Introduction
Infective keratitis with acanthamoeba spp. is a serious eye disease. The disease is rare in non-contact lens wearers1 and frequently remain undiagnosed in clinical practice leading to preventable loss of vision. To the best of our knowledge, the present case series is the first one in literature where diagnosis of acanthamoeba keratitis is based solely on detection of motile trophozoites in direct wet mount examination. The ulcers healed with instillation of an acanthamoebicidal2 0.02% Chlorhexidine gluconate eye drop, thus further confirming the laboratory diagnoses. Knowledge of risk factors and symptomatology is required for clinical suspicion and fair to good restoration of vision is possible if diagnosis as well as treatment is initiated appropriately.
Case History
Case 1
A 14-year-old boy presents in Eye emergency room referred from a peripheral rural hospital with the history of pain, redness, watering, photophobia and dimness of vision in his left eye for 15 days. He also noticed whitening of the cornea during this period. He had a history of taking bath in a reservoir at civil construction site. There was no history of contact lens wear. He was on eye drops natamycin 5%, moxifloxacin 0.3%. On examination LE-visual acuity –counting finger 30 cm with PR accurate in all quadrants, lid- severe blepharospasm, conjunctiva- severe congestion, cornea- well – circumscribed central stromal infiltrate of 5mm x 5 mm. There was also a ring infiltrate around the central infiltrate, the intervening cornea between the two infiltrates was spared. An epithelial ulcer of 1.5mm x 1.5 mm was present at the inferotemporal rim of the ring, giving rise to a typical signet ring appearance on fluorescein staining. Anterior chamber- flare++, Cells++, no hypopyon (Figure 1, upper left). Right eye was normal. A provisional diagnosis of Acanthamoeba/ fungal corneal ulcer of left eye was made, corneal scraping was done and with the scraped material wet mount preparation with normal saline was done and the rest was inoculated in different culture media and immediately sent to parasitology and microbiology laboratory. Microscopy of Wet mount preparation of corneal scraping showed presence of motile acanthamoeba spp. (Figure 1 upper right and lower left). Therefore the patient was put on eye drops chlorhexidine gluconate 0.02%, natamycin 5%, moxifloxacin 0.3% hourly in the daytime and 2 hourly at night, eye ointment neomycin thrice a day and, eye drops atropine sulphate 1%, Timolol maleate 0.5% twice a day. Culture report after 48 hours and one week in SDA and SDA CCA media showed no growth. Culture in Blood agar did not show any growth of microorganism. Therefore, eye drop moxifloxacin and natamycin were discontinued after one week and rest continued. The ulcer healed after 30 days of in-patient therapy (Figure 1, lower right). The final visual acuity was 6/60 at discharge.
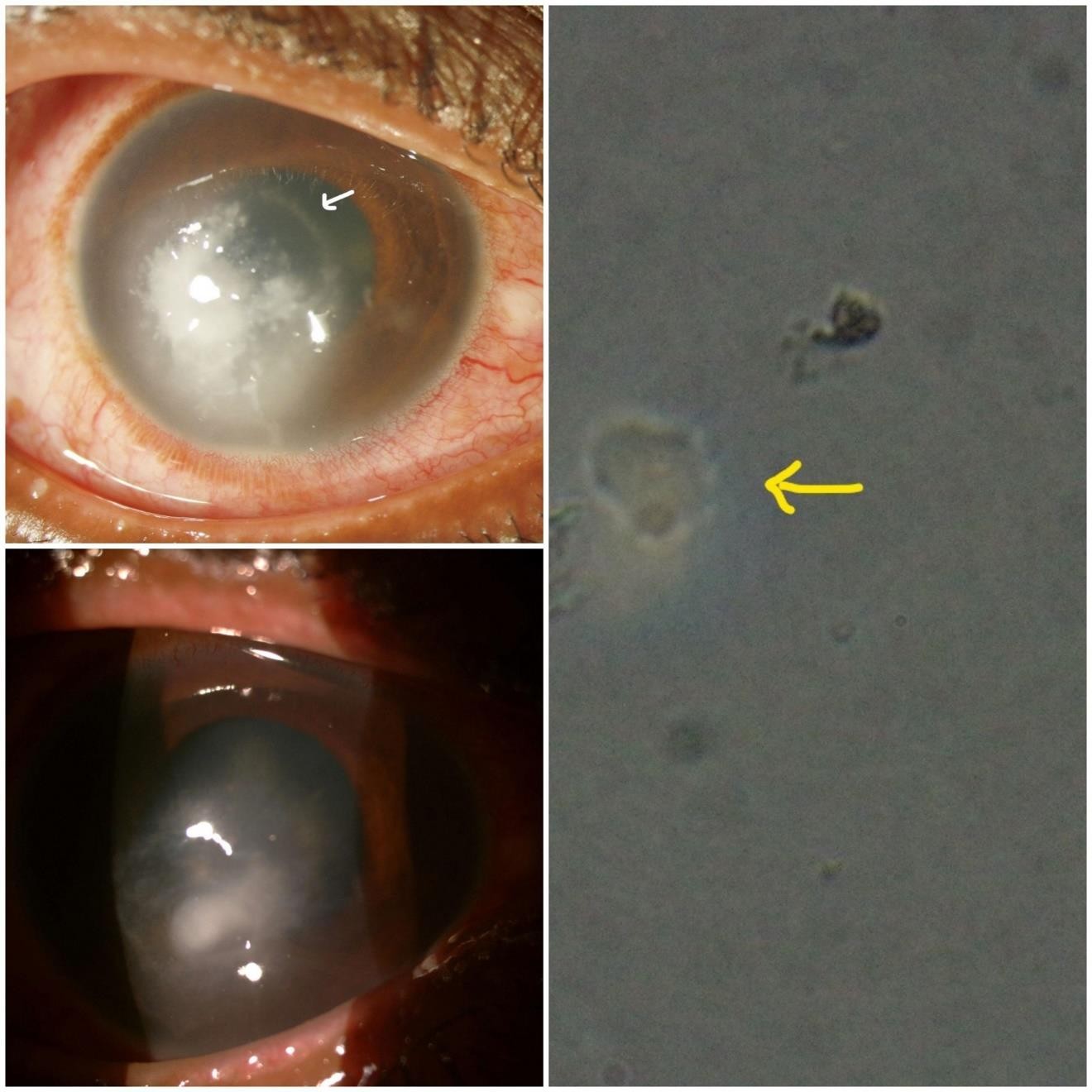
Figure 1
Case 1: Reader’s view; upper left. Healing Acanthamoeba ulcer: epithelial ulcer infero- temporally (big arrow), part of ring infiltrate still discernable (small arrow). upper right. Trophozoites of acanthamoeba under microscope (40 x 10) in direct wet mount showing irregular out line with finger like pseudopodia and prominent nucleus in each cell. (lower left) One trophozoite of acanthamoeba focused under high power magnification showing prominent nucleus and pseudopodia. (lower right) Healed acanthamoeba ulcer
Case 2
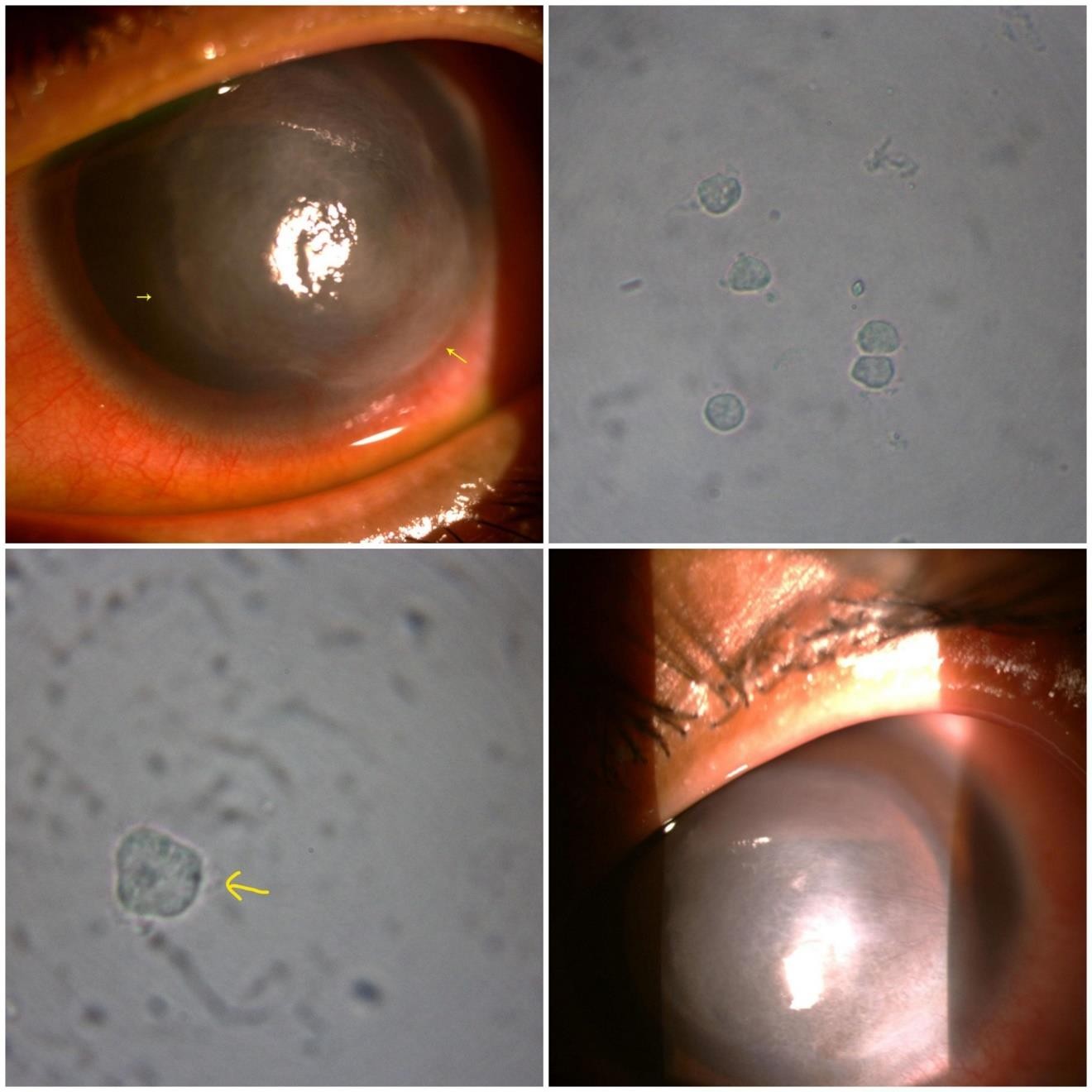
A male of 34 years of age attended OPD with complain of pain, redness, watering, photophobia and whitening of cornea with dimness of vision in his right eye for 28 days. At first, he was treated by a local eye specialist with eye drop ciprofloxacin 0.3%, eye drop Natamycin 5%, eye ointment aciclovir and eye drop cyclopentolate 1%. After 12 days of this therapy pain and other symptoms went on increasing. He then attended a private hospital where he was added eye drop voriconazole with his previous treatment regimen. However, another two weeks of treatment with this treatment regimen his symptoms did not subside, and he attended our OPD. On examination, visual acuity of right eye -perception of light with projection of rays accurate in all quadrants. Lids- swollen, blepharospasm+. Conjunctiva- congested. Cornea- fluorescein +ve epithelial ulcer of 5mm x 5 mm in the centre of the cornea with stromal infiltrate, with a rim of incomplete ring infiltrate was found (Figure 2 upper left). Anterior chamber- flare+++, cells+++, hypopyon 3 mm. Perineural infiltrate- present. Left eye was normal. A provisional diagnosis of acanthamoeba keratitis of right eye was made and patient was admitted. Wet mount microscopy of corneal scrapes showed trophozoites of acanthamoeba (Figure 2 right) Therefore the diagnosis was confirmed. Treatment started with Eye drop Chlorhexidine gluconate 0.02% hourly in the daytime and two hourly at night. In addition eye ointment Neomycin, e/d Atropine, e/d Timolol maleate, e/d Carboxymethylcellulose were continued. Patient felt subjectively better within few days and hypopyon disappeared after seven days. Ulcer completely healed after 89 days of hospital stay (Figure 2, lower left). However, during the course of the treatment there was some waxing and waning of signs and symptoms and e/d Fluconazole 0.3%, e/d voriconazole 1% which have proven anti-acanthamoeba activity were used for limited periods depending on clinical judgment. Final BCVA was 6/9.
Case 3
A 45 years age-old male presented in eye OPD with complain of pain, redness, swelling, dimness of vision of left eye for last one week following eye injury by stick. He also noticed whitening of cornea. Earlier he visited an eye-specialist and was on antibiotics (moxifloxacin, tobramycin), antifungal (natamycin) eye drops and antiviral (acyclovir) eye ointment, but with no relief. On examination at opd, visual acuity of left eye-perception of light with projection of rays accurate in all quadrants. Lids-swollen, blepharospasm+. Conjunctiva- congested. Cornea- fluorescein – ve, 4mm x 4 mm round stromal infiltrate located slightly off-centre towards inferior quadrant with a complete stromal ring infiltrate surrounding it. Anterior chamber- flare+++, cells+++, hypopyon 1.5 mm (Figure 3, upper left). Right eye was normal. Therefore, a provisional diagnosis of acanthamoeba keratitis was made and patient was admitted. Direct wet mount examination of corneal ulcer scraping showed presence of motile trophozoites of acanthamoeba. (Figure 3, upper right). Treatment started with eye drop chlorhexidine gluconate 0.02% hourly in the daytime and two hourly at night. In addition eye ointment neomycin TDS, e/d atropine 1% B.D, e/d timolol maleate 0.5% B.D, e/d carboxymethylcellulose TDS were continued. Patient was discharged from hospital after 21 days and same treatment continued thereafter for two more months. Ulcer healed but with severe fibrosis and thinning (Figure 3, lower). Final BCVA was PL+, PR accurate in all quadrants.
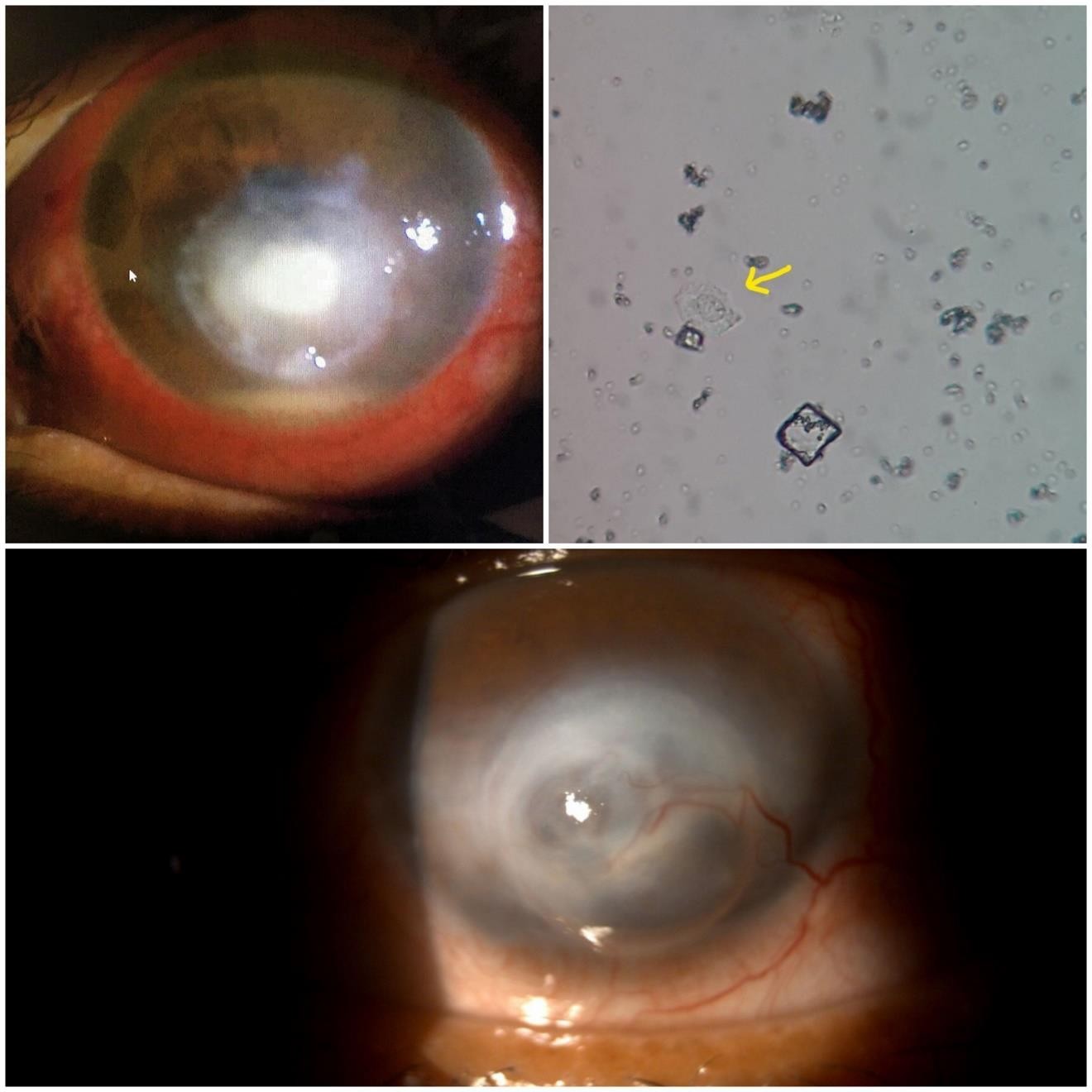
Figure 3
Case 3: (Reader’s view): upper left: round stromal infiltrate located slightly off-centre towards inferior quadrant with surrounding complete stromal ring infiltrate. upper right. trophozoite of Acanthamoeba, horny surface with prominent nucleus and pseudopodia. lower. Healed Ulcer. Fibrosis and thinning of cornea is seen
Discussion
Patients with acanthamoeba keratitis are diagnosed fairly late, more so in noncontact lens wearers. All of the cases of our series were noncontact lens wearer. In Sharma et al.1 series of 39 cases, 15 (38.46%) were diagnosed in more than 30 days and 24 (61.53%) within 30 days of initial symptoms. In our series of 03 cases, case 1, 2, 3 were diagnosed 19 days, 31days and 10 days respectively after the onset of initial symptoms. The patients of Acanthamoeba keratitis are commonly treated by many ophthalmic physicians before being diagnosed.1 In series of Sharma et al. 84.61% patients received ophthalmic attention before attending to tertiary care centre. In our series all 03 patients were treated by ophthalmic physicians before attending to our centre. Common misdiagnoses and treatments are for bacterial, fungal, or viral keratitis in both Sharma et al1 and in our series. Therefore, in general there is substantial delay in diagnosis and commencement of anti- acanthamoeba treatment.
In our series, delayed presentations, presence of excruciating pain and blepharospasm with varying combinations of signs like ring infiltrate (complete ring in cases 1 and 3 and incomplete ring in case 2), hypopyon (in cases 2 and 3) and failure of antifungal, antibacterial, antiviral medications aroused the suspicion of Acanthamoeba keratitis. Radial perineural infiltrate was found in case 2. All these clinical features and their frequencies were in conformity with those of Sharma et al.1
Treatment protocol and Visual recovery of our cases were in conformity with those reported by Lim 128 N et al.
We employed simple parasitological confirmatory tests by direct wet mount examination of corneal scraping material under microscope.
In the case series of Sharma et al.,1 none of the 39 cases who attended tertiary eye centre had prior microbiological examination although (33/39) 84.61% had received ophthalmic attention before reporting the centre. This showed that there was a huge lacunae in the awareness and facility of microbiological examination below the level of tertiary eye care centre. However, Calcofur white stain, non-nutrient agar with E coli overlay culture, PCR test are not supposed to be available outside dedicated eye hospital laboratories.
We employed the following protocol for preparation and transportation of wet-mount of corneal scraped material: A Petri-dish was kept ready with two sterile broom-sticks of 7.5 cm length each lying parallel to each other at some distance, to accommodate two clean glass slides over these sticks. Ulcer was thoroughly scraped with No.11 B.P scalpel blade and smear was prepared on the slides on one to two drops of normal saline (from a fresh bottle) and a cover slide of 22×22 mm was placed onto the smear. Cotton balls moistened with normal saline were kept inside the petri-dish on four corners to keep the chamber moistened. The petri-dish containing the slides were then rapidly transported to the Parasitology department stationed at the next building and examined under microscope within 15 minutes. Parasitologist was informed beforehand to prevent delay in examination.
Very few studies are available in English literature where detection of motile trophozoites in direct wet mount preparation was tried for diagnosis of acanthamoeba. In two studies to our knowledge this was tried, but authors failed to locate trophozoites in any of the cases although all those cases became acanthamoeba positive by some other tests.3, 4
Therefore, our study report is unique as we were able to detect acanthamoeba trophozoites persistently in direct wet mount examination. In our case series we have shown that this is a simple method to detect motile trophozoites. We think if wet mount microscopy becomes a routine practice, the rate of diagnosis of acanthamoeba keratitis in early stage would be enhanced. Therefore, we recommend direct wet mount microscopy of the corneal scraped material to be included in the routine protocol for the diagnosis of acanthamoeba keratitis.