Introduction
Opacification of crystalline lens is referred as cataract, which can be congenital, infantile, juvenile, pre-senile and senile. Childhood cataract is one of the leading causes of treatable blindness. It accounts for 7.4%–15.3% of paediatric blindness and significant avertable disability adjusted life years.1, 2 One of the priority diseases within the disease-control strategy of VISION 2020 initiative is childhood blindness.3 Incidence of childhood cataract ranges from 1.8 to 3.6 /10,000 per year with a median prevalence of about 1.03/10,000 children(0.32-22.9/10,000). Low income economies have a higher prevalence (0.63-13.6/10,000) of childhood cataract as compared to high income economies (0.42-2.05/10,000), laterality and gender based prevalence has no difference.4 The diagnosis of cataract is incidentally made on routine screening in 41% of cases whereas leukocoria and strabismus led to diagnosis in 24% and 19%, respectively.5 Childhood blindness can be reduced and quality of life can be changed by operating on these cases as early as possible.
In today’s developed world half of approximately all childhood cataracts are of unknown etiology. The rest are due to hereditary disease, metabolic disease, or associated with other ocular or systemic disorders.6 Trauma, radiation, drug induced and laser therapy induced in ROP are other causes of childhood cataract in older children. Most common cause of unilateral cataract in the developing countries is trauma.7, 8 Common cause of bilateral cataract is long term use of systemic steroid. Approximately 50% of all bilateral cataracts and virtually all unilateral cataracts underlying cause is unidentified.9, 10 Genetically inherited cataracts are main contributory factors in etiology of childhood cataracts among which half have mutation in crystallins and quarter have mutation in connexins.11 Attempts to present evidence based information in order to improve childhood eye care facilities in India have been made.7, 12, 13, 14, 15, 16, 17
Choithram Netralaya and Research Center provide community eye care services to West Central population of India. Free eye care services and eye screening camps have contributedto improve pediatric eye care by early detection, counseling and early surgery of childhood cataract. All the surgeries performed are free of cost, under Rashtriya Baal Swasthya Karyakram(RBSK) scheme which started in our institute in 2018. We studied childhood cataract and visual outcome following surgery as an objective of our study to provide evidence based information regarding pediatric cataract in West Central India.
Materials and Methods
Retrospective analysis of records was done, of patients of age 5months to 17 years who were operated for childhood cataract at Choithram Netralaya and Research Center from June 2018 to April 2020. Screening of more than 13000 patients was done by trained community optometrist at outreach camps and patients with significant cataract were referred to institute for further evaluation and cataract surgery.
Analysis of medical records was done, data was collected and recorded in Microsoft Excel Sheet (Version 6.0, Microsoft USA). Recorded data included demographic data, parental information including, medical history, marriage history regarding consanguinity, birth history including birth weight, prematurity, vaccination history, parental medical history and patients past history was recorded. Visual acuity was recorded with the help of Snellen’s Chart and Tellers Acuity cards. Detailed anterior segment evaluation was done by our experienced Pediatric surgeon under full pupillary dilatation, anterior chamber details, corneal diameter, type of cataract whether congenital, developmental, traumatic or complicated, IOP was recorded with the help of Perkins Hand held Applanation Tonometer. For those patients in whom examination was not possible examination was done under short general anesthesia. Keratomerty, axial length and IOL power was calculated with the help of IOL Master (Zeiss, Germany). Posterior segment evaluation was done using indirect ophthalmoscopy and if media opacity obstructing the view then B-scan was done. Routine blood and urine analysis was done including complete blood count, random blood sugar analysis, routine urine analysis, HIV, HBsAg following which pre anesthetic check up was done and fitness was taken for each and every case.
Standard surgical technique phacoemulsification, posterior capsulorhexis, anterior vitrectomy and primary IOL implantation was done in all patients. All the surgeries were performed single handedly by highly experienced pediatric ophthalmology surgeon and Vitreo-Retinal backup was called for if required. Intra-operative complications were noted. Post-operative evaluation was done at post-operative day 1, 1 week, 1month and 6 months (if possible) which included visual acuity assessment, visual axis clarity, amblyopia (if present standard patching protocol was followed), refractive status and any post-operative complications.
Statistical analysis was done using parametric method of univariate analysis. Percentage, proportions, frequency was analyzed for important parameters using Microsoft Excel Sheet (Version 6.0, Microsoft USA).
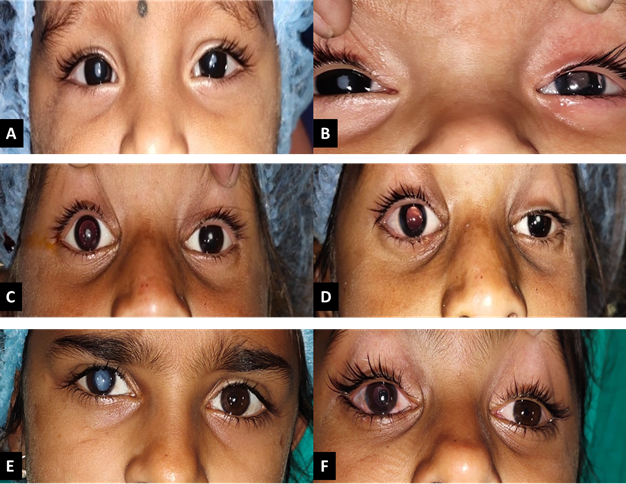
Figure 1
Pre and post operative photos; A: Pre-operative Figure of a 11 month old Female child showing Bilateral Congenital Cataract, B: Post-operative Figure of a 11 month old Female child showing OD Congenital cataract, OS Pseudophakia with clear Fundal Glow, C: Pre-operative Figure of a 8 years old Female child showing Bilateral Developmental Cataract, D: Post-operative Figure of a 8 years old Female child showing OD Pseudophakia with clear Fundal Glow, OS Developmental Cataract, E: Pre-operative Figure of a 12 years old Female child showing OD Traumatic Cataract, OS Clear lens, F: Post-operative Figure of a 12 years old Female child showing OD Pseudophakia with clear Fundal glow, OS Clear lens.
Results
Table 1
Showing gender and age wise distribution of data
Table 2
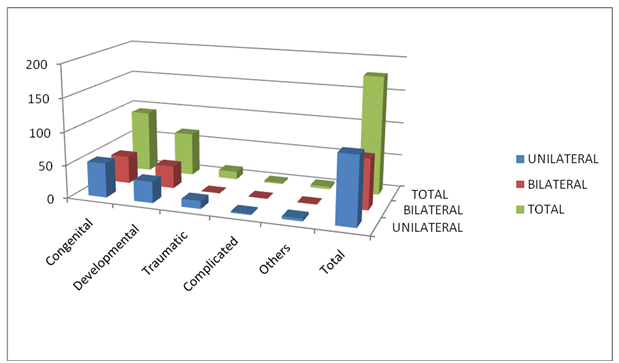
Showing distribution of unilateral and bilateral cataract amongst different type of pediatric cataract
|
Cataract Type |
Unilateral |
Bilateral |
Total |
|
Congenital |
52 |
42 |
94 |
|
Developmental |
32 |
34 |
66 |
|
Traumatic |
12 |
0 |
12 |
|
Complicated |
02 |
0 |
02 |
|
Others |
04 |
0 |
04 |
|
Total |
102 |
76 |
178 |
Table 3
Showing age wise distribution of different types of pediatric cataract.
|
Cataract type |
1 month-1 yr |
2 yrs – 6 yrs |
7 yrs – 12 yrs |
13 yrs – 18 yrs |
|
Congenital |
4 |
30 |
38 |
22 |
|
Developmental |
0 |
4 |
30 |
32 |
|
Traumatic |
0 |
0 |
12 |
0 |
|
Complicated |
0 |
0 |
0 |
2 |
|
Others |
0 |
0 |
0 |
4 |
Our study included 244 eyes of 178 pediatric patients which were operated at Choithram Netralaya from June 2018 to April 2020 under RBSK scheme. Of these 178 patients 100 were male and 78 female, mean age of patients at the time of surgery was 8.64 years (SD2.63 years), gender and age wise distribution was calculated (Table 1). Youngest operated child was 7 months old and eldest was 17 years old, a large proportion of patients 59.55% were operated between the age of 7years to 12 years, followed by 24.71% in age between 2 years to 6 years, 13.48% in age between 13 years to 18 years and 2.24% in age between1 months to 1 year.
Of these 178 patients 102 (57.30%) patients had unilateral and 76 (42.69%) patients had bilateral cataract, unilateral and bilateral frequency was calculated in different sub groups of different types of cataract. On the basis of history obtained for age of onset, trauma, systemic and ocular disease childhood cataract were divided into Congenital (52.80%), Developmental (37.07%), Traumatic (6.74%), Complicated (1.12%) and others (Membranous and Absorbed cataract of unknown etiology) (2.24%) (Table 2). Frequency and proportions of different cataract were analyzed in different age groups at the time of operation, maximum number of congenital and traumatic cataract patients 40.04% and 100% respectively belonged to age group of 7 years to 12 years, whereas developmental (48.48%), complicated(100%) and others (100%) were found to be in age group of 13 years to 18 years (Table 3).
During the detailed pre-operative evaluation we found that of 96 patients with congenital cataract 46 (48.93%) patients had nystagmus, 6 (6.25%) had microcornea, 2 (2.08%) had Marfan’s syndrome with subluxated lens, 2 (2.08%) had iris coloboma, 2 (2.08%) had aphakia in other eye and 2 (2.08%) had corneal opacity. Of 12 traumatic cataract patients 10 (83.33%) had corneal opacity. Of total 178 patients 14 (7.86%) had squint. None of the patient had persistent fetal vasculature (PFV), any pre existing posterior capsular deficiency, congenital glaucoma or any systemic or metabolic disease. None of the parents had consanguineous marriage.
Of the 244 eyes operated only 2 cases had intra-operative complication of loss of capsular bag during the surgery, following which Iris claw lens was placed in one and in other patient PCIOL was placed in sulcus along with peripheral iridectomy. One case had IOL drop in early post – operative period for which vitrectomy, IOL removal and SFIOL placement was done by Vitreo-Retinal surgeon. In 10 patients reactionary membrane formation in early post-operative period was seen which was managed by oral and topical steroids along with cycloplegics, which resolved at 1 month follow up. In 4 patients severe inflammation was present post-operatively along with reactionary hypopyon which was managed by oral and topical steroids. None of the case had infective endophthalmitis. One patient had corneal abrasion at one week follow up which was taken care with patching but it developed nebulo– macular corneal opacity afterwards.
Visual axis opacification were noted in 14 patients 6 moths post-operatively which were due to deposition of pigments and fibrin over IOL in 6 cases, posterior capsular opacification in 2 cases and corneal opacity obscuring vision in 4 cases.
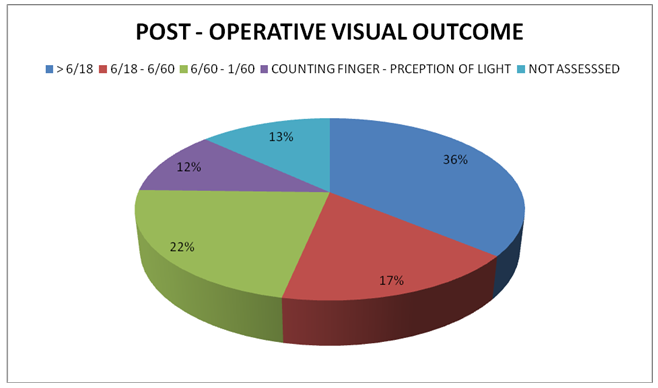
For assessment of visual outcome following surgery patients were divided into four groups. Group 1 with good visual acuity more than 6/18 having 88 patients (36.06%), group 2 with visual acuity between 6/18 – 6/60 having 42 patients (17.21%), group 3 with visual acuity between 6/60 – 1/60 having 34 patients (22.13%) and group 4 with visual acuity between counting fingers to perception of light having 28 patients (11.47%) as shown in Pie chart 1below. Due to uncooperative nature in 32 (13.11%) patients accurate vision could not be assessed. Post-operatively on fundus evaluation it revealed that one patient had Coat’s disease and 2 had myopic fundus with RPE atrophy. Amblyopia was dealt with standard patching technique after proper counseling of parents.
Discussion
One of the major treatable causes of childhood blindness is cataract. It is one of the major cause of loss of vision in pediatric age group worldwide and in developing countries, counting for 17-39% of cases as said by Moriarty et al.(1988)7 and Eckstein et al.(1995),18 however after Vision 2020 global initiative the problem has decreased quite a bit. As stated by Lloyd et al. (2007)6 this is a rare disorder, in contrast to our study where the rate of childhood cataract was pretty high, this might be due to low socioeconomic status of our study population, lack of health care facilities around them, and mainly the education status and awareness of parents, this is supported by the fact that all the patients in our study were screened in rural out-reach camp setup and then referred to our institute for further management. Improvement in management of childhood cataract is improving day by day due to continuous outreach and ongoing clinical research.
Overall male: female ratio in our study was 1.28 which relates nearly well with Abrahamsson et al. 1999 and Haargaard et al. 200419, 20 on childhood cataract including both operated and non-operated cases. This could be due to low literacy rates of the parents, a relatively less access for females to eye care services, lower socioeconomic status and higher incidence of trauma in males.
Incidence of unilateral cataract was nearly 1.5 times more than bilateral cataracts in our study which was less than observed by Khandekar R et al. 200717 in which unilateral cataract was six times more than bilateral cataracts. On contrary ratio was 1:2 in Wirth MG. et al. 200221 in Australia and bilateral cataracts were more than unilateral in a study in Denmark.22 This might be due to more number of traumatic, complicated cataracts in our study. The distribution of children operated for unilateral versus bilateral cataract was fairly equal in Magnusson, Get al.23 This is in accordance with Abrahamssonet al. 1999 and San Giovanni et al. 200219, 24 including both operated and non-operated children although Haargaard et al. 2004a25 show a predominance of bilateral cases.
Out of 94 congenital cataracts 12 had associated anomalies such as microcornea, Marfan’s Syndrome, iris coloboma and corneal opacity. None of the cataract was associated with maternal rubella syndrome, which is less as compared to Johar et al.12 and previous studies in north India and south India.7, 26 This decrease may be attributed to the fact that good antenatal care and counselling is provided and aggressive vaccination in children is done these days. In rest of the cases aetiology could not be assessed in congenital cataracts.
In our study post-operative visual acuity was more than 0.5 logMAR in around 36% cases which was less as compared to Raina et al. 16 which reported >0.5 visual acuity in 42 eyes. In Kim D Het al.2012, 27 thirty-seven paediatric bilateral pseudophakic patients were identified with a mean follow-up period of 81.4 months and best corrected visual acuity of20⁄40 or better were attained in 44.0% of eyes, and the median BCVA was20 ⁄ 50. Low visual outcome in our study can be attributed to late presentation of patients for surgery; maximum patients were presented between 7 yrs – 12 yrs among which maximum patients were having congenital cataract leading to development of amblyopia.
Most of the children needed visual rehabilitation services post cataract surgery 26 such as proper amblyopia management, low vision aids etc. Due to low rate of follow up, lost follow ups, uncooperative nature of children proper visual assessment could not be done in many patients. This can be improved by having a children friendly atmosphere in the paediatric ophthalmology departments and having trained optometrist who can properly and patiently assess the visual acuity of children by use of toys, coloured blocks acuity cards and proper counselling of parents regarding importance of follow ups.
Long term follow ups should be encouraged in parents’ by proper counseling of parents pre and post surgery on community basis in society providing them good knowledge about the severity disease and outcome after surgery. This will in turn help in assessing proper visual outcome in these patients and lead to a better visual rehabilitation.
Conclusion
Treatment of childhood cataract has evolved during the past decade but delivering the facilities to patients has been a biggest challenge to health care providers. This can be improved by delivering proper and frequent counselling to society including prevention, identification, intervention and rehabilitation. Further studies are required to identify factors leading to childhood cataract. Finally eye care providers should collaborate with different eye care programme run by government such as RBSK and AYUSHMAN Bharat in improving child health especially in rural areas where socioeconomic condition of patients overpowers the graveness of disease.