Introduction
Retinopathy of prematurity (ROP) or retrolental fibroplasia as it was formerly named is a retinal disorder occurring mainly in premature infants. Its key pathological change is retinal neovascularisation. Like other proliferative retinopathies like Diabetic and Sickle cell retinopathy, ROP is associated with local ischaemia and subsequent development of neovascularisation.1, 2
ROP is unique in that the vascular disease is found only in infants with immature, incompletely vascularised retina; hence its connection with low birth weight premature infants’ has been responsible for major cause of blindness in neonates.
It can be mild with no visual defects, or it may become aggressive with neovascularisation and progress to retinal detachment and blindness. Timely screening and treatment of ROP can prevent blindness and minimalize visual handicaps.
Retinopathy of prematurity, was first identified by Terry in 1942 who named it retrolental fibroplasia based on his impression that the primary change involved a proliferation of embryonic hyaloid system which incorporated the retina. The term retinopathy of prematurity was coined by Heath in 1951.
Firstly, duration of oxygen administration was found to be of major significance in development of ROP in 1950s. Over next decades a number of factors were found possibly associated with incidence of ROP
Risk factors in ROP3, 4, 5, 6
Birth weight and gestational age
The major risk factor for development of retinopathy of prematurity. The younger the GA and the lesser the birth weight, the greater are the chances of developing ROP.
Oxygen use
Excessive use of oxygen in premature baby with respiratory distress syndrome is an important contributory.
Though, no direct association has been found between oxygen and ROP as ROP can be found in premature neonates who never received oxygen.
Respiratory distress syndrome
RDS is caused by a surfactant deficiency in the neonate. With RDS, the infant may become hypoxic and require mechanical ventilation and oxygen therapy, both of which are associated with increased incidence of ROP.
Light
Early exposure to light was suggested as a causative factor. It was proposed that light could, by damaging retinal tissue, generate free radicals and thereby cause ROP.
Exchange transfusion
Preterm infants given blood transfusions receive adult haemoglobin as the latter binds oxygen less avidly than foetal haemoglobin, the oxygen dissociation curve is shifted so that more oxygen is delivered up rendering tissues relatively hyperoxic. This could increase the risk of ROP.
Other risk factors7, 8
Maternal Factors: maternal factors including maternal hypertension, gestational diabetes, maternal age has been considered associated risk factors in development of ROP.
Neonatal anaemia, thrombocytopenia has been implicated in development of ROP in many studies. Mechanism though not fully known might be due to production of reactive oxygen species due to need for blood transfusion. Thrombocytopenia has been found associated particularly with occurrence of APROP.
Patent ductus arteriosus, neonatal sepsis, intraventricular haemorrhage may lead to retinal hypoxia leading to ROP development
Various studies from India have reported incidence of ROP varying from 20% to 52%.5, 9 With the development of neonatology, more of the high risk premature infants, those with extremely low birth weight, are now surviving, who have the highest risk of ROP.1, 2, 4
In 1970s, cryotherapy was used as treatment to destroy spindle cells, presumed source of angiogenic factors. With the advent of portable diode laser systems most of the countries have switched over to laser photocoagulation because of its precision and fewer side effects. Management of retinal detachment due to ROP is surgical with poor visual prognosis.
ROP screening10, 11, 12, 13, 14
According to guidelines by RBSK screening should be carried out for the infants with either of the following:
Birth weight Less than 2000 gm
Gestational age less than 34 weeks
Gestational age between 34 to 36 weeks but with risk factors such as : i) prolonged oxygen therapy ii) Respiratory Distress syndrome iii) Chronic lung disease iv)neonatal sepsis v) blood transfusion vi) intraventricular haemorrhage vii) exchange transfusion.
Infants with unstable clinical course who are at high risk (as determined by neonatologist or paediatrician.
Infants should receive screening at 4 weeks of birth.
Infants with gestational age less than 28 weeks or birth weight less than 1200 gm should receive first screening at 2-3 weeks after delivery.
Classification of ROP10, 11, 12
International Classification of ROP (ICROP)
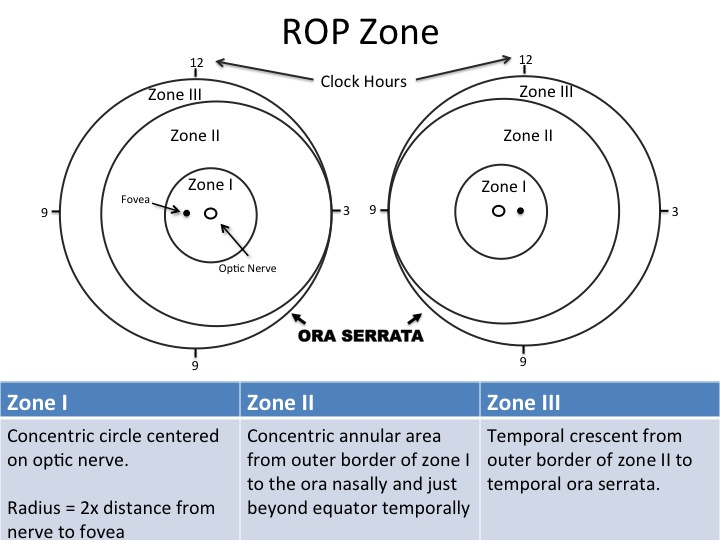
According to location
Zone I (Posterior pole or inner zone) : the limits of zone I are defined as twice the disc fovea distance in all direction from the optic disc.
Zone II: extends from the edge of zone I peripherally to a point tangential to the ora serrata nasally and just beyond equator temporally.
Zone III: Is a residual temporal crescent of retina anterior to Zone II. This zone is last to get vascularized in premature eye.
Extent: The extend of the disease is coded by the number of clock hours with ROP. The extent is further described as contiguous clock hours of ROP or non-contiguous clock hours.
Staging (as defined by ICROP)10
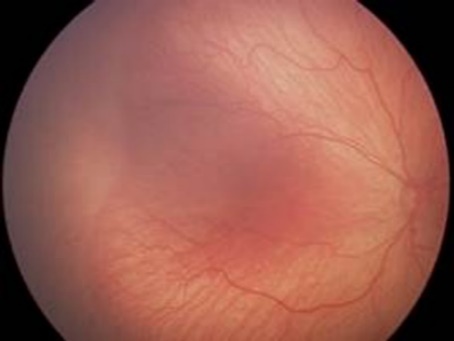
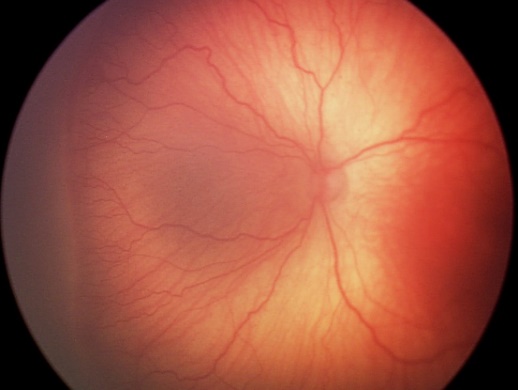
Stage 1 (Demarcation Line): There is a thin but definite structure that separates the avascular retina anteriorly from the vascularised retina posteriorly. It is relatively flat, lies within plane of retina and is white in colour.
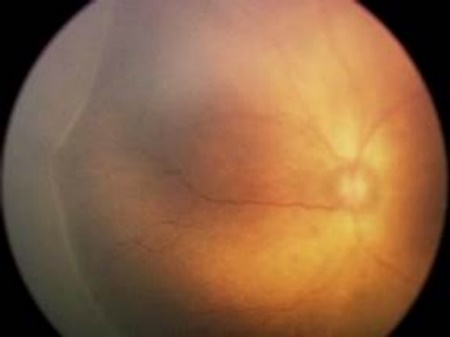
Stage 2 (Ridge): The line of stage 1 grows, has height and width, extends up out of the plane of retina, may change colour from white to pink.
Stage 3 (Ridge with extraretinal fibrovascular proliferation): To the ridge of stage 2, the presence of extraretinal fibrovascular proliferative tissue is added.
Stage 4 (Retinal Detachment): It may be caused by an exudative effusion of fluid, traction or both.
Stage 4a: Subtotal retinal detachment not involving macula
Stage 4b: Subtotal retinal detachment involving macula
Stage 5: Total tractional retinal detachment. It is always in funnel shape
In addition to identifying the zone, stage and extent of the ROP, there may be other signs to indicate that the ROP is active.
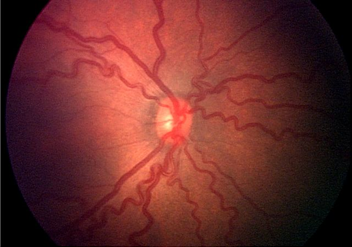
PLUS disease: It can be present as a major complicating factor at any stage. It is characterised by :
Significant level of venous dilatation
Arteriolar tortuosity of posterior retinal vessels.
Two quadrants of the retina must be involved for the changes to be characterised as plus disease
Associated changes may include : Iris vascular engorgement, poor pupillary dilatation, vitreous haze and anterior chamber haze.
PRE-PLUS disease: Pre-plus disease indicates posterior pole tortuosity and dilatation that are not sufficiently abnormal to reach the criteria of plus disease, but is nevertheless greater than that regarded as normal. It may or may not progress to plus disease.
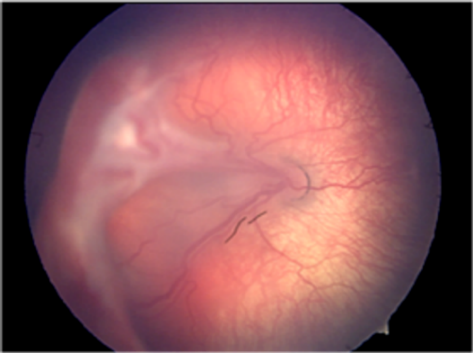
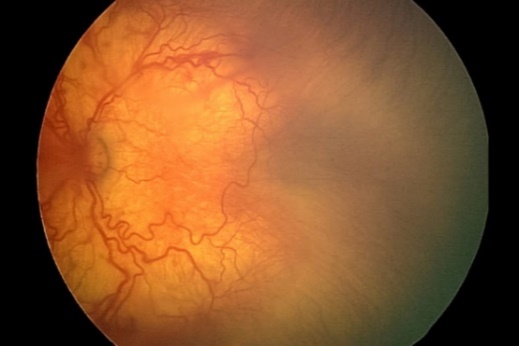
APROP (Aggressive Posterior ROP)
An uncommon, rapidly progressing, severe form of ROP is designated as AP-ROP, if untreated, it usually progresses to stage 5 ROP.
The characteristic features of this type of ROP are its posterior location, prominence of plus disease, and the ill-defined nature of retinopathy.
It was previously referred to as Rush disease.
It is observed most commonly in zone 1.
Materials and Methods
This is the cross-sectional study carried out in 500 newborns presenting in OPD at a tertiary care centre of Rajkot district in year 2021-2022 after approval from institutional ethical committee. Informed valid consent was taken from parents or guardian of the neonate. Patients were chosen according to inclusion and exclusion criteria.
Exclusion criteria
Any Neonates with more than 36 weeks of gestational age.
Any Neonates with more than 2500 gm of birth weight.
Any neonate with congenital conditions like – congenital heart diseases, genetic conditions and other ocular diseases like – congenital glaucoma, microcornea, mucopolysaccharidosis.
Examination was performed with approval of neonatologist/Paediatrician. The Informed Verbal Consent was taken from Patient’s parents or Guardian. History was taken along with risk factors according to proforma. The anterior segment was examined and pupillary reaction were noted. Then Pupil were adequately dilated with Tropicamide 0.5% with phenylephrine 5% instilled thrice every 10 minutes. Proparacaine was instilled in both eyes before examination for anaesthesia. Patient was immobilized by wrapping them in sterile linen. A sterile infant eye speculum (Alfonso) was used during examination. A complete fundus examination was done with Indirect ophthalmoscopy and 20 Dioptre lens. Scleral Indenter was used to see peripheral retina up to ora serrata. Patient was advised for follow up or was referred to higher centre as required.
Data was recorded and analysis of the data was done using student t test and chi square test to find p value of the data to find the significance of the study results.
Results
Total 500 preterm low birth weight neonates (1000 eyes) were examined during the study and the results found in the study were as Table 2.
In the study, among 500 patients, 271 patients were male and 229 patients were female patients.
Table 2
Distribution of patients with ROP according to gestational age
|
Gestational age (in weeks) |
Cases of ROP |
|
27 |
1 |
|
28 |
15 |
|
29 |
2 |
|
30 |
8 |
|
31 |
2 |
|
32 |
10 |
|
33 |
2 |
Table 3 shows that, among 40 patients who were diagnosed with ROP, majority of the patients (15 patients) were having gestational age of 28weeks, while least patients (1 patient) had gestational age 27 weeks.
Table 3
Distribution of patients with ROP according to post conceptional age
|
Post conceptional age (in weeks) |
Cases of ROP |
|
30-35 |
17 |
|
35-40 |
15 |
|
40-45 |
08 |
Table 4 shows, out of 40 patients diagnosed with ROP, majority of the patients(17patients) had post conceptional age 30-35 weeks, while the least patients (8 patients) had post conceptional age 40-45 weeks.
Table 4
Distribution of patients with ROP according to sex
|
Sex of patient |
Cases of ROP |
|
Male |
22 |
|
Female |
18 |
Among 40 patients diagnosed with ROP, 22 patients were male and 18 patients were female.
Table 5
Distribution of patients with ROP according to birth weight
|
Birth Weight ( in kg) |
Cases of ROP |
|
|
8 |
|
1.1-1.49 |
5 |
|
1.5-1.9 |
11 |
|
2.0-.2.4 |
14 |
|
2.5 |
2 |
Table 6 shows, among 40 patients with ROP. Maximum No. of the patients (14patients) had birth weight between 2-2.4 kg, while least number of patients were having birth weight 2.5kg.
Table 6
Distribution of patients with ROP according to Twins status
|
Twins status |
Cases of ROP |
|
Singlet |
33 |
|
Doublet |
7 |
Table 7 shows, among 40 patients with ROP,33 patients were singlets and 7 patients were twins.
Table 7
Association of ROP with prenatal steroids administration
|
Pre natal steroid administration |
Cases of ROP |
|
Given |
03 |
|
Not Given |
37 |
Table 8 shows, among 40 patients diagnosed with ROP, 37 patients did not receive pre natal steroids while, only 3 patients received pre natal steroids.
Results were analysed by students T- test and p value came out to be p=0.02 which implies that Prenatal steroid is a significant protective factor against development of ROP.
Table 8
Association of ROP with maternal systemic diseases
|
Systemic Diseases |
Cases of ROP |
|
Present |
03 |
|
Absent |
37 |
Table 9 shows, among 40 patients diagnosed with ROP, in 37 patients mother had no history of systemic disease like hypertension and diabetes mellitus, while 3 patients had history of any systemic disease in mother.
Table 9
Association of ROP with oxygen therapy
|
Oxygen therapy given (in days) |
Cases of ROP |
|
0-10 |
18 |
|
11-20 |
07 |
|
21-30 |
09 |
|
31-40 |
01 |
|
>40 |
05 |
Among 40 patients, 18 patients who developed ROP were given oxygen therapy upto 10 days. Whereas 5 ROP positive patients were given oxygen for >40 days.
Table 11 shows, among 40 patients with ROP 18 patients developed ROP, while 22 patients who developed ROP had no history of phototherapy.
Results were analyzed by student -T test and p value came out to be p=0.06 which implies association between occurrence of ROP and phototherapy is not significant.
Table 11
Distribution of ROP according to stages
|
Stage of ROP |
Number of cases |
|
Stage 2 |
15 |
|
Stage 3 |
05 |
|
Stage 4 |
10 |
|
APROP |
10 |
Table 13 shows that out of total 40 ROP cases 36 had history of respiratory distress syndrome (90%)
Results were analyzed by chi square test and p value came out to be p=0.004 which implies association between occurrence of ROP and RDS is highly significant.
Discussion
Table 13
Comparison between incidence of retinopathy of prematurity in various studies
|
Study |
Incidence |
|
Ved P. Gupta et al5 |
21.7% |
|
Anand Vinekar et al15 |
45.1% |
|
Sudha Chaudhari16 |
22.3% |
|
G Sanghi et al17 |
21.8% |
|
Present Study |
8% |
Incidence of retinopathy of prematurity in our study was 8%, which is less in comparison to other studies done in other parts of India. This might be due to difference in exclusion and inclusion criteria and methodology with other studies. There is need to emphasize more on timely screening for retinopathy of prematurity and need to strengthen the screening programme for retinopathy of maturity by organizing camps at grass root level so that more and more population can be educated about retinopathy of prematurity and greater number of children with risk factors for retinopathy of prematurity can be diagnosed and treated timely.
Table 14
Comparison of role of oxygen therapy in neonates with retinopathy of prematurity
|
Studies |
Conclusion |
|
Sudha Chaudhari et al16 |
64.5% |
|
Andrea Gin et al2 |
78.1% |
|
C Gilbert et al18 |
82.7% |
|
Present Study |
100% |
In our study, all the patients who developed retinopathy of prematurity were given oxygen therapy. It is close to other Asian and Indian studies as shown in Table 15 studies, however variation in the incidence may be due to variability in neonatal care and oxygen therapy practices in various NICU. From all the studies we can draw the conclusion that oxygen therapy has important role in pathogenesis of retinopathy of prematurity.
Table 15
Comparison of incidence of retinopathy of prematurity in very low birth weight baby (≤1.500 kg)
|
Studies |
Incidence |
|
Sudha Chaudhari et al16 |
23.6% |
|
G Sanghi et al17 |
41.18% |
|
Anand Vinekar et al15 |
23.3% |
|
Gupta et al5 |
21.7% |
|
Present Study |
29.78% |
In our study, incidence of retinopathy of prematurity in very low birth weight baby (≤1.5kg) was 29.8% which is almost similar to other Indian studies as shown in Table 16.
Table 16
Comparison of prevalence of APROP among babies diagnosed with ROP
|
Studies |
Incidence |
|
G Sanghi et al17 |
20% |
|
Anamika Diwedi et al19 |
27.7% |
|
Tekchandani et al20 |
22% |
|
Present Study |
25% |
In our study. Prevalence of APROP among babies diagnosed with ROP was 25%. It is almost similar to studies done in other parts of India.
Table 17
Comparison of average gestational age in patients diagnosed with ROP
|
Study |
Mean ± SD (Range) |
|
Parag et al1 |
31.7 ± 3,45 (Range, 28-35) |
|
Jalali et al21 |
29.6 ± 3.76 (Range, 26-36) |
|
Present study |
30.56 ± 2.18 (Range, 27-33) |
It can be seen from our study that average gestational age in patients diagnosed with ROP was approx. 30.56 weeks and it is similar to other studies done in other region of India. It was seen from our study that as there was increase in gestational age, number of patients with retinopathy were almost same which was consistent with other studies done by Parag et al. and Jalali et al. We can conclude that lower the gestational age, higher is the risk of developing ROP because immature vessels are more prone to oxidative stress due to oxygen therapy.
In our study, there were 7 doublet twins and all the twins developed Retinopathy of prematurity (p=0.4) which was not significant. Among them 3 twins had history of prenatal steroid administration (p =0.02) which was a significant protective factor against ROP and 2 patients had history of sepsis (p=0.07) and in 3 patients there was history of maternal hypertension (p=0.06). There was no significant association of sepsis and maternal systemic illness with occurrence of retinopathy of prematurity. Reason for occurrence of ROP in all twins was associated with low birth weight and long term exposure to the oxygen therapy.
In similar study conducted by Rao et al17 16.36% of twins developed ROP, but twining was not significantly associated with occurrence of retinopathy of prematurity.
Comparison of risk factors for APROP in various studies.
Table 18
Gestational age
|
Study |
Gestational age (in weeks) Mean ± SD (Range) |
|
G Sanghi et al17 |
30.7 ± 1.03 ( 29-32) |
|
Parag et al22 |
31.7 ± 1.34 ( 28-35) |
|
Our study |
30.4 ± 1.87 ( 28-33) |
Table 19 shows, average gestational age for occurrence of APROP was approximately 30 weeks and it is almost similar to other Indian studies.
Table 19
Oxygen exposure duration
|
Study |
Duration of oxygen exposure (in days) (Range) |
|
G Sanghi et al17 |
7-23 |
|
Parag et al22 |
3-25 |
|
Our study |
3-21 |
Table 20 shows that range of duration of oxygen exposure in patients with APROP was 3-21 days. It was almost similar to other studies done.
Table 20
Birth weight
|
Study |
Birth weight (in kg) (MEAN) |
|
G Sanghi et al17 |
1.79 kg |
|
Parag et al22 |
1.5kg |
|
Our study |
1.77kg |
Table 21 table shows mean birth weight in patients with APROP was 1.77kg and it was almost similar to other studies done India.
From our study and on comparison with other studies we can say low birth weight and extremely low birth weight, gestational age ≤ 30 weeks and chronic oxygen exposure were important risk factors in pathogenesis of APROP. Few patients with APROP in our study had septicemia which may be an important risk factor for pathogenesis of APROP.
Conclusion
The incidence of ROP in any stage was 8% in our study which is less than other studies conducted in India. This shows less awareness among parents for retinopathy of prematurity and its risk factors.
Mean Gestational age among ROP positive neonates was 31.76 weeks (range 27 to 33 weeks) which is comparable to other studies conducted in India. Inclusion criteria for gestational age in our study was ≤36 weeks. No positive ROP cases were reported in gestational age more than 33 weeks even with oxygen exposure and low birth weight.
Incidence of ROP in gestational age ≤32 weeks in our study was 11.5%. Only one positive case was noted in gestational age more than 32 weeks. This shows setting a smaller target population with lower birth weight and gestational age might yield better results with limited resources.
All the ROP positive patient had exposure to oxygen therapy for significant number of days. However, out of 381 neonates exposed to oxygen therapy only 40 developed ROP. Most of the patients who developed ROP were exposed to oxygen at very early post conceptional age. This shows that rather than oxygen therapy alone age at which oxygen is given is more important. Setting lower oxygen concentration targets in lower post conceptional age and higher targets for higher post conceptional age neonates might help in preventing ROP in neonates requiring oxygen support.
Most of the cases of ROP were in neonates with ≤2kg birth weight (33/40) in our study. Incidence of ROP in ≤2 kg birth weight neonates was18.9% in our study. Thus, our study shows that the lower the birth weight higher the chances of developing ROP.
Incidence of APROP in our study was 25% among ROP of any stages. Mean gestational age and birth weight for APROP in our study was 30.4 and 1.77 respectively.
Other significantly associated risk factors in our study was respiratory distress syndrome. 90% of the ROP positive cases had history of respiratory distress syndrome. Newborns with low gestational age were more prone to developing RDS leading to requirement of Oxygen or Ventilatory support.
Other risk factors considered in our study were phototherapy, intraventricular hemorrhage, blood transfusion, maternal factors, multiple pregnancies were found to be insignificant in our study.
Recommendation
Low birth weight and prematurity were the most important risk factors for developing any ROP. Late presentation for screening is the most important factor associated with ROP related blindness. Creating awareness in the Indian Society for early screening for the at risk neonates is necessary to prevent ROP associated blindness in infants. Also, a dedicated team of qualified staff including ophthalmologist and pediatrician should be appointed at every CHCs and district level so that screening for ROP can be done at greater scale covering rural population.