Introduction
Psoriasis is a non-infectious, chronic inflammatory disease of the skin, triggered by the activation of immune system. The course of the disease can be altered by environmental factors and relapses are common. It is a commonly encountered inflammatory disorder with an estimated global prevalence ranging from 0.5% to 4.6%.1 The estimated prevalence in India is 0.7%.2 The immunopathology of psoriasis is characterized by T-cell activation and increased cytokine activity, in which tumour necrosis factor-a plays an important role. The classical lesions are well demarcated plaques, with an erythematous base and silvery scales on its surface. It is seen mainly over the extensor surfaces and scalp. The percentage of body affected by psoriatic plaques can vary. It can be graded as mild (<2%), moderate (2–10%), and severe (>10%) psoriasis. The most common type of psoriasis is chronic plaque psoriasis or psoriasis vulgaris. However, it can also be classified into 4 different types such as guttate, pustular, erythrodermic, and inverse psoriasis.3
Psoriasis has been associated with various comorbidities, such as inflammatory bowel disease, arthritis, psychiatric disorders, cardiovascular disease, stroke, diabetes mellitus and renal diseases. Ophthalmic complications of psoriasis are numerous and affect almost all parts of eye. Prevalence of ocular psoriasis is reported to be 67%, with blepharoconjunctivitis being the commonest manifestation.4 Ocular involvement in psoriasis predominantly occurs during exacerbation of systemic disease.5
An ocular inflammatory reaction involving the conjunctiva, sclera, cornea, uvea and lens is common in patients with psoriasis. Of these, uveitis is a serious and sight threatening complication. Psoriasis may affect the eye due to direct involvement by the disease or by immune mediated mechanism. The treatment modalities such as retinoids and psoralen and ultraviolet A (PUVA) therapy can also affect the eye. The various findings range from blepharitis, conjunctivitis, dry eye, episcleritis, marginal keratitis and uveitis. Signs and symptoms may be subtle and overlooked,6 but a thorough understanding of ophthalmic involvement is important for comprehensive care of patients with psoriasis as many times it is diagnosed only after irreversible damage has occurred in the ocular tissue. The delay in presentation maybe due to lack of awareness, fewer symptoms or deferred referrals. The aim of this study was to identify the prevalence and to analyse the various ocular abnormalities and their association with the type of psoriasis. Visual morbidity due to ocular complications during both presentation and following psoriasis treatment are to be determined in our cohort of patients. We also assessed primary symptoms and ocular complications that can occur following the treatment of psoriasis such as steroid induced cataract, steroid induced glaucoma, recurrence or reactivation of infection.
Materials and Methods
A prospective observational study among psoriasis patients was conducted in the ophthalmology department at Sri Ramachandra Institute of Higher Education and Research. This was performed in concurrence with the department of dermatology after ethics committee approval was obtained (CSP-MED/18/OCT/47/171). A detailed history was recorded regarding their systemic symptoms, ocular complaints, duration of psoriasis and treatment history after getting an informed consent from each patient. All participants underwent complete ocular examination including visual acuity using Snellen's chart, anterior segment examination using slit-lamp biomicroscope, intraocular pressure (IOP) measurement using applanation tonometry and posterior segment examination with +78D lens/direct /indirect ophthalmoscope.
Tear film height assessment, tear break -up time, Schirmer’s test and corneal and conjunctival staining with Rose Bengal stain was done for all study subjects as diagnostic tests of dry eye. Conjunctival and corneal staining methods provide an objective measurement of the extent of ocular surface damage caused by dry eye. In our study this was done using Van Bijsterveld scoring system. In this system the cornea is divided into 3 zones (grading areas) and it is enumerated to determine the total score. As part of ocular surface evaluation, history of other risk factors such as rheumatoid arthritis, diabetes mellitus, contact lens use, smoking and thyroid eye disease was recorded.
We followed up the patients every month as routine and more frequently if required. Patients with ocular complaints and dermatological features of psoriasis were sent to dermatology department for confirmation of diagnosis, and treatment of systemic disease. All established psoriasis patients and those with ophthalmic and dermatological features suggestive of psoriasis with a confirmed clinical diagnosis were included in the study. Patients with other inflammatory connective tissue disease, rheumatological disease or other autoimmune disease with skin lesions were excluded from the study.
Statistical analysis
The data were collected and analysed using ibm spss statistics software, version 23.0. Descriptive statistics frequency analysis for data distribution, percentage analysis for categorical variables and the mean & standard deviation for continuous variables were used. Tests were correlated and between test values were calculated using kappa coefficient. Chi-square test was used to find the significance in categorical data. A probability value of p< 0 .05 was considered as statistically significant.
Results
An observational, prospective cohort study on 240 eyes of 120 patients with psoriasis was performed. In our study, of 120 patients with psoriasis, total number with ocular manifestation was 68 patients (57%). The distribution was seen as 67% of males and 53% of females. Majority of the patients with ocular involvement were found to be within the age group of 41-60 years (median age of 50 years). Bilateral involvement was seen in 91% of patients which was statistically significant with p=0.01.
The most common type of psoriasis in the study group was psoriasis vulgaris (59 patients out of 120 patients). However, although the prevalence of psoriasis vulgaris was higher, ocular involvement was found to be more common in patients with pustular and guttate psoriasis (100%) followed by erythrodermic psoriasis (80%). We observed that ocular findings were more common in patients with scalp psoriasis with 62% prevalence. 61% of patients with ocular manifestation had psoriasis for a duration of less than 5years only.
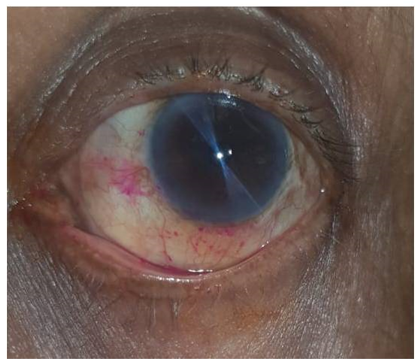
The prevalence of ocular manifestation in psoriasis was 57%, of which 22% of the patients were symptomatic, with irritation of eyes being the commonest symptom, followed by watering. The various ophthalmic features among psoriasis patients were ocular surface disorder in 46%, cataract in 30%, meibomitis in 17%, blepharitis in 16%, conjunctival congestion in 16% and non-specific superficial punctate erosions in 9%. Keratoconjunctivitis sicca (dry eye) was the most common.
Objective tests for evaluation of the tear film done showed that 8% had abnormal Schirmers test I indicating reduced aqueous secretion, 63% had a positive score on Van Bijsterveld grading system which was greater than 6 in 72% of patients. 96% had reduced tear break up time indicating tear film instability. Correlation between tests was calculated using kappa coefficient and statistical significance was found in the pattern of conjunctival staining with a p value of 0.02.
The prevalence of blepharitis was 16%, associated meibomitis was seen in 17%, non-specific conjunctival congestion in 16%, associated conjunctival keratinisation in 13%, superficial punctate erosion in 9% and tylosis in 5%. None of the patients had peripheral corneal melting.
The mean intraocular pressures of our study subjects were predominantly in the normal range. 26 patients of the total 120 with psoriasis had borderline to high intraocular pressures ranging from 21-30 mmHg. Fundus examination in these patients showed cup disc ratio of 0.4-0.5 with a normal neuroretinal rim in 78% of patients. Gonioscopy showed open angle with visualisation up to the scleral spur in 66% of patients. The use of topical corticosteroids was noted in the majority of these patients. In those with high IOP, the relationship between the IOP, cup to disc ratios, central corneal thickness and neuroretinal rim thinning was studied. Steroid induced glaucoma in 79% and ocular hypertension in 21% was identified. Perimetry in these patients showed nasal step and arcuate scotoma in 3% of patients.
Even though 9 patients in our study group had psoriatic arthritis, none of them had active uveitis during the time of screening. 3% of patients showed old keratic precipitates and posterior synecheae.
Cataract was observed in 60% of psoriasis patients receiving oral steroids. Among them 15 patients of were less than 40 years. Majority of the patients were on treatment with topical steroids, followed by a combined treatment with methotrexate and topical steroids. In patients who received ciclosporin, 80% had ocular manifestation, with dry eye being the most common finding.
Table 1
Distribution of ocular manifestations in psoriasis
|
Ocular manifestation |
No. of patients |
Percentage |
|
Dry eye |
35 |
46% |
|
Cataract |
25 |
30% |
|
Glaucoma |
22 |
27% |
|
Meibomitis |
14 |
17% |
|
Blepharitis |
13 |
16% |
|
Conjunctival congestion |
11 |
10% |
Table 2
Ocular manifestation in different types of psoriasis
Table 3
Dry eye evaluation-Schirmer’s test
|
Schimers Test |
>15mm |
5-15mm |
<5mm |
|
Re |
98 |
14 |
8 |
|
Le |
99 |
10 |
11 |
|
Total |
197 (82%) |
24 (10%) |
19 (8%) |
Discussion
Psoriasis is a multisystem inflammatory disease with predominantly skin and joint involvement. Out of the 120 patients, we found that ocular manifestation occurred in 67% of the males and 53% of the female patients. Majority of patients with ocular involvement were found to be in the 5th decade of life. Patients with longer duration had been on treatment with corticosteroids thus altering inflammation but had ocular features of complications to steroid use such as cataract and glaucoma.
The most common type of dermatological presentation is psoriasis vulgaris, but we found that ocular manifestation was 100% in pustular and guttate psoriasis, 80% in erythrodermic psoriasis, 60% in palmoplantar and only 54% in psoriasis vulgaris. Patients with scalp psoriasis had 62% prevalence.
Previous studies done by Chandran et al.7 and Erbagci et al. had reported the prevalence to be 67% and 65% respectively. In our study group, only 22% of the patients were symptomatic, with irritation of eyes being the commonest symptom, followed by watering. Among ocular manifestation the most common ocular feature was ocular surface disorder followed by cataract, glaucoma meibomitis, blepharitis, and superficial punctate erosions.
Dry eye tests were done to look for aqueous secretion, tear film stability, mucus plaques/filaments by Schirmers test me, tear break up time and Rose Bengal staining. We found that 8% had abnormal Schirmers test I of less than 5mm indicating reduced aqueous secretion and 96% had reduced tear break up time. Van Bijsterveld score was positive in 63% and was predominant with scores greater than 6 in 72% of patients with conjunctival involvement more common than cornea.
The presence of a normal Schirmer’s test in the presence of an abnormal tear break up time was seen in a large number of our patients. Conjunctival staining with Rose Bengal was significant and was more common in the central and inferior zones than superior due to evaporative dry eye.
This probably suggests that the tear film secretion is normal or near normal but the dry eye state is because of tear film instability and a chronic diseased ocular surface. The glandular component, predominantly the goblet cells may be deficient which can cause the grittiness and discomfort in these patients. Corneal involvement in the form of superficial punctate erosions due to de-epithelialisation which can occur in keratoconjunctivitis sicca.
Our results were similar to a study done by Lima et al,8 who reported abnormal Schirmer’s test and reduced tear break up time in psoriasis patients, while Kilic et al.9 on comparing with control group, found that Schirmers test and tear break up time values were statistically lower in psoriasis patient group.
In our study, the prevalence of squamous blepharitis was found to be 16% and was associated with meibomitis and tylosis in the majority. Secondary changes in the lipid component of the tear film resulted in increased evaporation and worsening of ocular surface disease. The cause for blepharitis and meibomitis in our patients was probably due to increased epithelial turnover which is a part of the systemic autoimmune disease process. Blepharitis was controlled with lid hygiene, warm compression, lid scrubs, lubricant eye drops and antibiotic ointment. All patients responded to this treatment and inflammation cleared within 1 week. Conjunctival congestion with associated conjunctival keratinisation and superficial punctate erosion were complications of severe dry eye due to micro-trauma in the cornea. None of our patients had peripheral corneal melting.
An association between joints and eye in psoriasis has also been established in many studies. Contrary to previous literature, in our study we did not see any correlation between psoriatic arthritis and active uveitis. All these patients were on anti-inflammatory medication for psoriatic arthritis which could have suppressed inflammation in the eye.
The prevalence of anterior uveitis in patients with psoriatic arthritis was reported to be 25% and 7% in a previous study by Wollina et al.,10 and Villani et al.11 Also a large nationwide Danish study showed that patients with psoriatic skin disease, even in the absence of psoriatic arthritis, are at increased risk for uveitis.12 Using a flare-cell meter, Okamoto and Umebayasi13 showed a significantly higher aqueous flare level in psoriasis patients without ocular features than in controls. He suggested that a blood aqueous barrier breakdown may occur as a result of subclinical inflammation in psoriasis patients and had a positive correlation with both the severity of psoriasis and age of the patient.
Cataract has been reported to be a common cause of visual impairment in patients with psoriasis.14 We found that majority of patients receiving topical steroids had cataract and this could be because of senile or more frequently corticosteroid induced cataractous changes.
In our cohort, the mean intraocular pressures of our study subjects were in the normal range. 22% of patients had borderline high IOP (21-30 mmHg) due to steroid induced glaucoma. All patients were treated with brimonidine or timolol eye drops.
Majority of the patients were on treatment with topical steroids, followed by a combined treatment with methotrexate and topical steroids. In patients who received ciclosporin, 80% had ocular manifestation, with dry eye being most common finding.
Ocular signs and symptoms in psoriasis may be subtle and overlooked, hence all patients should undergo complete ophthalmic examination for early detection of ocular abnormalities, ocular complication following treatment of psoriasis and for early initiation of treatment. We found that even though only 22% of the patients had ocular symptoms, 57% had ocular manifestations with ocular surface disorder being the predominant finding.
Though literature states that patients with psoriatic arthritis develop ocular involvement we observed in our study that they may be seen in patients without an arthritic component as well. Hence all patients should be screened for ocular manifestation irrespective of the presence of joint involvement.
Dry eye is due to evaporative type and an unstable tear film can aggravate it. Chronic keratoconjunctivitis sicca can predispose to allergic conjunctivitis and meibomitis, which can result in abnormality of lipid component of tear film. Patients must be evaluated and treated for dry eye in the early stages as irreversible ocular surface changes may lead to persistent ocular discomfort.
Psoriasis patient needs to be monitored regularly as ocular complications such as steroid induced cataract and steroid induced glaucoma can occur following the treatment of psoriasis. As multisystem involvement is seen in psoriasis, a combined treatment approach involving screening and early treatment is required to reduce the ocular morbidity of the patient and for complete patient care.