Introduction
One of the most common cause of decrease of vision in a pseudophakic patient is the formation of Posterior Capsular opacification (PCO) which is affected by several factors like the design of the implanted intraocular lens (IOL) and material of the IOL.1, 2, 3 PCO incidence has been reported to be 20.7% at 2 years & 28.5% at 5 years.4 Decrease of vision because of PCO necessitates a posterior capsulotomy with neodymium yttrium aluminum garnet (Nd-YAG) laser to create a small opening in the developed opacification. It is a commonly performed relatively safe procedure associated with rare complications like increased intraocular pressure, iritis, IOL pitting, macular edema, retinal haemorrhage, retinal detachment and endophthalmitis. Here in documenting a case of IOL decentration occurring as an acute complication post YAG-laser capsulotomy. YAG Capsulotomy leading to decrease of the visual acuity of the patient due to IOL decentration has been rarely documented in literature as a complications.
IOL decentration is calculated as the distance between the IOL centre and the reference axis (the reference axis being the pupillary axis or the visual axis).5, 6, 7 Decentration of 0.2–0.3 mm is common and clinically unnoticed for any design of IOL, larger extent decentration has a negative impact on the optical performance of the IOL and subsequently, the patients’ vision and satisfaction.8
Case Report
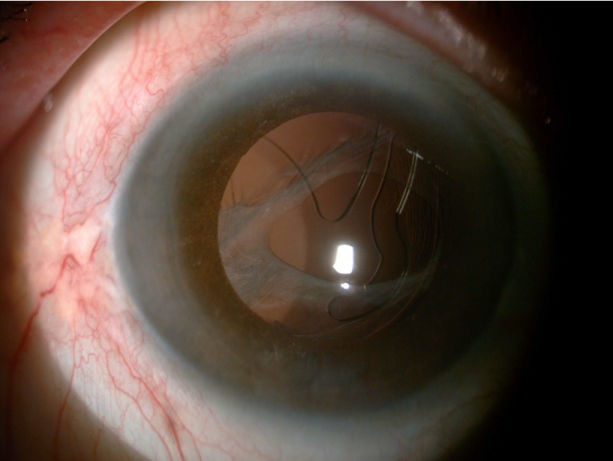
A 66-year old pseudophakic patient presented in OPD with complaint of decrease of vision in her right eye for two months. Her BCVA right eye was 6/12 and left eye 6/6, anterior segment was normal with presence of a foldable IOL with posterior capsular opacification in right eye. Fundus was completely normal both eyes. She was explained the need for YAG-laser capsulotomy which she underwent same day. Eye drops were prescribed and she was asked to review after one week. She presented one week later with complaint of complete loss of vision in her same eye for last two days. Knowing the complications of YAG-laser with a probability of retinal detachment (RD) in mind she was examined but to a surprise her IOL had undergone decentration, optic had moved out of centre and haptic had come in the central position causing her vision to decrease to CF counting finger at 2meter.
Discussion
YAG-laser capsulotomy is a common procedure done routinely by all ophthalmologists in their practices. Well known complications like IOL pitting, macular oedema and RD all are aware of. In this patient a rare complication i.e IOL decentration happened five days after the procedure (highlighting that capsulotomy was done using minimal energy, was small in size, and the ophthalmologist has been doing Capsulotomies for the last many years). Reporting this since IOL decentration has not been mentioned in most of the reports of Yag Cap complications available in literature and most of the ophthalmologists might not be aware of such a surprise post YAG-laser capsulotomy. Even in a paper by Derek O’Boyle which is a large literature review of 19 studies of Yag related complications none of the 19 studies have IOL decentration as an occurrence.9
Conclusion
YAG-laser capsulotomy is an out-patient procedure done by all ophthalmologists for posterior capsular opacification. It is known to be associated with complications like macular edema, IOL pitting and retinal detachment. IOL decentration is a rare complication post YAG-laser capsulotomy and should be kept in mind specially in eyes with foldable IOL’s.