Introduction
Axonal degeneration is a phenomenon of central and peripheral nervous system wherein a nerve fibre will lose function after an injury. Degeneration of an axon in the direction of its terminal following direct injury is classified as anterograde degeneration, whereas retrograde degeneration proceeds towards the cell body.1, 2
Some investigators believe that retrograde degeneration do not occur in post geniculate lesions, since the second order neurons end at Lateral geniculate nucleus. This may be because of absence of optic nerve head changes in these lesions.3 This belief has been challenged over recent years,4, 5 by demonstrating RNFL and GCC thinning using OCT.6, 7
Materials and Methods
Patients referred to Ophthalmology OPD as diagnosed cases of unilateral retrogeniculate lesions (it included vascular occlusions and mass lesions) from other departments were included in the study. Those who showed homonymous hemianopia corresponding to the retrogeniculate lesions were subjected to complete Ophthalmological examination, OCT RNFL and GCC. OCT was done using Cirrus™ HD-OCT.
Patients with high refractive errors, diabetic retinopathy, glaucoma, age related macular degeneration, multiple sclerosis and sick patients who cannot perform HFA and OCT were excluded from the study. None of the patients had clinically evident optic atrophy at the time of examination.
Quadrant wise RNFL thickness and average RNFL thickness of both eyes were recorded. Sector wise GCC thickness and average GCC thickness of both eyes were also recorded. Average nasal GCC thickness was calculated by taking average of superonasal and inferonasal sectors. Likewise average temporal GCC was calculated taking average of superotemporal and inferotemporal sectors.
A written informed consent for conduct and publication of the study was taken from all the patients included in the study as per the ethical committee guidelines. The study got approved by the Instituitional Review Board (IRB-AIMS-2017-133) on 19-12-2017.
Statistical analysis was done using IBM-SPSS version 20.0 (SPSS Inc, Chicago USA). For all continuous variables, the results are given as Mean +/- SD and for categorical variables as percentage. To test the statistical significance of difference in Retinal Nerve Fiber Layer thickness and Ganglion Cell Complex thickness between ipsilateral and contralateral eyes of patients with retrogeniculate lesions, Independence sample t tests was used. To test the statistical significance of the association of thickness of RNFL and GCL with respect to the presence of retrogeniculate lesions, chi square test was done. A p value < 0.05 was considered as statistically significant.
Results
Out of 30, 21(70%) patients were males, 9 patients (30%) were females. Mean age of the study population was 55.5±14.02 years. 23 (76.67%) patients had vascular lesions, 7 patients (23.33%) had mass lesions. 11 patients (36.67%) had Right sided lesion with Left homonymous hemianopia and 19 patients (63.33%) had left sided lesion with Right homonymous hemianopia.
RNFL thickness analysis
Quadrant wise RNFL thickness analysis between ipsilateral and contralateral eyes showed that contralateral eyes have nasal and temporal quadrant thinning. There was statistically significant thinning of nasal quadrant in contralateral eyes.(p value-0.035). Inferior and superior RNFL quadrants did not show much difference.(Table 1). There was no statistically significant difference in average RNFL thickness between ipsilateral and contralateral eyes. (p value 0.290).(Table 1)
GCC thickness analysis
Table 2 shows that in ipsilateral eyes, temporal GCC was thinner compared to nasal. This was found to have borderline statistical significance. (p value-0.059). Incontralateral eyes, nasal GCC was thinner compared to temporal. This was not statistically significant. (p value-0.102).
Table 3 shows that nasal GCC was thinner in contralateral eyes and temporal GCC was thinner in ipsilateral eyes. These were not statistically significant.
Sector wise GCC thickness comparison showed that GCC was lower in nasal sectors of contralateral eyes compared to ipsilateral eyes (statistically significant in inferonasal sector (p value- 0.00) and superonasal sector(p value-0.019). Also GCC was thinner in temporal sectors of ipsilateral eyes compared to contralateral eyes r (p value-0.031). (Table 4)
Average GCC thickness did not show any statistically significant difference between Ipsilateral eyes and contralateral eyes.(Table 4)
Eight patients showed GCC thinning pattern respecting the vertcal meridian in GCC thickness map and deviation map, corresponding to the visual field defects. All these patients had a duration of more than 3 years between diagnosis and OCT.(Figure 1)
Figure 1
Ganglion cell thinning respecting vertical meridian corresponding to visual field defect in a post geniculate lesion
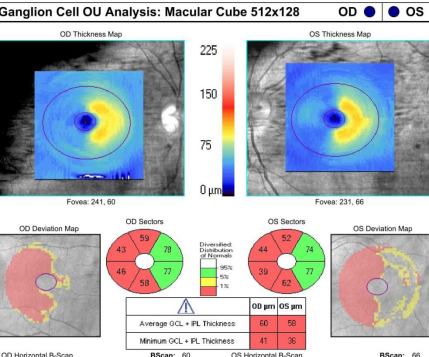
Table 1
Comparison of RNFL thickness in different quadrants between Ipsilateral and contralateral eyes
Table 2
Comparison of average nasal GCC with average temporal GCC of ipsilateral and contralateral eyes
|
|
Nasal GCC mean ± SD |
Temporal GCC mean ± SD |
p value |
|
Ipsilateral eyes |
71.62 ±9.789 |
66.83±9.443 |
0.059 |
|
Contralateral eyes |
66.95±10.692 |
69.70±10.009 |
0.308 |
Table 3
Comparison of nasal and temporal GCC of ipsilateral with contralateral eyes
|
|
Ipsilateral Eyes Mean ± SD |
Contralateral Eyes Mean ± SD |
p value |
|
Nasal GCC |
71.617 ±9.789 |
66.95±10.692 |
0.065 |
|
Temporal GCC |
66.833 ±9.443 |
69.70±10.009 |
0.214 |
Table 4
Comparison of mean thickness of GCC sectors between ipsilateral and contralateral eyes
Discussion
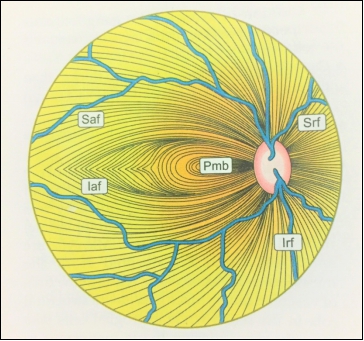
Arrangement of Retinal Nerve Fiber Layer (RNFL) of temporal and nasal retina at optic nerve head.8, 9
Nasal Retinal Nerve Fibres reach optic disc as superior and inferior radiating fibres (Srf & Irf), which enters optic nerve head nasally, superonasally, superiorly, inferonasally, and inferiorly.
Papillomacular bundle (PMB): pass straight to temporal part of disc.
Temporal Retinal Nerve Fibres arch above and below the papillomacular bundle as superior / inferior arcuate fibres. (Saf & Iaf) which enters the optic disc superotemporally, superiorly, inferotemporally, and inferiorly.(Figure 2).
In this study we compared RNFL and GCC thickness between affected and unaffected fibres because of the characteristic projection of fibres to visual cortex.
Retinal nerve fiber layer thickness parameters
We found that superior and inferior RNFL thickness was not much different between ipsilateral and contralateral eyes. The circumpapillary RNFL in the superior and inferior parts of the optic nerve comprises retinal nerve fibers originating from both temporal and nasal hemiretinal areas. Hence superior and inferior RNFL cannot help in topographical localisation of visual pathway lesions.
In our study, nasal and temporal RNFL quadrants thinning was present in contralateral eyes. Nasal RNFL quadrant receives fibres only from nasal hemiretina as nasal radiating fibres.8, 9 Temporal RNFL quadrants consists of fibres from both nasal hemiretina as papillomacular bundle and temporal hemiretinae as arcuate fibres. The major contribution is from papillomacular bundle. Hence we can expect nasal and temporal RNFL thinning in contralateral eyes which contribute to decussating nasal fibres of retrochiasmal pathway. This was proved in our study also. This was in accordance with a study done by Katsutoshi Goto,10 et al. in homonymous hemianopia caused by post-geniculate lesions using spectral-domain optical coherence tomography, where they found that in contralateral eyes temporal and nasal RNFL thickness was reduced at the end of 24 months. There was statistically significant thinning only in nasal RNFL quadrant (p value-0.035) of contralateral eyes. This may be because of the fact that superior, inferior and temporal RNFL quadrants receive fibres from both nasal and temporal hemiretinae, wheres nasal RNFL consists of fibres only from nasal hemiretina.
In our study, average RNFL thickness was reduced in the contralateral eyes compared to ipsilateral eyes. (p value-0.290). This may be because of greater proportion of decussated fibres in the retrochiasmal pathway.
Ganglion cell complex thickness parameters:
In our study, sector wise GCC comparison showed that GCC thickness was significantly lower in nasal sectors of contralateral eyes compared to ipsilateral eyes.(statistically significant thinning in inferonasal(p value-0.00) and superonasal (p value-0.019) sectors in contralateral eyes) also GCC was thinner in temporal sectors of ipsilateral eyes compared to contralateral eyes. (statistically significant thinning in inferotemporal sector (p value-0.031) of ipsilateral eyes).
In the ipsilateral eyes, mean temporal GCC was thinner compared to mean nasal GCC-this was found to have borderline statistical significance (p value 0.059). In the contralateral eye mean nasal GCC was thinner compared to mean temporal GCC. This was not statistically significant, but clinically significant.
Average nasal GCC was thinner in contralateral eyes compared to that of ipsilateral eyes. Average temporal GCC was thinner in ipsilateral eyes compared to contralateral eyes. Though clinically significant, these were also not statistically significant.
Average GCC thickness was reduced in contralateral eyes compared to ipsilateral eyes, but not statistically significant. This may be because of greater proportion of decussated fibres in retrochiasmal pathway (53% of total fibres).
We also observed that GCC thickness map shows homonymous pattern of thinning in eight patients which corresponds to their field defect. The normal donut pattern of GCC around fovea is lost respecting the vertical meridian in these patients.
Our findings in GCC thickness analysis was in accordance to the retrospective study on retrograde degeneration of retinal ganglion cells in ischemic occipital cortex lesions, conducted on 9 patients by Jindahra et al,11 who found out that there exists a functional correlation between sector thinning of the GCL and the sensitivity loss of the in the corresponding visual field. They found a significantly stronger correlation between the VF defect and the thickness of GCL rather than that of the peripapillary RNFL. A case report of 3 patients with Posterior cerebral artery infarction, published by Yamashita et al,12 says that GCC correlated better than RNFL with visual field defects, same as our findings. Johannes Keller et al,13 did a retrospective analysis of 8 patients with retro geniculate lesions where they tried to analyse the association between GCL thickness and peripapillary RNFL thickness with each quadrant of the VF, They found a strong correlation between the corresponding macular segment of the GCL and the Visual fields.
This is probably due to the fact that at the macula, the cell bodies of the neurons are more numerous and topographically organised to correspond to the visual field. But the anatomical distribution of fibres in the peripapillary RNFL is more complex, making a correlation with the visual field more difficult to establish. Also, peripapillary RNFL is not symmetric at baseline in normal subjects, the inferior quadrant is thickest, followed by the superior, nasal, and temporal. The absence of blood vessels or other structures in the perifoveal region results in better OCT image acquisition unlike peripapillary region.14
The fovea represents the physiologic division between crossed and uncrossed fibers to the visual cortex, and at baseline perifoveal thickness is symmetric between the superior, inferior, nasal, and temporal quadrants.15 For these reasons, the GCC analysis is a more straightforward way to demonstrate thinning as it is projected to the visual cortex and measured by a visual field. The GCC has been shown to be a more sensitive marker of inner retinal thinning than the RNFL in many diseases like Glaucoma and Multiple Sclerosis.16, 17 GCC temporal to the fovea in the temporal hemiretina comprise strictly retinal ganglion cell elements that reside within the corresponding areas. The same is true with nasal GCC. Such enrichment in retinal ganglion cell components, as well as stringent retinotopical segregation renders GCC superior to the cpRNFL in the detection of homonymous hemianopic atrophy of the GCC due to retrogeniculate pathologies.18
Conclusion
Our study shows that there is clear cut evidence of retrograde trans synaptic degeneration in patients with retrogeniculate lesions which manifest as GCC thinning respecting the vertical meridian with contralateral nasal RNFL thinning also. Those patients who have concurrent diseases like Glaucoma, Diabetic retinopathy, Age related macular degeneration etc, the Ganglion cell loss cannot be solely due to these diseases. The axonal loss is contributed by the posterior visual pathway lesion also. This should be kept in mind while evaluating progression of such diseases using OCT.