Introduction
This is a case report of a 61yrs old male patient who presented with complaints of diminution of vision in the left eye. The patient was a known diabetic and a smoker. He had a previous history of berry aneurysm for which he underwent clipping. Ocular examination revealed a peculiar tuft of capillaries that was present on the inferotemporal portion of the optic disc. There was associated macular edema. The patient was treated with intra vitreal anti-VEGFs for the macular edema. This was followed by periods of resolution and recurrence. The following is the course of the patient in the hospital with repeated recurrences of macular edema following treatment with anti-VEGF injection.
Table 1
Figure 1
Fundus photo of the left eye of the patient demonstrating a normal sized disc, normal colour with a normal cup/disc ratio with a tuft of capillaries along the inferotemporal border of the disc
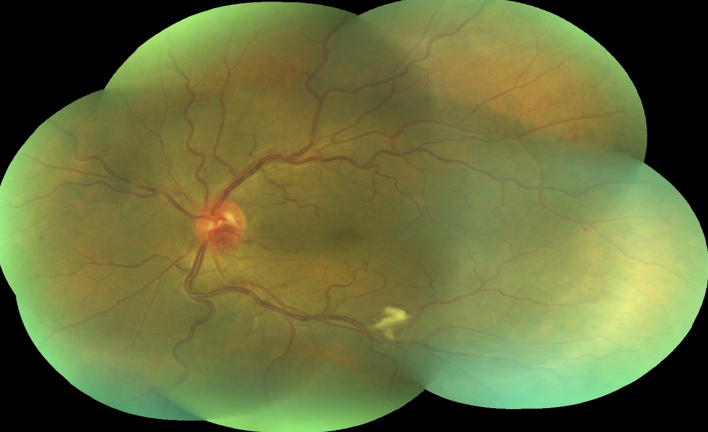
The fundus photo of the left eye showed essels over disc appear which appeared tortuous and dilated, with a A:V ratio 2:4. Cotton wool spots are seen in the inferotemporal arcade. Macula had a dull foveal reflex.
Course in the hospital
Over the next 12 months the patient underwent 4 more courses of intravitreal ranibizumab and 1 intravitreal dexamethasone. The patient’s blood pressure was monitored routinely and also recorded before every procedure and was found to be normal. The highest reading recorded was 140/90mmHg. The patient eventually underwent phacoemulsification+intraocular lens in the LE for cataract.
Course in the hospital
Over the next 12 months the patient underwent 4 more courses of intravitreal ranibizumab and 1 intravitreal dexamethasone.
The patient also underwent phacoemulsification+intraocular lens in the LE for cataract.
Differential diagnosis
A-V malformation: The patient has a history of berry aneurysmal clipping many years ago, which could mean he is prone to A-V malformations due to poor vessel wall strength. In essence an A-V malformation is an abnormal communication between an artery and a vein without an intervening capillary wall predisposing it to a turbulent state and aneurysm formation.
Impending CRVO: Dilated tortuous veins with CME is suggestive of an impending CRVO. Also known as non-ischemic CRVO-the most common type of CRVO. Fundus photography usually reveals dilated tortuous blood vessels, flame and splinter shaped hemorrhages and optic disc edema.1
Wyburn mason syndrome: Rare congenital disorder affecting the blood vessels. Markedly dilated and tortuous vessels, shunt blood flow from arteries to veins which usually do not leak fluid. Additionally might present with proptosis and nerve palsies.2 This is a congenital neurocutaneous disorder affecting leading to areterio venous malformations. Often diagnosed during infancy, they are associated with phakomatoses and present with tumors in the mid brain and spinal cord. There is no known inheritance pattern or gender predilection. They present with multiple arteriovenous malformations in the brain, orbit, retina and skin. Orbital malformations are quite frequent. These AV malformations are abnormal communications between an artery and a vein leading to turbulent blood flow predisposing it to thrombosis and ischemia. They also have an abnormal histological anatomy with an abnormally thick muscular wall. Orbital manifestations are frequently unilateral and have varying presentations with visual field defects, choroidal infarctions, vascular occlusions, optic disc edema or optic disc atrophy. AVMs presenting in the retina can predispose to vein occlusions, neovascularization and glaucoma. Rhegmatogenous retinal detachment is a rare complication. There have been reported cases of macular edema associated with retinal AVMs. The pathology is thought to be a high turbulent flow in the venous system in the absence of a capillary network, causing a back pressure on the vessel walls which causes them to leak AVMs present in the midbrain region are predisposed to aneurysm formation due to the high flow rate. Presence in the occipital region can cause visual field defects and transient vision loss. Severity and characteristics of AVMs were divided into three groups by Archer et al.3
Group 1: Defined as a retinal arteriovenous malformation containing a major artery and vein with an abnormal capillary plexus in between. These lesions typically remain asymptomatic.Group 2: Defined as a retinal arteriovenous malformation between an artery and a vein without any capillary network in between. These have a risk of retinal complications.Group 3: Defined as complex and extensive AVM’s with large vessels without a capillary plexus in between. These have a high risk for retinal complications and more likely to have intracranial malformations.
If we were to classify this patient, owing to the recurring macular edema in this patient, we could justifiably classify this patient in group 2 of Archer’s classification.
Other Ocular Signs and Symptoms Include
Proptosis, abnormally dilated vessels on the ocular surface, nerve palsies, strabismus, decreased visual acuity, vitreous hemorrhages, retinal vein occlusion, neovascularization leading to glaucoma, optic disc edema and atrophy. The patient can present with features of increased intracranial tension such as neck rigidity, headache, vomiting, seizures. Fluorescein angiography, MRI and cerebral angiography are essential for the diagnosis.
Diabetic retinopathy: The vascular structure could be a neovascularization due to the diabetic status of the patient. However this is unlikely as the fellow eye did not show any changes suggestive of diabetic retinopahty
Splinter hemorrhage of the disc vessel. Usually associated with hypertensive retinopathy. Splinter hemorrhages are suggestive of vessel wall weakness and leakage. This is unlikely however as the patient was not a known hypertensive and the hemorrhage would have resolved in weeks and not be persistent and associated with macular edema.
Conclusion
MRI and MRV had no abnormality, ruling out the possibility of an associated intracranial vascular malformation. Fundus fluorescein angiography was requested. The patient refused for the same. Glaucoma work up was done for the patient. OCT demonstrated normal RNFL thickness and Ganglion cell count, making glaucoma an unlikely pathology. Neovascularization of the disc due to diabetic retinopathy is unlikely as the fundus of the other eye had no retinopathy changes. Wyburn mason syndrome is unlikely as the patient has no other systemic abnormalities. Patients of this syndrome are also likely to be diagnosed of the same during their infancy or childhood.2 No history of skin lesions, neurological manifestations or any other characteristic ocular abnormalities such as proptosis, blepharoptosis or cranial nerve palsies. This patient has to be treated symptomatically. Owing to the wide range of presentations in AV malformations, there is no particular treatment protocol and each patient’s treatment must be individually tailored according to their symptoms. This patient must be monitored regularly with serial OCT images to make sure the normal foveal contour is maintained and any recurrences with macular edema should be treated appropriately with anti-VEGF injections or intravitreal steroids. The patient maintained good vision with this protocol and having already treated the patient’s cataract in the left eye, this would be the best course of treatment.
Taking into account the history of Berry anuerysm AV malformation of the optic disc seems to be likely diagnosis.






