates a burden on healthcare system as primary care cannot be initiated well on time specifically in situations like cluster endophthalmitis where it’s a race against time for early detection and where prompt intervention is the key. The current retrospective study found delays in treatment which could have been prevented as none of the patients had accessibility for prompt intravitreal injection. In endophthalmitis, primary intervention should be an empirical intravitreal antibiotics and sample for microbiological clue so as to prevent further ocular damage.8 Literature from past suggests that immediate intravitreal injection on suspicion of endophthalmitis reduce the incidence and may prevent further deterioration.28 Lack of immediate intravitreal injection at earliest point created a time-lapse in intervention that might have affected final visual outcome. Studies from past have also suggested major cause of delay which included availability of emergency services, immediate operation theatre availability, availability of intravitreal medications, proper communication between the patient and doctor.29
Numerous perioperative procedures have been attempted in past to avoid these serious complications. 30 The use of antibiotic prophylaxis protocol is commonly proposed preventive measure with different route of administration (topical, intraocular, subconjunctival, oral, intravenous) and timing (preoperative, intraoperative, perioperative, postoperative).31
The major obstacles in delivering high-volume cataract surgery may not always be technical or clinical, but can be administrative and logistical. In the present study, time to seek immediate medical assistance was delayed. All patients(100%) reported after 7th post-operative day of surgery. Patients faced difficulty in decision making, attitudinal problems and had missed alarming sign for any rapid intervention. The barriers posed were immediate transport access, distance to eyecare provider, gender-specific differences in cultural status.32 The inaccessibility to roads, isolated terrains, transportation, travel distance and patients’ awareness were other factors responsible for the delay.29
A study from past had also highlighted barriers even for uptake of refraction services in rural areas of India.32 Here it is important to highlight the financial crunch on patients which could have caused the delay in decision-making. It is a big task for patients of low socio-economic status to reach a tertiary care centre from tribal area. The timely identification of alarming symptoms and decision for seeking medical assistance are also dependent on patient and family. Poor vision, pain and discomfort cause both psychological as well as financial disturbance. Effective emergency care is dependent on patient's or caregiver's ability to recognize that an abnormal condition exists and has a level of severity warranting intervention and that an intervention is available to treat the condition.33 In the present study, all patients were from remote tribal region of Madhya Pradesh. They had a low level of education and lacked awareness about the gravity of the problem. The language barrier also played a major role in the management of patients. A study from past found that communication has an influence on healthcare delivery and patient safety.34 The decision to immediately seek medical assistance affected the final arrival at the medical facility. It is recommended that when an emergency occurs on large scale as in cluster endophthalmitis, any delay makes a huge difference in the outcome. Besides managing the cases on an emergency basis, ample time should be devoted to preoperative counselling, there has to be proper planning with special attention to logistics and hygiene of patient and close postoperative follow up to identify the complication at the earliest.35
The National Program for Control of Blindness (NPCB) norms for service delivery in eye camps emphasizes that camps should be held under controlled conditions with due permissions and safety measures, always in a permanent operation theatre setup. It is also mandated that all the drugs and solutions for intraocular use should be procured in advance from GMP-certified manufacturers and the batch is evaluated for contamination by microbiological tests and fluids for intraocular use should be autoclaved before use in camp setting.36
There are few limitations of our study. First, the patients were from tribal region and language was a big barrier in communication between patient and doctor. Secondly, patients follow-up could not be done. Thirdly, a complete vitrectomy could not be done in all cases due to compromised visualisation of posterior segment.
To summarize, endophthalmitis remains a dreaded complication of cataract surgery and cluster endophthalmitis is a catastrophic ophthalmic situation both for the patient and the surgeon. It, nonetheless, can be prevented and managed successfully.