- Visibility 147 Views
- Downloads 23 Downloads
- DOI 10.18231/j.ijceo.2021.044
-
CrossMark
- Citation
Pediatric normative Retinal nerve fiber layer thickness in south Indian population
- Author Details:
-
Sunil Ganekal *
-
Varun Ganekal
Introduction
The diagnosis and follow-up of children with an ocular disease is more difficult than that of adults because of the challenge in obtaining reliable and reproducible visual examinations. Important diagnostic tools used in adults, such as visual fields, require their cooperation. For children, such tools are often impractical because the results are unreliable, and hence difficult to interpret However, OCT provides objective measurements of the affected structures. Generally, children older than 3 or 4 years of age can cooperate sufficiently. Macular measurements are even easier to obtain than those of the optic nerve, making OCT particularly suitable for use with uncooperative children or those with poor fixation. The potential value of OCT in diagnosis of childhood glaucoma has also been demonstrated recently.[1]
OCT provide objective information of optic disc configuration and/or RNFL thickness and may represent valuable tools in the evaluation of children with subnormal vision and in children with known diseases that may affect the optic nerve, such as craniopharyngioma and glioma. In children with binocular subnormal vision, a normal database is necessary for purposes of comparison. Similarly, in order to assess children with monocular subnormal vision, we need to know the normal range of differences between the two eyes. Normal databases have been established for both HRT and OCT, but these have been determined in adults and may not be applicable to children.[2] Hence we did this study to assess the normal RNFL thickness in south Indian pediatric normal.
Materials and Methods
Prospective observational OCT based study of 200 eyes of 100 children who presented to the ophthalmic outpatient department from November 2017 to August 2019. The study was approved by the Institutional review board. Any child aged 5 years to 18 years but cooperative for OCT with no asymmetry in cup-disc ratio and without optic nerve head abnormalities were included in the study. Children with strabismus or amblyopia, abnormalities of the disc or the retinal nerve fiber layer, Family history of glaucoma, any other hereditary eye disease, history of intraocular surgery or any kind of laser therapy, Mentally challenged children with neurological, metabolic or vascular disorders, systemic disease possibly affecting the eye, Ocular media opacity, Best-corrected visual acuity of less than 20/30, hypermetropia more than +5D and myopia more than –5D or astigmatism ≥ 2D were excluded from the study.
A detailed history including demographics, information on past medical illness and drug intake and their duration was recorded. Ocular diseases if any was noted. The complete Ophthalmological examination was done in all children. Vision was assessed carefully using Snellen's chart. Pupil was also tested for any afferent pupillary defect, which grossly tests optic nerve function and retinal functions. cycloplegic refraction was done in relevant cases. A thorough examination of the eyes was carried out under slit lamp. Fundus evaluation was done using Direct and Indirect ophthalmoscope with special attention to any opacity in the lens, vitreous hemorrhage and retinal detachment.
Spectral-domain OCT was performed with the Cirrus HD-OCT-500. This has an acquisition rate of 27,000 A-scans per second. The protocol used for RNFL assessment was the optic disc cube where a 3.46 mm circular scan is placed around the optic disc and the information about parapapillary RNFL thickness is obtained whereby 27,000 A scans are acquired per second. All images were reviewed and only images with good signal strength with no movement artifact were included for the study. The parapapillary RNFL thickness parameters automatically calculated by the Cirrus software and evaluated in this study included average/full circle thickness — RNFL-FC (360º measure), temporal quadrant thickness, RNFL-T, superior quadrant thickness, RNFL-S, nasal quadrant thickness, RNFL-N, inferior quadrant thickness, RNFL-I. Three such circular scans were performed successively. The average of the 3 scans was used in the analysis. All scans were performed by the same investigator. Mean RNFL thickness in micrometers along the whole circle circumference, four quadrants, 12’o clock hours were obtained.
Both eyes of every subject were selected for statistical analysis. Data were entered in a excel sheet, and then transferred to the statistical package for social science program for data management and analyses. Results were expressed as mean ± SD, range and normal value (95% confidence intervals) calculated according to age, gender and laterality of eyes. Unpaired t-test was used to compare between two groups (male v/s female, right eye v/s left eye). Correlation and regression analysis was done to assess the relationship between RNFL and clinical parameters (age, sex and refractive error). A P-value 0.05 or less was considered for statistical significance. SPSS (version 16) software was used for all the analysis.
Results
The age of the patients in this study ranged from 5 to 18 years with the mean of 13.3 ± 2.4 SD. There were 14 children in age group between 6-10 years, 56 children in age between 11-14years and 30 in the age group between 15-18 years. The study had 65 males and 35 females. The unaided visual acuity of all the eyes ranged from 6/6 (log MAR 0.0) to 6/36 (log MAR 0.778) with mean refractive error of -0.28 ± 0.91 diopters (range-4 to + 2.5). The axial length varied from 21.7 mm to 25.7mm with the mean of 23.0 ± 0.7 SD. The difference of mean axial length and the refractive error was not statistically significant between the right and the left eyes. Mean Global RNFL thickness and distribution of RNFL in each quadrant shown in ([Table 1]). The mean global RNFL thickness (RNFL-FC) was 97.0 ± 8.8 mm (range 79.4 - 114.6). The RNFL thickness was maximum in the inferior quadrant (RNFL-I) 126 ± 13.7mm followed in order by superior (RNFL-S) 126 ± 16.3mm, nasal (RNFL-N) 70.5 ± 12.3mm and temporal (RNFL-T) 63.4 ± 9.2mm, in both the sexes. Seventy six children had global RNFL (RNFL FC) thickness ranging from 86.0-105.9 µ. When comparing the mean RNFL between both sexes females had thicker RNFL than males ([Table 2]) which was not statistically significant (p<0.37). However, when the nasal quadrant (RNFL-N) between both sexes was compared the mean difference was 4.40 with P value<0.03. The inter-ocular variations in RNFL thickness in normal children measured by SD OCT. The mean global RNFL thickness was 97.7 ± 9.2SD in right eye (range 74.4 - 116mm) and 96.3 ± 8.4SD in left eye (range 79.5 - 113.1). The mean difference in global RNFL thickness between the two eyes was 1.38 with P value <0.27 which showed no statistical significance.
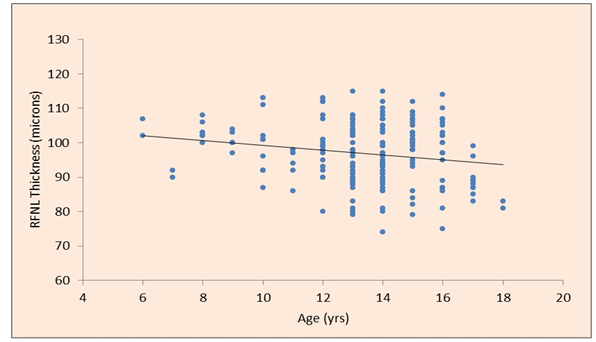
Mean global RNFL thickness and thickness of RNFL in each quadrant according to the age groups shows as age increases the mean RNFL thickness as well the thickness in each quadrant decreases ([Table 3] and [Figure 1]). The RNFL ([Table 4]) thinning was found to be more in the surerior quadrant (RNFL-S). In order to assess the relationship between the age and the RNFL thickness correlation analysis was done. The analysis revealed that there is negative correlation between age and RNFL which shows that there is decrease in RNFL with increasing age (r=0.19). Though this relationship was weak, regression analysis was carried out to know the RNFL reduction for every 1 year increase in age. Analysis revealed that there was reduction of 0.70 micron in RNFL for average increase of one year. Explained variation was found to be (3.6%) R²=0.036(P=0.008).
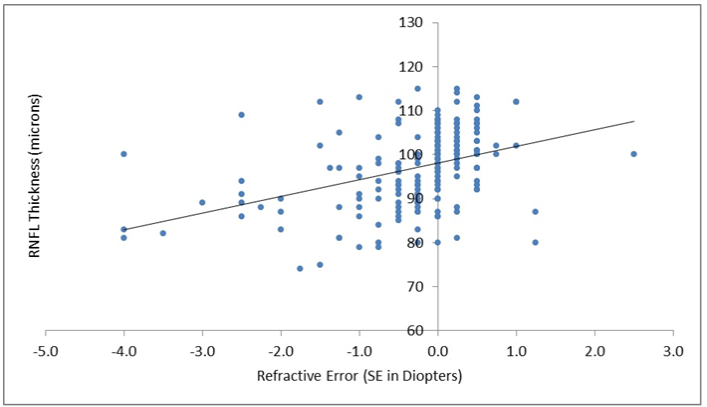
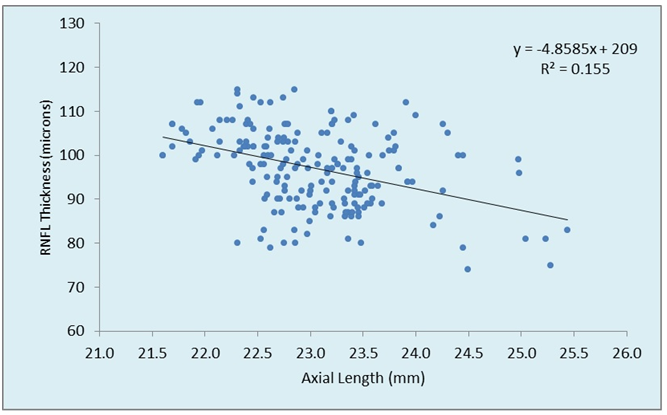
Significant positive correlation coefficient of 0.38 with refraction error in spherical equivalent (SE) with regression coefficient of 3.77 ([Figure 2]). On analysis, it was found that for every increase in one diopter of spherical equivalent the mean RNFL increased by 3.77 microns Explained variation was found to be 15.2% (R²=0.036)(P < 0.001). Correlation and regression analysis between axial length and RNFL thickness revealed negative correlation between axial length and RNFL thickness ([Figure 3]), which shows there is reduction in mean RNFL thickness by 4.86 micron for every 1 mm increase in axial length. The explained variation was found to be 15.2 % (R²=0.155)(P < 0.001). The correlation and regression analysis between RNFL thickness with respect to age, refractive error and axial length are shown in ([Table 4]). Positive correlation was seen with refractive error while inverse or negative correlation was seen with axial length and age.
|
Variable |
Total |
|
|
Mean ± SD (micron) |
Normal range (micron) |
|
|
RNFL-FC |
97.0 ± 8.8 |
79.4 - 114.6 |
|
RNFL-S |
126.2 ± 13.7 |
98.7 - 153.7 |
|
RNFL-I |
127.7 ± 16.3 |
95.2 - 160.2 |
|
RNFL-N |
70.5 ± 12.3 |
46.0 - 95.0 |
|
RNFL-T |
63.4 ± 9.2 |
45.0 - 81.9 |
|
Variable |
Males |
Females |
Males v/s Females |
||||
|
Mean ± SD |
Normal range (micron) |
Mean ± SD |
Normal range |
Mean diff |
t value |
P value |
|
|
RNFL-FC |
96.6 ± 8.9 (micron) |
78.7 - 114.4 |
97.8 ± 8.6 |
80.6 - 114.9 |
1.19 |
0.91 |
0.37,ns |
|
RNFL-S |
126.7 ± 13.5 |
99.6 - 153.7 |
125.3 ± 14.2 |
96.9 - 153.7 |
1.36 |
0.65 |
0.52,ns |
|
RNFL-I |
126.7 ± 16.7 |
93.4 - 160.1 |
129.6 ± 15.4 |
98.9 - 160.3 |
2.85 |
1.20 |
0.23,ns |
|
RNFL-N |
69.0 ± 10.7 |
47.2 - 90.7 |
73.4 ± 14.1 |
45.1 - 101.7 |
4.40 |
2.24 |
0.03* |
|
RNFL-T |
63.9 ± 9.7 |
44.5 - 83.4 |
62.5 ± 8.2 |
46.1 - 78.9 |
1.44 |
1.10 |
0.27,ns |
|
Variable |
6 - 10 Yrs (n = 29) |
11 - 14 Yrs (n = 110)) |
15 - 18 Yrs (n = 61) |
|||
|
Mean ± SD |
Normal range |
Mean ± SD |
Normal range |
Mean ±SD |
Normal range |
|
|
RNFL-FC |
100.2 ± 6.4 |
87.5 - 112.9 |
96.6 ± 8.9 |
78.9 - 114.4 |
96.2 ± 9.4 |
77.4 - 115.0 |
|
RNFL-S |
133.4 ± 15.7 |
102.0 - 164.8 |
124.8 ± 11.6 |
101.7 - 147.9 |
125.5 ± 15.7 |
94.1 - 156.8 |
|
RNFL-I |
130.4 ± 14.9 |
100.6 - 10.1 |
127.0 ± 17.5 |
92.0 - 162.0 |
127.9 ± 14.5 |
99.0 - 156.9 |
|
RNFL-N |
70.6 ± 8.4 |
53.7 - 87.4 |
70.5 ± 12.6 |
45.4 - 95.6 |
70.6 ± 13.3 |
44.0 - 97.1 |
|
RNFL-T |
65.8 ± 7.3 |
51.1 - 80.5 |
64.3 ± 9.8 |
44.7 - 83.8 |
60.8 ± 8.5 |
43.8 - 77.8 |
|
Relationship between |
Corr.Coeff 'r ' |
Regn.Coeff 'ß' |
Relation equation |
R² |
|
Age & RNFL |
-0.19 |
-0.70 |
RNFL = 106 - 0.70 Age |
0.036 (3.6%) |
|
Ref. error & RNFL |
0.38 |
3.77 |
RNFL = 98 ± 3.78 Ref Er |
0.152 (15.2%) |
|
Axl & RNFL |
-0.39 |
-4.86 |
RNFL = 209 - 4.86 Axl |
0.155 (15.5%) |
Discussion
OCT has become widely used tool in clinical and scientific ophthalmology. Its uses in diagnosis of diseases is not restricted only to ophthalmology. Beside its use in identifying macular pathology and glaucoma, in recent year its application to diagnose various ocular conditions has widely been expanded such as multiple sclerosis, optic nerve gliomas, peudotumor cerebri, optic neuritis and papilloedema.[3], [4], [5], [6]
Normative data are provided automatically by OCT but the data base only include individuals 18 years and above limiting its use in children. The application of OCT in children has been documented in several studies.[7], [8], [9], [10] However minimal literature on normative data base exist which would serve as a bench mark for reference and glaucoma scanning.[11] The average RNFL thickness in our study was 97.0 ± 8.8µm. When compared to other studies in the past, the average RNFL of our study was lower to those studies done previously. In a large study conducted by Huynh et al., the average RNFL thickness was 103.7 ± 11.4µm.[12] The average RNFL in our study was lower to those of salchow et al.,[13] Qian et al.,[14] EL-dairi et al.,[7] Leung et al.,[15] and Ahn et al.,[16] Borne et al., compared the OCT 2000 with the Stratus OCT and found that the former model consistently yielded a higher RNFL thickness value.[17] In comparison the study conducted by Elai et al.,[18] Barrio-Barrio et al.,[19] Al-Haddad et al.,[20] using cirrus OCT yielded results that were consistent with our finding. The RNFL thickness varies significantly among types of OCT used and therefore direct comparison of RNFL thickness measurement among OCT instrument like Stratus and Cirrus may be misleading.[11]
The distribution of RNFL thickness (thickest inferiorly and superiorly and thinner nasally and temporally) are in agreement with the normal distribution of RNFL. These variations are the result of the large number of nerve fibres converging to the optic nerve head from the superior and inferior arcuate bundles, relative to the number of fibres converging from the papillomacular bundles and nasal retina. Studies vary as to whether the RNFL was thicker temporally or nasally or whether it was thicker superiorly or inferiorly. In our study it was seen that, in the age group between 5-10 years, superior RNFL was thicker compare to the inferior RNFL, with increasing age more thinning was seen in the superior RNFL compare to inferior RNFL, thinning was also seen in temporal RNFL while minimal changes were detected in the nasal RNFL.[12]
Large number of studies has shown that RNFL thickness decreases as age increases. [21], [22], [23] It has been confirmed by several studies that the number of ganglion cells in human retina decreases with age which results in thinning of the RNFL. This has been confirmed by several investigations using OCT.[24], [25] It has been estimated that normal individual lose ganglion cells at a rate of 4909 per year.[26] Bundez et al., found that RNFL was thinner in older people with decline of appoximately 2 microns per decade.[23] Qian et al.,[14] and salchow et al.,[13] reported that RNFL thickness tends to increase with age in a population younger than 18 years. B Alamouti et al., studied 100 individual to establish changes in RNFL thickness with age in their study.[25] They found highly significant correlation of both the retinal and the RNFL thickness with age. In these study the retinal thickness decreased by 0.53 μm per year. About 80% of the changes in retinal thickness over time are caused by shrinkage of the RNFL. Poinooswamy et al., examined 150 healthy volunteers of different ages using scanning laser polarimetry.[27] They found a progressive reduction of the RNFL thickness with increasing age. The data presented in their study indicate a significant reduction of the RNFL thickness of 0.38 μm/year. In this present study we analyzed that there was mean global decrease in the RNFL, as well as decrease in RNFL in each quadrant with increasing age. The decrease in RNFL was more in superior quadrant compare to inferior quadrant, thinning was also seen in temporal quadrant while it was absent in nasal quadrant. Age was correlated negatively with RNFL thickness. In study conducted by Rajul S Parikh, it was seen that RNFL tends to decrease with age.[28] Average RNFL and RNFL by quadrant decreases especially after 50 years of age. Thinning of the RNFL is not uniform in all with maximum loss in the superior quadrant in comparison to inferior quadrant which is more resistant to loss. These findings were consistent in our studies also.
The effect of refractive error has been widely debated. Many studies have demonstrated positive correlation with spherical equivalent.[12], [13], [14], [29] Huynh et al., studies on 1765 children less than 6 years reported significant trend for thicker RNFL with more positive refraction, however the changes were small. [10] Qian et al., reported a positive correlation of the average RNFL thickness with refractive error in healthy children.[14] Merugacz et al., compared RNFL thickness between 30 myopic and 15 controlled participants without myopia and reported no significant difference between the two groups.[1] Vernon et al., conducted similar study on 31 highly myopic eyes of caucasian origin and observed no statistically significant correlation between the RNFL and spherical equivalent.[30] A. Rao et al., found that axial length and refractive status accounted for only 10% of the variation in RNFL thickness.[11] In our study significant correlation was established between refractive error and global RNFL thickness, which showed regression coefficient to be 3.77. There was increase in mean RNFL thickness by 3.77 microns for every unit diopter increase in refractive error.
The relationship between RNFL with axial length has been established in many studies. Sony et al., [31] and Bayratkar et al., [32] reported no significant correlation between the RNFL average thickness and axial length, however these studies were limited by small sample size. While Huynhet et al., found significant trend toward thinner RNFL with longer axial length.[10] Knight et al., observed that axial length had a negative correlation with the mean RNFL thickness but had a positive correlation with the temporal quadrant in 63 chinese children.[21] Cheung et al., reported that longer axial length was associated with thinner RNFL in a population based study of Chinese adults.[33] A. Rao et al., in their study reported that the longer the axial length and greater the myopic shift early in life, the thinner will be the RNFL thickness.[11] In our study negative or inverse correlation is seen (R²=0.155) with regression coefficient of -4.88 which shows that for every 1 mm increase in axial length, RNFL l decreases by 4.88 microns.
The retinal nerve fiber followed a normal distribution. RNFL varied minimally with gender, RNFL thinning was associated with increasing axial length and less positive refraction. The normative data from this study could serve as reference for further studies on pediatric glaucoma or other optic nerve head pathologies using nerve imaging modalities.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest
References
- M Mrugacz, A B Lazarczyk. Optical Coherence Tomography Measurement of the Retinal Nerve Fiber Layer in Normal and Juvenile Glaucomatous Eyes. Ophthalmologica 2005. [Google Scholar]
- E Larsson, U Eriksson, A Alm. Retinal nerve fibre layer thickness in full-term children assessed with Heidelberg retinal tomography and optical coherence tomography: normal values and interocular asymmetry. Acta Ophthalmologica 2011. [Google Scholar]
- L Jeanjean, G Castelnovo, B Carlander. Retinal atrophy using optical coherence tomographya (OCT) in 15 patients with multiple sclerosis and comparison with healthy subjects. Rev Neurol 2008. [Google Scholar]
- C Lamirel, N Newman, V Biousse. The use of OCT in neurology. Rev Neurol Dis 2009. [Google Scholar]
- R A Avery, G T Liu, M J Fisher, G E Quinn, J B Belasco, P C Phillips. Retinal Nerve Fiber Layer Thickness in Children With Optic Pathway Gliomas. Am J Ophthalmol 2011. [Google Scholar]
- P Kemenyova, P Turcani, S Sutovsky, I Waczulikova. Optical coherence tomography and its use in optical neuritis and multiple sclerosis. Bratislava Med J 2014. [Google Scholar]
- M A El-Dairi. Optical Coherence Tomography in the Eyes of Normal Children. Arch Ophthalmol 2009. [Google Scholar]
- D B Hess, S G Asrani, M G Bhide, L B Enyedi, S S Stinnett, S F Freedman. Macular and retinal nerve fiber layer analysis of normal and glaucomatous eyes in children using optical coherence tomography. Am J Ophthalmol 2005. [Google Scholar]
- M Mrugacz, A B Lazarczyk. Optical Coherence Tomography Measurement of the Retinal Nerve Fiber Layer in Normal and Juvenile Glaucomatous Eyes. Ophthalmologica 2005. [Google Scholar]
- S C Huynh, X YWang, E Rochtchina, P Mitchell. Distribution of Macular Thickness by Optical Coherence Tomography: Findings from a Population-Based Study of 6-Year-Old Children. Invest Ophthalmol Vis Sci 2006. [Google Scholar]
- A Rao, B Sahoo, M Kumar, Gl Varshney, R Kumar. Retinal Nerve Fiber Layer Thickness in Children <18 Years by Spectral-domain Optical Coherence Tomography. Semin Ophthalmol 2013. [Google Scholar]
- S C Huynh, X Y Wang, E Rochtchina, P Mitchell. Peripapillary Retinal Nerve Fiber Layer Thickness in a Population of 6-Year-Old ChildrenFindings by Optical Coherence Tomography. Ophthalmology 2006. [Google Scholar]
- D J Salchow, Y S Oleynikov, M F Chiang, S E K Salchow, K Langton, J C Tsai. Retinal Nerve Fiber Layer Thickness in Normal Children Measured with Optical Coherence Tomography. Ophthalmology 2006. [Google Scholar]
- J Qian, W Wang, X Zhang. Optical coherence tomography measurements of retinal nerve fiber layer thickness in chinese children and teenagers. J Glaucoma 2011. [Google Scholar]
- C K Leung, C Y Cheung, R N Weinreb. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a variability and diagnostic performance study. Ophthalmology 2009. [Google Scholar]
- H C Ahn, H W Son, J S Kim, J H Lee. Quantitative analysis of retinal nerve fiber layer thickness of normal children and adolescents. Korean J Ophthalmol 2005. [Google Scholar]
- R R A Bourne, F A Medeiros, C Bowd, K Jahanbakhsh, L M Zangwill, R N Weinreb. Comparability of Retinal Nerve Fiber Layer Thickness Measurements of Optical Coherence Tomography Instruments. Invest Ophthalmol Vis Sci 2005. [Google Scholar]
- N Elía, V Pueyo, I Altemir, D Oros, L E Pablo. Normal reference ranges of optical coherence tomography parameters in childhood. Br J Ophthalmol 2012. [Google Scholar]
- J B Barrio, S Noval, M Galdós, M R Canela, E Bonet, M Capote. Multicenter Spanish study of spectral-domain optical coherence tomography in normal children. Acta Ophthalmologica 2013. [Google Scholar]
- C A Haddad, A Barikian, M Jaroudi, V Massoud, H Tamim, B Noureddin. Spectral domain optical coherence tomography in children: normative data and biometric correlations. BMC Ophthalmol 2014. [Google Scholar]
- O J Knight, C A Girkin, D L Budenz. Effect of race, age, and axial length on optic nerve head parameters and retinal nerve fiber layer thickness measured by Cirrus HD-OCT. Arch Ophthalmol 2012. [Google Scholar]
- T Alasil, K Wang, P A Keane, H Lee, N Baniasadi, J F D Boer. Analysis of Normal Retinal Nerve Fiber Layer Thickness by Age, Sex, and Race Using Spectral Domain Optical Coherence Tomography. J Glaucoma 2013. [Google Scholar]
- D L Budenz, D R Anderson, R Varma. Determinants of normal retinal nerve fiber layer thickness measured by Stratus OCT. Ophthalmology 2007. [Google Scholar]
- Rohit Varma, Sheila Bazzaz, Mei Lai. Optical Tomography–Measured Retinal Nerve Fiber Layer Thickness in Normal Latinos. Invest Ophthalmol Vis Sci 2003. [Google Scholar]
- B Alamouti. Retinal thickness decreases with age: an OCT study. Br J Ophthalmol 2003. [Google Scholar]
- F S Mikelberg, S M Drance, M Schulzer. The normal human optic nerve. Axon count and axon diameter distribution. Ophthalmology 1989. [Google Scholar]
- D Poinoosawmy, L Fontana, J X Wu, F W Fitzke, R A Hitchings. Variation of nerve fibre layer thickness measurements with age and ethnicity by scanning laser polarimetry. Br J Ophthalmol 1997. [Google Scholar]
- R S Parikh, S R Parikh, G C Sekhar, S Prabakaran, J G Babu, R Thomas. Normal Age-Related Decay of Retinal Nerve Fiber Layer Thickness. Ophthalmology 2007. [Google Scholar]
- D C Tsai, N Huang, J J Hwu. Estimating retinal nerve fiber layer thickness in normal school children with spectral-domain optical coherence tomography. Jpn J Ophthalmol 2012. [Google Scholar]
- S A Vernon, A P Rotchford, A Negi, S Ryatt, C Tattersal. Peripapillary retinal nerve fibre layer thickness in highly myopic Caucasians as measured by Stratus optical coherence tomography. Br J Ophthalmol 2008. [Google Scholar]
- P Sony, R Sihota, H K Tewari. Quantification of the retinal nerve fibre layer thickness in normal Indian eyes with optical coherence tomography. Indian J Ophthalmol 2004. [Google Scholar]
- S Bayraktar, Z Bayraktar, O F Yilmaz. Influence of Scan Radius Correction for Ocular Magnification and Relationship Between Scan Radius With Retinal Nerve Fiber Layer Thickness Measured by Optical Coherence Tomography. J Glaucoma 2001. [Google Scholar]
- C Y Cheung, D Chen, T Y Wong. Determinants of quantitative optic nerve measurements using spectral domain optical coherence tomography in a population-based sample of non-glaucomatous subjects. Invest Ophthalmol Vis Sci 2011. [Google Scholar]
How to Cite This Article
Vancouver
Ganekal S, Ganekal V. Pediatric normative Retinal nerve fiber layer thickness in south Indian population [Internet]. Indian J Clin Exp Ophthalmol. 2025 [cited 2025 Sep 04];7(1):212-217. Available from: https://doi.org/10.18231/j.ijceo.2021.044
APA
Ganekal, S., Ganekal, V. (2025). Pediatric normative Retinal nerve fiber layer thickness in south Indian population. Indian J Clin Exp Ophthalmol, 7(1), 212-217. https://doi.org/10.18231/j.ijceo.2021.044
MLA
Ganekal, Sunil, Ganekal, Varun. "Pediatric normative Retinal nerve fiber layer thickness in south Indian population." Indian J Clin Exp Ophthalmol, vol. 7, no. 1, 2025, pp. 212-217. https://doi.org/10.18231/j.ijceo.2021.044
Chicago
Ganekal, S., Ganekal, V.. "Pediatric normative Retinal nerve fiber layer thickness in south Indian population." Indian J Clin Exp Ophthalmol 7, no. 1 (2025): 212-217. https://doi.org/10.18231/j.ijceo.2021.044
