- Visibility 99 Views
- Downloads 9 Downloads
- DOI 10.18231/j.ijceo.2021.119
-
CrossMark
- Citation
Retrobulbar neuritis associated with empty sella syndrome: A diagnostic challenge
- Author Details:
-
Abhishek Agarwal *
-
Manisha Kataria
Introduction
Empty sella is a radiological or pathological finding, in which sella turcica is filled with cerebrospinal fluid (CSF) which may lead to compression and flattening of pituitary gland.[1], [2] Empty sella is usually asymptomatic but can cause visual field defects and/or loss of pituitary endocrine functions. Vision loss in some patients with empty sella may also be due to primary ocular or optic nerve pathology and such distinction can be challenging.[3] We report a case where RBN was the cause of acute vision loss in a patient with ESS, which caused diagnostic confusion and responded dramatically to systemic steroids.
Case History
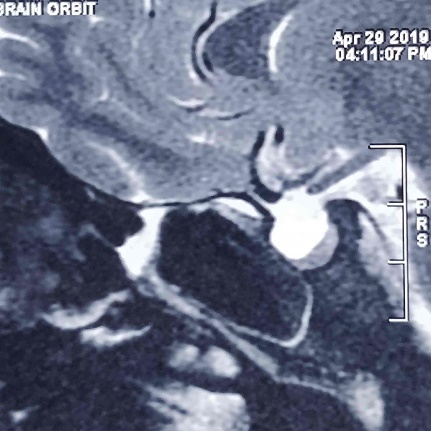
A 35-year-old Indian female presented with painless, sudden diminution of vision in right eye (RE) since 15 days. There was no prior history of craniocerebral trauma, brain tumor, neurosurgery, hormonal treatment, radiotherapy or any other systemic illness. She was married and had two children aged five and seven years. Patient was of average built, well oriented to time, place and person. Systemic examination including neurological examination was normal. Visual acuity in the RE was counting finger at half meters and left eye (LE) was 6/6. Colour vision examination revealed red green colour defect in RE and normal colour vision in LE. RE showed grade III RAPD. Slit lamp examination, intraocular pressure and fundus examination were normal in both eyes. MRI imaging of brain and orbit showed empty sella with pituitary gland lying along the floor ([Figure 1]). Hormonal study showed normal serum levels of growth hormone, prolactin, luteinizing hormone, follicle stimulating hormone, thyroid stimulating hormone and adrenocorticotropic hormone. Neurosurgical reference was sought and no neurosurgical intervention was advised for ESS. We suspected RBN as cause of acute loss of vision and prescribed intravenous methylprednisolone in dosage of 1000 mg in 100 ml saline once daily for three days followed by oral steroids as per ONTT, which demonstrated that intravenous methylprednisolone 1000mg/day for 3 days, followed by oral prednisone 1mg/kg/day for 14 days, sped visual recovery.[4] After 15 days, vision in RE improved to 6/12.
Discussion
Empty sella is characterized by herniation of the subarachnoid space into the sella turcica. Consequently, the sella turcica is filled with CSF and flattening of the pituitary gland at its base. [1], [2] Empty sella can be classified according to its etiology as primary or secondary. Primary empty sella is usually the result of intracranial hypertension with or without insufficiency of the sellar diaphragm. In addition, involution of hyperplastic pituitary after pregnancy and lactation can lead to development of primary empty sella, which accounts to significant higher prevalence of this condition in females. Secondary empty sella occurs secondarily to pituitary surgery, radiotherapy, trauma, apoplexy or Sheehan’s syndrome.[5], [6], [7] Our patient was female who had history of two uneventful pregnancies and no significant past medical history which suggests that empty sella was likely primary in etiology.
Empty sella is usually asymptomatic and is detected in neuroimaging studies as an incidental finding.[7], [8] In symptomatic patients, empty sella can lead to neurological, ophthalmological and endocrinal dysfunction. Neurological symptoms include headache, rhinorrhea, syncope or convulsions.[5], [7] Endocrine dysfunction includes hyperprolactinemia leading to oligomenorrhea or sexual dysfunction and/or panhypopituitarism.[5], [6], [7] Ophthalmic problems caused by empty sella include papilledema, diplopia and loss of visual field and/or visual acuity.[7], [9] Visual loss can be ascribed to empty sella when it leads to damage of suprasellar optic neurons either due to mechanical trauma or vascular insult.[3] However, in most cases of empty sella, visual function remains normal.[3], [7] Moreover, vision loss in some patients with empty sella can be due to primary ocular or optic nerve pathology and such distinction can be challenging.[3] In our case, since the loss of vision was acute and there was no evidence of acute change in morphology of sella turcica like hemorrhage, trauma or ischemia along with no pathological findings in RE and visual cortex, we ascribed loss of vision to RBN and treated the patient accordingly with intravenous steroids followed by oral steroids. Vision improved promptly to 6/12 after 15 days, substantiating our diagnosis of RBN.
Since empty sella is a relatively common finding,[3], [10] at some point in their career most ophthalmologists will face the problem of a patient with unexplained acute visual loss and an empty sella on neuroimaging, which can cause diagnostic confusion. Our case highlights this problem and prompts us to seek an alternative ocular or neuro-ophthalmic pathology in cases where ESS does not corroborate with visual loss. Our case reports that RBN can cause acute loss of vision in patients with empty sella. Furthermore, we found that systemic steroids were effective in treatment of RBN associated with ESS.
Source of Funding
None.
Conflict of Interest
None.
References
- W Busch. Morphology of sella turcica and its relation to the pituitary gland. Virchows Arch 1951. [Google Scholar]
- MSF Mclachlan, ED Williams, FH Doyle. Applied anatomy of the pituitary gland and fossa: a radiological and histopathological study based on 50 necropsies. Br J Radiol 1968. [Google Scholar]
- PG Griffiths, M Dayan, A Coulthard. Primary empty sella: cause of visual failure or chance association?. Eye 1998. [Google Scholar]
- RW Beck. The Optic Neuritis Treatment Trial. Arch Ophthalmol 1988. [Google Scholar]
- MK Auer, MR Stieg, A Crispin, C Sievers, GK Stalla, A Kopczak. Primary Empty Sella Syndrome and the Prevalence of Hormonal Dysregulation. Dtsch Arztebl Int 2018. [Google Scholar]
- D Miljic, S Pekic, V Popovic, KR Feingold, B Anawalt, A Boyce. Empty Sella. Endotext 2000. [Google Scholar]
- LD Marinis, S Bonadonna, A Bianchi, G Maira, A Giustina. Primary Empty Sella. J Clin Endocrinol Metab 2005. [Google Scholar]
- M Guitelman, NG Basavilbaso, M Vitale, A Chervin, D Katz, K Miragaya. Primary empty sella (PES): a review of 175 cases. Pituitary 2013. [Google Scholar]
- J Wang, N Hui, Y Fan, X Li, N Sun. A case of papilloedema caused by primary empty sella turcica syndrome. Yan Kexue Bao 2008. [Google Scholar]
- J Debnath, R Ravikumar, V Sharma, KPS Senger, V Maurya, G Singh. Empty sella on routine MRI studies: an incidental finding or otherwise?. Med J Armed Forces India 2016. [Google Scholar]
