Introduction
DED is a chronic pain syndrome affecting quality of life adversely in patients and even affecting outcome of surgeries for cataract, refractive errors and glaucoma.1 It is characterised by instability of the tear film, with or without inflammation of the ocular surface and lacrimal glands2 and accompanied by increased osmolality of tear film and inflammation of the ocular surface.2, 3, 4
The dry eye workshop study classifies dry eye as:3
Aqueous deficient dry eye i.e. failure of lacrmal tear secretion as seen in Sjogren’s syndrome, lacrimal gland deficiency, lacrimal duct obstruction, reflex blockage or as a result of systemic drug toxicity.
Evaporative dry eye due to excessive evaporation of the aqueous component secondary to deficient lipid component as seen in meibomian gland dysfunction, lid disorders, contact lens wearers, vitamin A deficiency and topical drug toxicity.
Patients usually present to the ophthalmologist with complaints of foreign body sensation, ocular dryness, ocular grittiness, hyperemia, ocular irritation, burning, itching, photophobia and fluctuation or blurring of vision associated with redness of eyelids and conjunctiva. Ocular examination may reveal stringy mucus and particulate matter in the tear film. Ocular surface becomes lusterless. There is conjunctival xerosis or Bitot’s spots in the conjunctiva and filamentary keratitis may be present.5
Various studies have revealed the inflammatory component to be the main causative factor of the disorder. Cytokine and receptor mediated inflammatory cascade6 and apoptosis have also been implicated in the pathogenesis of dry eyes.7
With a better understanding of the underlying pathogenesis, goal for treatment of patients with DED has shifted from merely improving the patient’s ocular comfort and quality of life to return of the ocular surface and tear film to the normal homeostatic state. Current therapies for the management of dry eye include drugs for tear supplementation, retention and stimulation; anti-inflammatory agents, and environmental strategies.6 Newer techniques include lipiflow8, 9 and punctum occluders.10 Palliative therapies like tear substitutes are currently the most common choice of treatment but have failed to yield high success rates because they give only symptomatic improvement and do not correct underlying cause.6
Chloroquine is a well-known anti-inflammatory drug used in the treatment of rheumatoid arthritis,11, 12, 13 discoid lupus erythematosus,14 and amoebic hepatitis.15 Yavuz et al. conducted a study to evaluate effects of systemic hydroxychloroquine on dry eye disease associated with primary Sjogren syndrome and concluded that there is a significant relief on symptoms of DED.16 In another study by Bhavsar et al., it was observed that chloroquine eyedrops were effective in DED and were infact superior to sodium carboxymethyl cellulose in treatment of DED.17
Since the use of chloroquine phosphate eyedrops in DED has been started recently, there is a dearth of studies to provide evidence regarding its efficacy and drawbacks in management of DED. Hence this study was planned.
Materials and Methods
A single blind, prospective, comparative study was done in 100 patients of either gender, between the age of 30 to 70 years diagnosed with DED after taking ethical clearance from Institutional Ethics Committee. The Tenets of Declaration of Helsinki were followed. Participants were randomly divided into two groups, each consisting of 50 patients. Group-1 patients were given CMC 1% 4 times a day for 12 weeks and Group-2 patients were given CQP 0.03% as the treatment modality 2 times a day for 12 weeks.
Patients with systemic or local ocular diseases known to cause dry eyes or ocular surface abnormalities, patients with history of chronic contact lens wear and ocular surgeries in the past were excluded. Also, patients on local or systemic medications known to cause dry eyes or ocular surface disorders were excluded from the study.
After informed and written consent, a detailed history of ocular complaints was taken as per the questionnaire in Table 1.18
Table 1
Depicting a questionnaire on DED
Answers to these questions were recorded as rarely (at least once in 3–4 months), sometimes (once in 2–4 weeks), often (at least once a week) or all the time. Presence of one or more symptoms often or all the time were taken as positive.
After a brief general and systemic examination detailed ocular examination was done which included recording visual acuity with Snellen’s chart, evaluating the condition of lids, Meibomian glands, conjunctival surface and corneal surface. Detailed anterior and posterior segment evaluation was done. The DED profile included TBUT, marginal tear strip evaluation, Schirmer’s 1 test, and staining of ocular surfaces with fluorescein stain, Rose Bengal stain and Lissamine green stain. Van Bijsterveld scoring system was used to grade the staining of cornea and conjunctiva. Asymptomatic patients with positive clinical signs or tests were also considered to have dry eye.
Follow up was done after every 4 weeks for 12 weeks by evaluating symptoms, signs, testing and scoring in both the groups. Grading was assessed by Khurana’s grading system (Table 2, Table 3).
Table 2
Showing scoring system for Khurana’s grading system for dry eye
Table 3
Showing grading of dry eye as per Khurana’s grading system of DED
|
Total score |
Severity of dry eye |
|
0-1 |
No Dry eye |
|
2 |
Dry eye suspect |
|
3-8 |
Mild dry eye |
|
9-13 |
Moderate dry eye |
|
14-18 |
Severe dry eye |
The results were entered into Microsoft Excel sheet and then in SPSS software for statistical analysis. Qualitative data were analysed using Chi square test and quantitative data with student t test. Degree of improvement of parameters on subsequent follow up visits was assessed using repeated ANOVA. Degree of improvement between the two groups was compared using Two Way ANOVA test. Marginal Homogeneity test was used to measure change in severity of parameters.
Observations and Results
The two groups were comparable in terms of age and gender distribution. Maximum patients were from the age group of 61-70 years indicating that DED is a disorder of old age.
It was observed that the mean TBUT recorded in group 1 was better than group 2 in all follow up visits (p<0.001). The degree of improvement of TBUT values after 12 weeks of treatment from pre-treatment level in the two groups was statistically significant (p<0.001); i.e. both the drugs affect TBUT significantly. The rate of improvement in the two groups was also similar (p=0.191), implying that time taken by both the drugs for restoring the TBUT to normal values is almost equal.
Group 1 showed statistically significant improvement in the quality of the Marginal Tear Strip (MTS) between 8-12 weeks (p<0.001) indicating a delayed onset of action of CMC. On the other hand, group 2 showed significant improvement in MTS quality in first 8 weeks followed by a plateau thus showing early onset of action and fast attainment of maximum respite with CQP (p=0.011 in 1st visit, p=0.049 in second visit and p=0.948 after third visit). Maximum improvement achieved with CMC was better than that with CQP (p=0.001 at 12 weeks).
The change in Schirmer’s test values from pre-treatment levels to the levels achieved after 12 weeks of treatment was found to be statistically significant (p<0.001) in both the groups. However, on comparing the rates of improvement of mean Schirmer’s test value in both the groups, a statistically significant difference was observed. (p=0.022). Therefore, it can be safely concluded that the rate of improvement of this parameter of DED is better in group 2 patients treated with CQP although both the drugs are equally effective in terms of the Schirmer’s score at the end point of the study (p=0.172 at 12 weeks).
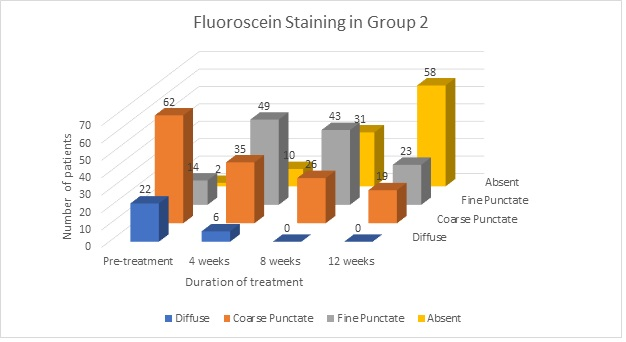
The severity of fluorescein staining (FS) of ocular surface did not change significantly from pre-treatment levels to 8 weeks (p=0.219, p=0.519) in group 1, whereas it improved significantly from 8 weeks to 12 weeks with p = 0.007; thus, suggesting delayed improvement in group 1. In group 2, the FS improved significantly from pretreatment value to 4 weeks and from 8 weeks to 12 weeks (p=0.004, p<0.001) indicating an early and sustained improvement in FS in group 2.
There was no statistically significant difference observed between the two groups on rose bengal staining (RBS) score (p=0.501, p=0.817 at 4 weeks and 8 weeks and p=0.680 at 12 weeks). On comparing the rates of improvement of mean RBS value in both the groups using Two Way Repeated ANOVA measures test, no difference was observed (p=0.054). Therefore, it can be concluded that the degree of improvement of this parameter of DED is similar with both the drugs. Therefore, the drugs improve RBS score with equal efficacy.
The difference in the rates of improvement of mean Lissamine Green test value in both the groups using Two Way Repeated ANOVA measures test was statistically significant (p<0.001). Therefore, the degree of improvement of Lissamine Green staining score in DED is better in group 2 patients treated with CQP than with group 1 patients treated with CMC.
The severity of DED was graded into mild, moderate and severe according to the Khurana’s grading system and was compared at each follow up. In both the groups, the improvement in severity of DED was significant from pre-treatment to 12 weeks post treatment (p<0.001). The observed p value at 4 weeks was 0.058 indicating no significant difference between the two groups whereas a significant difference was observed at 8 weeks and 12 weeks (p=0.005, p=0.009). Therefore, both the drugs reduce severity of the disease with CQP having faster onset of action.
Discussion
Ageing and post menopause known to be associated with DED. In a study conducted by Kinoshita et al., on a total of 308 patients with dry eye, the mean age was 55.2 years.19, 9 However, Shah et al. have reported a younger age of onset. The current study shows that the maximum number of patients were in age group of 50 to 70 years of age with mean age of patients being 50.98 years.
Post-menopausal women are at increased risk of developing DED as they develop hormonal imbalances between estrogen and androgens. This excites inflammation in lacrimal gland and ocular surface, disrupting the normal homeostatic maintenance of the lacrimal gland and ocular surface.20
Statistically significant improvement was seen as early as 4 weeks of treatment in group-1 as well as group-2 as compared to their baseline values in terms of the TBUT values and this improvement continued over the period of 12 weeks of treatment (Figure 1 and Figure 4). On comparing the rate of improvement between the two groups, it was found that there was no statistically significant difference suggesting similar efficacy of both CQP and CMC eye drops in improving tear film stability. No relevant study was found comparing TBUT between the two drugs after thorough literature research.
On analyzing the Marginal Tear Strip, we found that both the groups had statistically significant improvement beginning as early as 4 weeks of treatment in group-1 (CMC) and group-2 (CQP) which persisted over the period of 12 weeks (Figure 2 and Figure 5). The rates of improvement between the two groups were also not significantly different, thus suggesting similar results of both CQP and CMC eye drops in improving tear film integrity.
Both the drugs effectively increase the amount of tear film levels as evident by the improving Schirmer’s values in both the groups (Figure 1 and Figure 4). The difference between the two groups was statistically significant at 4 weeks and 8 weeks follow up visit but not at 12 week visit. This implies that Chloroquine Phosphate group showed early improvement than CMC group. However, overall improvement in tear film at the end of 12 weeks was similar in both groups. In a similar study conducted by Bhavsar et al.,17 significant changes in Schirmer’s test value were reported and it was concluded that both drugs are efficacious but CQP is more efficacious than CMC. These findings are not consistent with our study.
Rose Bengal staining values changed significantly within both the study groups at every follow up visit (Figure 1 and Figure 4) suggesting that both drugs effectively increase the viability of ocular surface cells. It was evident that the difference in change between the two groups was statistically significant at 4 weeks, 8 weeks but not at 12 weeks follow up visit, indicating that CQP group showed early improvement in RBS value than CMC group but the overall outcome of both the drugs was similar on basis of RBS value.
A statistically significant reduction in Lissamine green staining score as early as 4 weeks in both the groups was seen which was continuous over the period of 12 weeks as compared to their pretreatment levels (Figure 1 and 4). Statistically significant better response was seen in group-2 (CQP) as compared to group-1 (CMC).
Bhavsar et al.17 reported significant improvements with CQP treatment in LGSS from baseline 2.79±0.12 to 0.22±0.04 after treatment (p < 0.001) with the net change of -2.57 (95% CI). CMC treatment showed significant change in mean score only at 12 weeks visit i.e. 1.11±0.11 from 1.98±0.13 with a net change of -0.87 (95% CI). The significantly better improvement with CQP in LG staining reported by this study is similar to our study.
We observed in our study that both the groups were comparable regarding the baseline fluorescein staining scores. In CQP group the change in Fluorescein staining at 4 weeks was significant as compared to the CMC group whereas the change was not significant at 8 weeks and 12 weeks follow up. These findings again suggest a faster onset of action of CQP than CMC but equal efficacy after the 12 week follow up period although both drugs improve ocular surface staining with fluorescein (Figure 3 and 6).
The observed difference and better response of CQP in ocular surface staining can be attributed to its proposed mechanism of action i.e. reducing apoptosis of ocular surface epithelial cells and protection of ocular surface epithelial cells from damage of UV rays.
Grading of severity of DED in enrolled eyes was done in both the groups. Eyes with DED were graded into 4 subgroups: No dry eye, Dry eye suspect, Mild, Moderate and Severe. The number of eyes in each sub group were evaluated at each 4 weekly follow up visit. It was evident that patients with severe DED showed the least improvement in both the groups. It suggests that mono-drug therapy is least effective in treatment of severe DED and multi drug therapy should be used early in treatment of severe DED.
Conclusion
On the basis of all the above observations, it can be inferred that both CQP and CMC are equally effective in treating DED, although faster onset of action was observed with CQP on ocular surface staining tests and Schirmer’s test. Lissamine green was the only test showing CQP to be better than CMC at every follow up visit. We therefore suggest regime consisting of initial management with CQP followed by maintenance with CMC as patient will have faster and sustained relief with cause effectiveness of the regime.
Differences in findings can be attributed to different mechanisms of action of CMC and CQP. CMC acts as an eye lubricant with little effect on pathophysiology of DED. CQP is postulated to act as an anti-inflammatory and also has an anti-apoptotic effect on ocular surface epithelial cells. This might be the reason behind early improvement in ocular surface staining scores in the CQP group. However, further studies at a larger scale need to be done to corroborate the findings of our study.