Introduction
Retinal vasculitis is one of the uncommon ocular disease noted more commonly in young adults. Predominantly seen in young male patients more compared to female. Patients present with various stages of disease. Management depends on the clinical presentation. Medical and surgical management is required in these patients based on the manifestation of the disease. Few cases presented with aggressive changes of retinal vasculitis showed poor outcome. Cases of infective aetiology had more proliferative component compared to non-infective. Retinal vasculitis can occur as primary due to various causative factors or secondary to posterior uveitis. Meticulous workup is very important to treat the primary cause and prevent the reoccurrence of activity.
Materials and Methods
Fiftyone patients of retinal vasculitis presented with various causes were studied. All patient’s data collected from medical records. Retrospective study done by collecting data from January 2016 to December 2020. Mean age of presentation was 24 plus or minus 2 years. Predominantly noted in male gender, females also presented with retinal vasculitis. All patients were registered with their consent for the study. After taking proper history, patients underwent detailed ocular examination. BCVA was documented, common symptom was blurred vision in most of our cases, few presented with sudden painless loss of vision. Slit lamp examination, fundus examination, Fundus fluorescein angiography(FFA), OCT, B Scan in cases with hazy media and documentation done. Uveitis workup and other systemic workup done to know the cause of the disease. Primary or secondary retinal vasculitis was diagnosed based on the clinical presentation. Oral steroids were the main part of the treatment to control inflammation, steroids were tapered based on the clinical activity of the disease. ATT and oral steroids considered in cases where tuberculin skin test was positive. Six patients(11.7%) were HIV associated opportunistic infections showed frosted branch angitis, ocular tuberculosis with co-existing HIV infection was diagnosed in three patients and managed with HART and ATT. Patient with moderate vitreous haemorrhage was treated with oral steroids and observed, once the haemorrhage cleared pan retinal photocoagulation done, followed every month till the activity ceased, afterwards every three months to check any reactivity. Patients presented with dense vitreous haemorrhage were started on oral steroids and planned pars plana vitrectomy two weeks after steroid therapy. Patients presented with recurrent vitreous haemorrhage, extra macular tractional retinal detachment causing frequent vitreous haemorrhage and combined retinal detachment underwent pars plana vitrectomy with or with without silicone oil tamponade. Patients with active proliferative vascular membranes underwent anti VEGF 3 three days before surgery followed by vitrectomy, endo laser and oil tamponade. Silicone oil removed after 3 months in all injected cases.
Results
Retinal vasculitis is inflammation of retinal vessels, may be due to infective aetiology, non-infective or only idiopathic inflammation of retinal vessels. It can also occur secondary to intra ocular inflammation. Aim of our study is to study the primary retinal vasculitis cases. We concentrated mainly on the clinical presentation, outcome after management and also the sequelae changes that occurred in our cases after management.
Table 1
Clinical profile of the study
Table 2
Medical management
|
Medical Management (ORAL STEROIDS + PRPC) |
|
|
Number of cases |
16(31.37%) |
|
male |
12, BCVA 6/6 |
|
female |
4, BCVA 6/12 |
Table 3
Surgical management
Discussion
Retinal vasculitis is inflammation of retinal vessels, may be due to infective aetiology, non-infective or only idiopathic inflammation of retinal vessels. It can also occur secondary to intra ocular inflammation. Aim of our study is to study the primary retinal vasculitis cases. We concentrated mainly on the clinical presentation, outcome after management and also the sequelae changes that occurred in our cases after management.
Management was easy in cases who presented in inflammatory and ischemic stages. Pan retinal photo coagulation was done in these cases. All these cases were observed and followed till the activity ceases. After wards they were regularly followed every three months for one year and later every year. Patients who underwent vitrectomy for dense vitreous haemorrhage also showed good outcome after photo coagulation.
Few young adults especially between 20 to 25 years showed poor outcome due to strong adhesion of hyaloid to retina, risk of breaks were common with these patients while stripping hyaloid. Hyaloid is tightly adherent in few cases, stripping of hyaloid causes profuse intra operative bleed if surgery is planned without reducing inflammation with steroids. Cases where anti VEGF injection given before surgery also caused profuse intra operative bleed during vitrectomy. Steroids are considered as the main stay of both medical and surgical management.
Residual anterior hyaloid can cause proliferation and leads to retinal detachment, vitreous haemorrhage and neo vascular glaucoma. Residual hyaloid can be fibrosed, proliferate and cause traction on retina. Remissions and relapses occurred in few cases, these cases had very poor prognosis.
Role of anterior retinal cryopexy to control the recurrent vitreous haemorrhage done in few cases, anterior retinal cryopexy has important role to treat extreme peripheral neovascularisation areas which is not possible with laser therapy.
Patients presented with combined retinal detachment underwent vitrectomy and silicone oil tamponade. Anatomical outcome was good but visual outcome in one patient was not favourable, probably due to prolong ischaemia of retina.
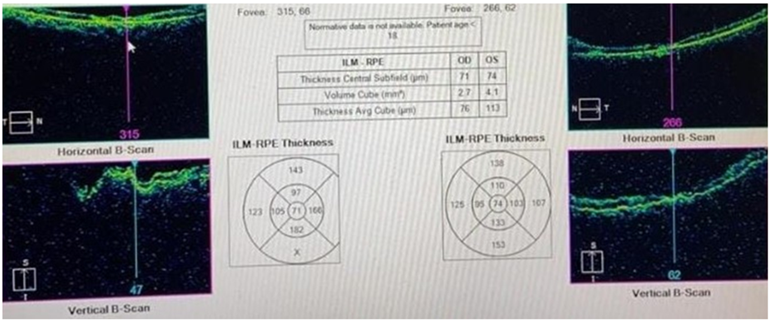
Ischemic retinal vasculitis is one clinical entity which has very poor prognosis which we noted in patients with SLE retinopathy and also in Z positive patients. SLE patients presented with multiple cotton wool spots and arteriolar occlusion, Z positive patients presented with atrophic pale retina, attenuated vessels, sclerosed vessels and atrophic macula with thinned out inner retinal layers. CD4 count in these patients was between 100 to 220 cells per cumm (Figure 1).
Figure 1
Both eyes OCT showing thinned out inner retinal layers and loss of foveal contour in Z positive patient presented with occlusive vasculitis
Cell-mediated immunity also plays a role in the pathology of retinal vasculitis, with CD4+T cells documented within and around the retinal vessels.1 The retina has high metabolic demand for oxygen that is normally met by a highly efficient vascular supply. Insufficiency of the retinal circulation causes neuro retinal dysfunction and degeneration. Focal retinal ischemia causes damage of retinal neurons and cellular death by apoptosis or necrosis with dysfunction and degeneration of the inner retina and finally visual loss.1
Occlusion of retinal vessels will cause VEGF production, hypo perfusion which later leads to increase vascular permeability causing macular and retinal edema and eventually retinal neovascularisation and proliferation. These incidence is common with auto immune and infective etiology patients. Patients with non-infective and idiopathic etiology have good prognosis due to better perfusion of retina.
Autoimmune processes considered as one of cause when retinal vasculitis occurs without systemic manifestations, but the exact etiology remains unknown.2
Macular ischemia, branch retinal vein occlusion, central retinal vein occlusion, branch retinal artery occlusions, persistent neo vascularization, vitreous haemorrhage, and tractional retinal detachment are the common complications associated with poor prognosis.
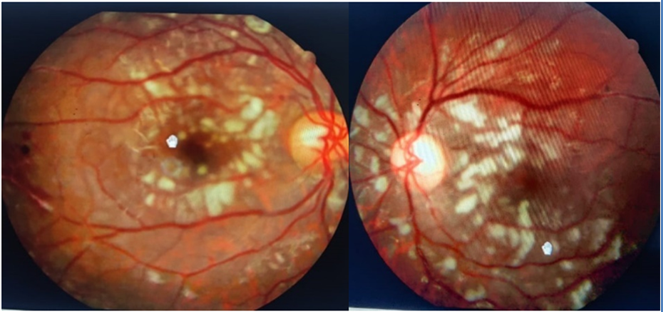
SLE related retinal vascular changes noted in three patients, one female presented with central retinal artery occlusion, one female presented with peri vascular exudates, her angiography showed vessel staining and leak, one male patient presented with multiple cotton wool spots in the posterior pole and peripheral vessel occlusion in both eyes. All the three patients were young adults, age group between 18 to 21 years (Figure 2 A,B).
Figure 2
Both eyes colour fundus picture of SLE showing multiple cotton wool spots in the posterior pole
Twelve patients were referred from rheumatology department for fundus examination, five patients were SLE (41.66%), SLE patients showed ANTI NUCLEAR ANTIBODIES immunofluorescence assay revealed homogenous pattern, intensity + 4, associated antigens involved ds DNA, Histones, ANTI DS DNA Antibody(ELIZA) – Negative. Patients were treated with Mycophenolate mofetil 5oomg and hydroxyl chloroquine 200mg.
Two patients (16.6%) were rheumatoid factor positive, presented with central retinal vein occlusion, OCT showed CMT 700 micro meters, huge SRF at macula, treated with anti VEGF, after some time patient developed neo vascular glaucoma, PRP done, anti-glaucoma medication started, after 3 months she developed multiple fibro vascular membranes on retina, prognosis explained to patient regarding the outcome.3
Tubercular vasculitis is usually present as peripheral vasculitis and the posterior pole vessels are more commonly involved in vasculitis secondary to a viral etiology.4 In our study central vasculitis was involved in three cases. Central Eales disease is a rare condition, prognosis is poor due to direct involvement of the posterior retina.
Tubercular retinal vasculitis was common among the infective cases, patients were diagnosed based on the skin test, treated with ATT regimen for 6 to 9 months, most of these patients showed good result, one or two cases showed reactivity after completion of ATT. Patients with induration and erythema of more than 15mm considered as positive patients.
Most of our patients presented with retinal peri vascular exudates, vascular sheathing, vitreous haemorrhage, few cases presented only with branch retinal vein occlusion without any peripheral vascular changes. Peripheral retinal disease is asymptomatic in initial stages. Central Eales disease will manifest early compared to peripheral Eales disease. Periphlebitis noted in 3 male patients.
India is endemic country for tuberculosis, there is no confirmatory test for tuberculosis, mantoux test is usually positive in Indian population, may be due to frequent exposure and secondary to BCG vaccination. Systemic anti-tubercular treatment was initiated with 600 mg of Isoniazid 450 mg of Rifampicin, 1200 mg of Pyrazinamide and 750 mg of Ethambutol along with oral prednisolone at 1 mg/kg body weight and topical prednisolone acetate (1%) eye drops four times a day in cases with vitritis and AC reaction.4 Patients who were on irregular management of ATT showed the reoccurrence, again managed with steroids and planned ATT.
Central eales presents as oedema of the optic nerve-head and adjacent retina, generalized dilatation of the retinal veins, little or no involvement of the retinal arteries, a variable amount of retinal haemorrhage, and an almost complete absence of vitreous haemorrhage and retinitis proliferans5 (Figure 3 A,B). Other infective cases reported were post-operative endophthalmitis (POE) and ocular toxoplasmosis (OT), OT presented with peri arterial exudates and also showed satellite lesion near the old healed scar in the macular area, initially due to severe vitritis only the scar with active lesion noted, after two weeks once the vitritis resolved the peri vascular exudates were seen. Management done in these cases was oral Azithromycin 500mg per day for five to seven days with oral steroids.
In POE and post traumatic endophthalmitis peri vascular exudates were noted after completion of vitrectomy, started oral steroids after physician clearance, visual outcome was not much favourable. In these cases, retinal vasculitis was secondary to the infection and inflammation in vitreous cavity. In non-infective aetiology, major percentage of the patients showed all ocular and systemic workup within normal limits, prognosis was also good in most of these cases.
One female patient presented with retro bulbar neuritis(RBN), managed with intra venous methyl prednisolone and oral steroids, after two years again she presented with blurred vision, headache and hearing loss, referred to neurophysician, diagnosed as Susac syndrome. Susac syndrome is a rare condition where microangiopathy affects the arterioles of the brain, retina, and cochlea, giving the classic triad of encephalopathy, branch retinal arterial occlusions, and sensorineural hearing loss. The underlying process is believed to be a small-vessel vasculitis causing micro infarcts of the retina, brain and cochlea.6
IRVAN was one condition reported in three male and one female patients, all were young adults, managed with anti VEGF, PRPC and steroids. FFA showed hyper fluorescence of arterial macro aneurysm, temporal peripheral wide capillary non perfusion areas and macular edema.
According to published literature female preponderance is common, in our study male preponderance is noted and unilateral presentation was common. The disease has a slight female preponderance, with an average age at presentation of 30–40 years. It is usually an asymptomatic disease, but if left untreated may lead to severe visual loss. It is usually bilateral, but a few cases of unilateral presentation have also been reported and a few cases where it was unilateral at presentation can also involve both eyes later.7
In cases of IRVAN, arterioles are commonly involved, associated with multiple aneurysmal dilatations of the retinal and optic nerve-head arterioles. These peculiar vascular anomalies measure 75–300 µm in diameter, and are present at or near major branching sites on retinal arterioles.7
Multiple sclerosis (MS) and Susac syndrome cases were referred to neuro physician and managed by the neurologist. These cases are rare but requires proper workup to prevent blindness in young adults. When uveitis patient is examined, Ophthalmologist always has to keep systemic diseases in mind at the time of evaluation. Uvea and optic nerve are commonly affected; rarely bilateral retinal vessels are also involved causing bilateral retinal vasculitis.
Prevalence of MS associated uveitis is 0.9 to 1.7%, recent studies shows increase in frequency 0.65% to 36.7%. Although uvea has no myelin then reason for the involvement is partially common embryonic neuro ectodermic origin and association with HLA DR15.Posterior segment manifestations like retinal vasculitis, has been found between 10% and 35% of patients with MS, but retinal neovascularization is an uncommon complication.8
One male patient was a case of AML presented with peculiar fundus picture showing leukostasis retinopathy as manifestation of the primary disease but complete workup revealed haematological malignancy, referred to medical oncologist for further management.
Retinal vasculitis can occur as an isolated condition in leukaemia patients at the time of relapse. Retinal manifestations in pre-existing ALL are frequent, but in this case patient developed blurred vision first, after work up haematological malignancy was diagnosed. “Leukemic retinopathy” is a term used to describe vascular features secondary to severe anaemia, thrombocytopenia, andhyper viscosity rather than to direct leukemic infiltration.9
One female patient with atypical retinitis pigmentosa presented with sudden drop of vision, FFA revealed exudative retinopathy, staining of vessels and leak from peripheral retinal vessels, started on oral steroids, there was dramatic improvement in vision. Retinal exudates in our case may be due to inflammation which usually occurs in Retinitis pigmentosa patients and cause macular edema, in our case there was inflammation of retinal vessels causing break down of blood ocular barrier and leading to the leak from vessels. Control of inflammation may help in constructing the blood ocular barrier and reduces exudative retinopathy.
Aetiology could be any vaso occlusive event, autoimmunevasculopathy, or chronic inflammation causing structuraldamage to vasculature which may precede the development of retinal telangiectasia. The Coats’ like response occurred because of damage to the retinal vasculature secondaryto inflammation.10
Conclusion
Retinal vasculitis is one group of ocular disease where young adults are effected, management depends on the presentation of clinical stage, meticulous workup is required to exclude the cause, major part of management depends on the cause of the disease. Can occur as primary or secondary due to uveitis, in our study we concentrated mainly on the primary retinal vasculitis cases. Genetic causes not excluded in our study, patient where poor prognosis noted requires complete workup to prevent the blindness in young adults. Cases with aggressive presentation and bad prognosis need tobe studied in detail to know the causative factor.



