Introduction
Paediatric vitreoretinal surgery (PVRS) has its unique set of challenges compared to surgery in adult eye. An understanding of ocular growth and development is an important consideration in PVRS. Changes in ciliary body dimensions with age may affect how sclerotomies are placed, so as to avoid iatrogenic damage to the peripheral retina. These changes are especially dramatic in early childhood.1
PVRS has important differences compared to that in adults. The main indications for PVRS include rhegmatogenous retinal detachments (RRD) caused by trauma, congenital retinoschisis, marfan, stickler or morning glory syndrome, peripheral retinal degenerations, fundus coloboma, retinoblastoma, myopia, previous ocular surgery and tractional retinal detachments (TRD) caused by retinopathy of prematurity(ROP), persistent fetal vasculature (PFV), familial exudative vitreoretinopathy (FEVR) and penetrating ocular trauma. RRD in the adult usually associates with the posterior vitreous detachment (PVD), while as the RRD in paediatric age is often caused by trauma or congenital abnormalities. As paediatric retinal detachment (RD) usually present in late stages and paediatric ocular anatomy is featured, PVRS is more difficult and complex and has greater complication rates. The most common devastating complication of PVRS is proliferative vitreoretinopathy (PVR). In particular, creating an iatrogenic retinal break in (IRB) during PVRS can cause PVR in children because of the strong inflammatory and proliferative response.2, 3, 4, 5, 6
Some special evaluations such as preoperative planning, appropriate information to parents on the management, good examination and viewing of fundus under general anaesthesia, decision on application of scleral buckle (SB) or pars plana vitrectomy, the entries, angles and placement of sclerotomy and trocars, crystalline lens status, separation of the posterior hyaloid, selection of intravitreal tamponade and also visual rehabilitation are required for PVRS.7, 8, 9, 10, 11, 12, 13, 14
Materials and Methods
This was a prospective interventional study of 20 consecutive patients aged 18 years or younger undergoing vitreoretinal surgery for retinal detachment at the department of Ophthalmology of Jawahar Lal Nehru Medical College, Ajmer (Rajasthan) in a time period between October 2020 to March 2022.
Exclusion criteria
Presence of significant corneal opacity.
Presence of significant conjunctival and/or scleral scarring.
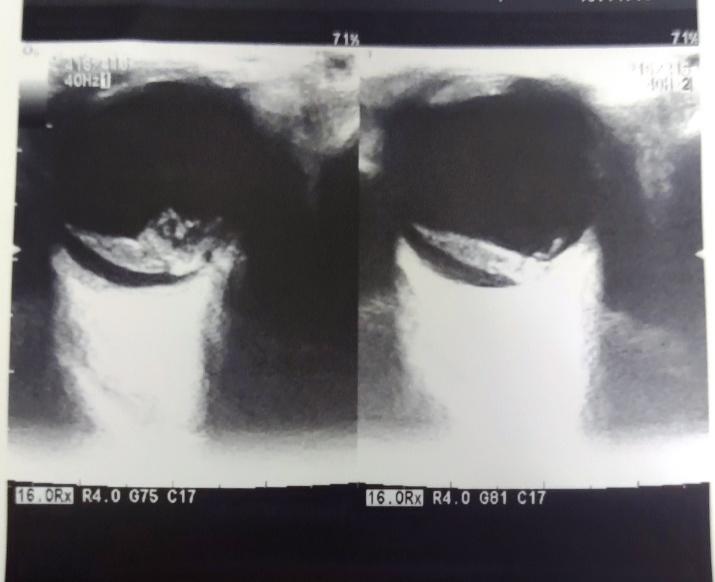
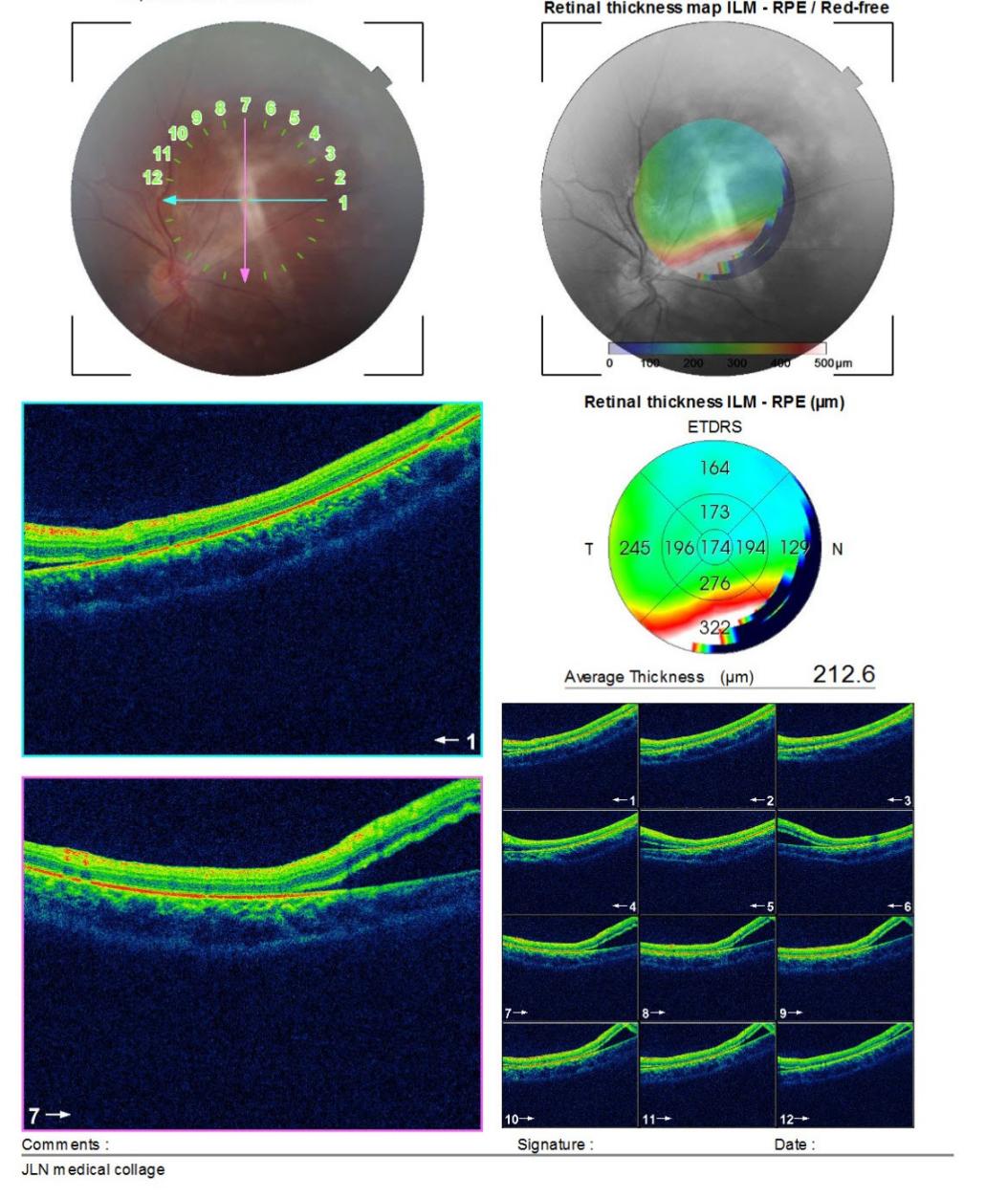
A detailed ocular and systemic history was recorded from all the patients. Written informed consent was taken from all patients. Preoperative and postoperative data were collected. Descriptive statistical analysis including name, age, gender, laterality, etiology, duration of presenting symptoms, presence of ocular comorbidities, anterior segment evaluation by slit lamp biomicroscope, macular status, presence or absence of proliferative vitreoretinopathy (PVR), ocular coherence tomography (OCT)- if required, initial and final best corrected visual acuity (Snellen visual acuity converted to logMAR), type of endotamponade used, pre and postoperative lens status, intraocular pressure (IOP) measurement (by schiotz tonometer), anatomical success and complications if any. A preliminary ultrasonography was done where there was no view of fundus. Other investigations were included according to need of diagnosis and requirement of anaesthesia.
Surgical procedure
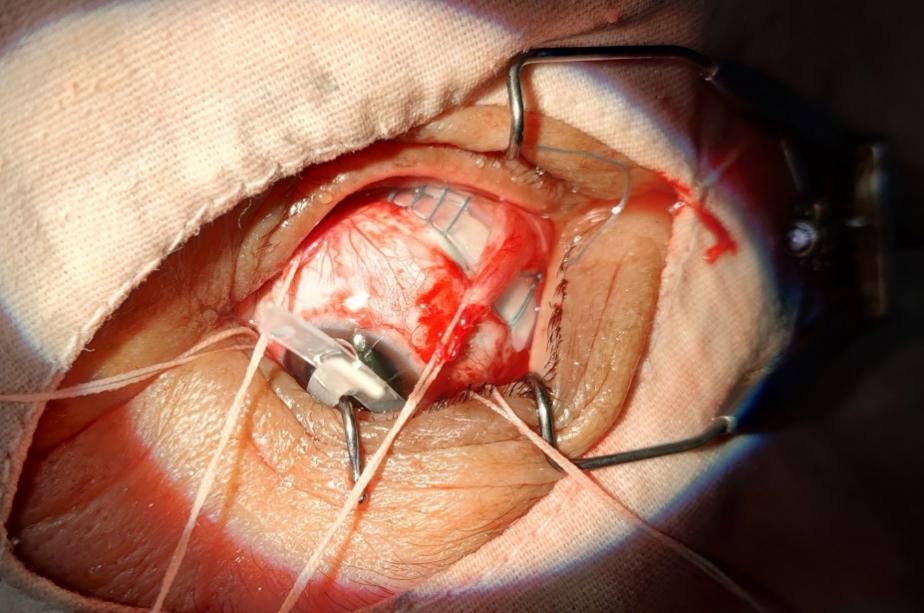
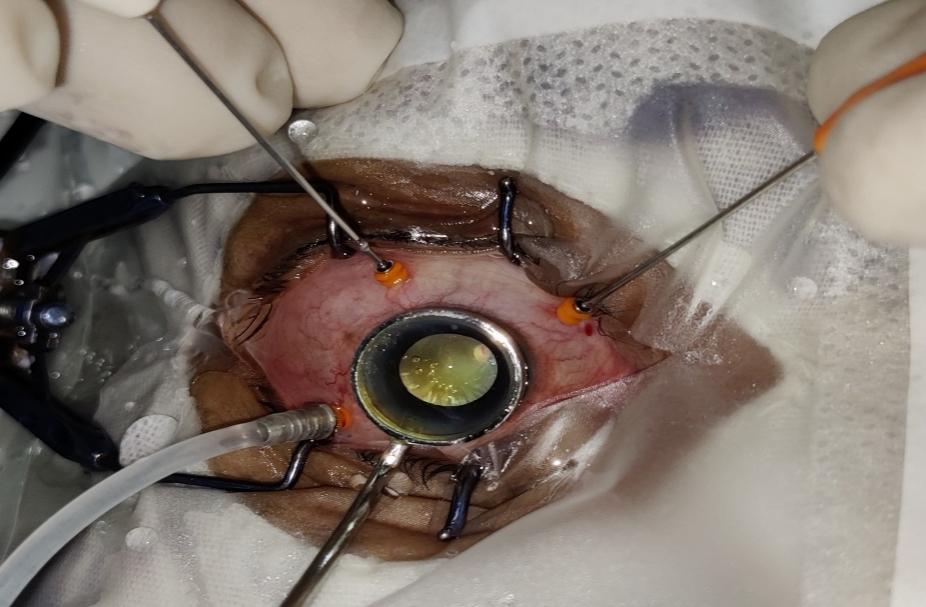
All the surgeries were performed under general anaesthesia. In patients with visible retinal breaks scleral buckle surgery was done. Three port 23G pars plana vitrectomy with silicone oil or air endotamponade was done in patients with un-detected retinal breaks, large and/or multiple retinal breaks, complicated RD with PVR and obscure ocular media. Pars plana lensectomy with vitrectomy also performed in patients with traumatic cataract. Combination of both scleral buckling and pars plana vitrectomy was also performed.
All evaluated eyes were followed up postoperatively day 1, one week, one month and three month. Outcome of surgery was measured in terms of improvement in visual acuity and retinal status.
Results
Demographical and clinical characteristics of patients are presented in Table 1.
Twenty eyes of 20 patients were studied. There were 15 (75%) males and 5 (25%) females. The mean age (SD) of the patients was 16.4 (2.01) years, ranging from 11 to 18 years. When coming to etiology,13 (65%) cases were due to trauma, 6 (30%) cases due to myopia and 1 (5%) case due to fundal coloboma. Figure 1 shows the morphology of RD found in each eye. PVR was seen in 20% cases, multiple retinal holes/breaks were found in 20% cases, tractional RDs were seen in 10% cases, exudative RD in 5% cases and giant retinal tears were seen in 5% cases. Break type was not specified or known in 40% cases. When coming to status of macula; macula was off in 8 (40%) patients, whereas macula on was seen in 12 (60%) patients.
Various surgical interventions were done, and they had been chosen based on the morphology of RD. out of total 20 patients 10 (50%) patients had been treated with pars plana vitrectomy (PPV), 3 (15%) patients underwent lensectomy with vitrectomy, 5 (25%) patients were treated with scleral buckle (SB) surgery with retinopexy, and 2 (10%) patients were treated with PPV with SB. Most commonly used endotamponade was silicone oil (93.33%) and in 1 case air was used. Preoperative mean BCVA was 2.33±1.12 and postoperatively at final follow up mean BCVA was 1.56±0.80 with statistically significant P value (0.001) as shown in Figure 2. Visual acuity improved in 17 patients (85%), deteriorate in 2 patients (10%) and stable in one patient (5%) at 3 months. Primary anatomical success was achieved in 16 patients (80%) at final follow up.
Intraoperative complications did not occur in our study. Table 2 shows complications after surgical intervention. Early postoperative complications (≤1 week) included corneal edema in 2 patients, hypotony in one patient, ocular hypertension in one patient, hyphema in one patient, pre-retinal bleeding in one patient and endophthalmitis in one patient. Late postoperative complications (>1 week) included Re-Retinal detachment (ReRD) in 3 patients and cataract in 2 patients. None of the patient developed secondary glaucoma. Corneal edema and pre-retinal bleed resolved spontaneously at one week follow up. Hyphema after surgery cleared on its own during the follow up period. Ocular hypertension was controlled by systemic and topical IOP lowering agents. Hypotony was resolved during follow up in 7 days. One patient of endophthalmitis and three patients of ReRD required second vitreoretinal surgery. Two patients who developed cataract at three months follow up required cataract extraction and IOL implantation.
Table 1
Demographic and clinical characteristics
Table 2
Early and late post-operative complications
Discussion
This study was performed to assess the clinical characteristics of paediatric RD, surgical outcome and complications after vitreoretinal surgery in children. Out of total 20 patients, there were male predominance with 75% than females (25%). Robert Rejdak et al. in his study also found higher number of male patients (75%) compared to females. This male predominance may be due to higher exposure to trauma to male gender.15
Various etiological factors were present in patients with underlying retinal conditions; trauma was the most common etiology (65%) followed by myopia (30%). According to Robert Rejdak et al. trauma was the most common etiological reason (57.1%) for RD followed by high myopia (37.3%).15 Soheilian et al. in his study has evaluated clinical features, functional/anatomical outcomes after surgery in paediatric rhegmatogenous RD and found that trauma and congenital anomalies were the etiologies in paediatric rhegmatogenous RD.16 Macula was off in 40% patients. As reported by Paul C Ajamian et al. in his study that in all standard cases of macula-off RD, should get treated as quickly as possible because chronic detachments can dramatically affect the visual outcome and prognosis.17
Vitroretinal surgeries used in the treatment of RD herein included pars plana vitrectomy, scleral buckle surgery and combination of both PPV-SB. Primary retinal reattachment rate achieved after surgery was 85% at last follow up, where as one patient of scleral buckle surgery developed endophthalmitis at one week follow up. Robert Rejdak et al. in his study achieved anatomical success in 86% cases.15 Gurler et al. also retinal reattachment after primary surgery in about 80% of cases. He reported better BCVA with RD associated with trauma than in cases of myopia.18
The surgical principles that guide repair of adult retinal detachment also direct the repair of paediatric retinal detachment, relief of vitreous traction on the causative retinal defects, reapproximation of the retina to the retinal pigment epithelium.19 Paediatric vitreous is often more rigid and adherent than adult vitreous. In cases with broad peripheral pathology, the vitreous itself can help to tampnade a break, once the traction has been relieved with a scleral buckle, allowing resorption of sub-retinal fluid.12 Vitreous that is retained near a break may contract, leading to recurrent detachment. Higher intraocular cellular activity means that the probability of developing PVR and recurrent detachment is higher in paediatric patients with retinal detachment when compared to adults with the same.19 Vitreoretinal surgeries are challenging in children due to strong vitreoretinal adhesions so that iatrogenic retinal break easily occur. It can be associated with cataract formation due to lens injury during surgery. Subsequent cataract surgery was required in 2 cases as described above.
In this study mean BCVA was improved in 85% cases, deteriorate in 10%, and stable in 5% cases. Good visual outcome after surgery was favourably influenced by preoperative visual acuity. The paediatric traumatic RD usually present early while no traumatic RD usually present at a later stage compared to adults. Therefor the management often lasts for a long because to fight the amblyopia and visual rehabilitation compared to adults.
Conclusion
In this study, mean age of the patients was 16.4±2.01 with male predominance. Most common etiology was found to be trauma followed by myopia. PPV was the major surgical procedure in this study due to complexity of RD. Most common endotamponade used was silicone oil in PPV. The visual and anatomical outcome following surgery were favourable in 85% and 80% cases respectively. Four eye underwent second vitreoretinal surgery (3 patients of ReRD and 1 patient of endophthalmitis) and two eyes for cataract surgery. Postoperative visual rehabilitation was also done to fight to amblyopia as far as possible.