Introduction
Cysticercosis is a preventable cause of blindness caused by Cysticercus cellulosae, the larval form of pork tapeworm, Taenia solium. It is endemic in many countries including South-East Asia, India, Africa and other developing countries where the areas of poor hygiene and consumption of pork are common. Human are the intermediate host and cysticerci develop into larvae and penetrate the human intestines to reach the blood stream after ingesting contaminated raw or undercooked meat or water containing eggs. The most common locations are central nervous system (CNS), eyes, heart, muscles subcutaneous tissues.1 The clinical manifestations of cysticercosis are highly variable depending on the number of lesions, site of involvement and host immune response to the parasite. Ocular cysticercosis can be extraocular or intraocular and may show different clinical presentations which rises a clinical challenge to the ophthalmologists. We report a case of ocular cysticercosis which presented with unilateral ptosis and mild pain.
Case History
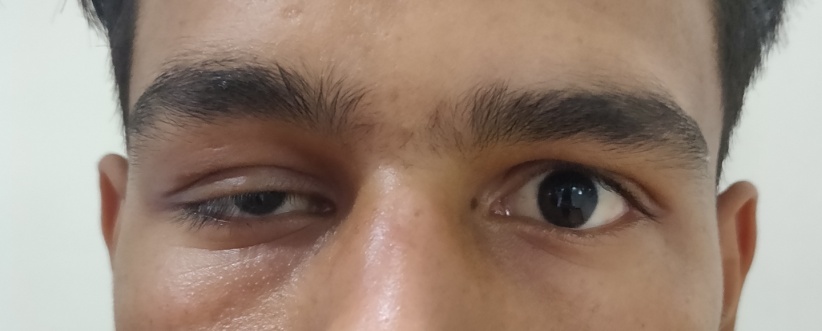
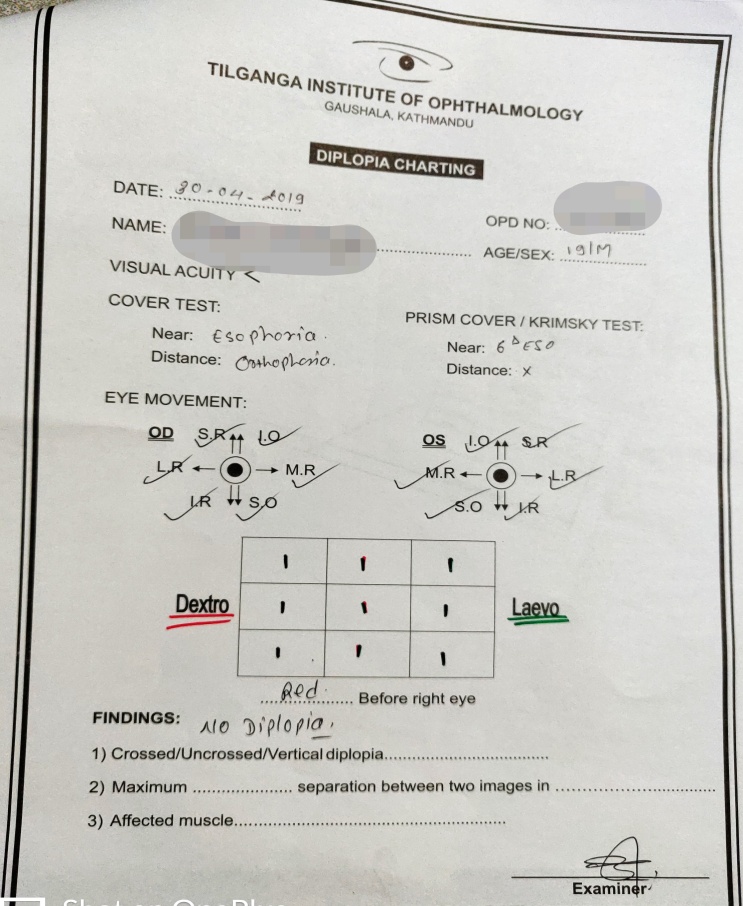
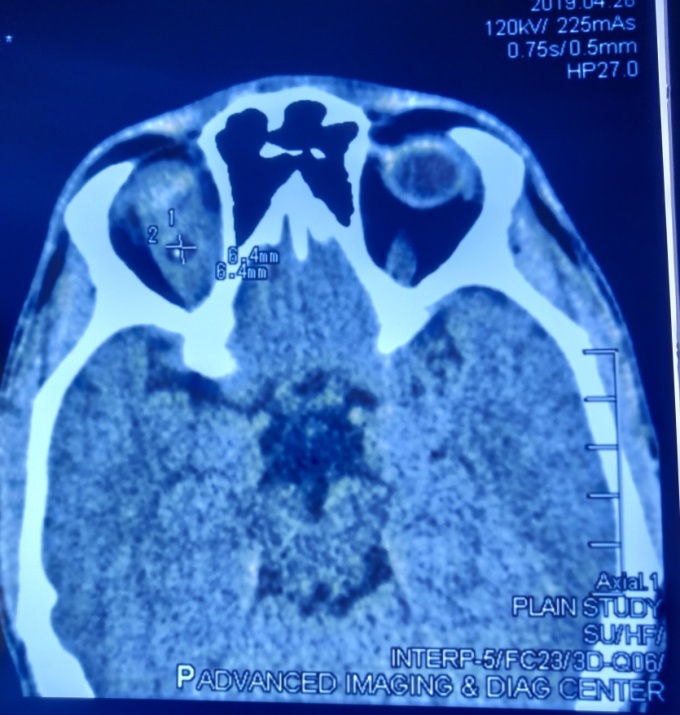
A 19 year old male patient, from Kathmandu, Nepal presented with mild swelling and drooping of right upper eyelid for 2 weeks associated with mild pain and redness on first 3 days. First, he was diagnosed as dacryoadenitis and treated with oral antibiotics and analgesics for 1 week but the swelling and ptosis were not relieved. On examination, visual acuity was 6/6 in both eyes and the ocular motility was full in all cardinal gazes. There was ptosis and mild swelling on temporal side of right upper eyelid. The swelling was soft in consistency with no tenderness. Vertical interpalpebral height (IPH) and margin reflex distance 1 (MRD1) were 6mm and -1m in right eye while in left eye, 11mm and 4mm respectively. Levator function was good (15mm) in both eyes with normal Bell’s phenomenon and intact cornea sensation. Marcus Gunn jaw winking phenomenon was absent and there was no fatigability. There was no proptosis and no any palpable mass in periocular region. The sclera and cornea were normal and there was no any congestion of conjunctiva in both eyes. Both pupils were symmetrical in size and equally reactive to both direct consensual light. Anterior segment and dilated fundus examination of both eyes showed no abnormalities. Other systemic examinations were within normal limit. The complete blood count was normal. Microscopic examination of the stool did not show any abnormal findings including Taenia parasites or eggs. The enzyme linked immunosorbent assay (ELISA) for serum antibodies against cysticercosis was negative. The diplopia chart showed no diplopia (Figure 5). The contrast enhanced computed tomography (CT) scan of head and orbit showed bulky right superior rectus muscle measuring around 15.1mm in width with a hypodense (HU:8-22) lesion measuring approximately 6.4x6.4mm in size with central puntate calcification within it (representing scolex). (Figure 2, Figure 3) After contrast administration, there was ring enhancement around the lesion. Rest of the bilateral extraocular muscles were normal. Bilateral bony orbits were symmetrical and appeared intact. Bilateral eyeballs appeared normal in size, shape and outline and there was no intraocular radiodense lesion. No intraconal or extraconal mass was seen on left side. The CT scan findings were suggestive of right eye myocysticercosis involving superior rectus muscle.
Final diagnosis was made as right eye ocular myocysticercosis. He was treated with oral prednisolone 50mg per day (1mg/kg) with tapering 10mg weekly for total 5 weeks and five days after starting prednisolone, oral albendazole 400mg two times per day (15mg/kg) was given for total 4 weeks. Follow up visits were at 2 weeks, 1 month and 3 months. At 1 month follow up, right eye vertical IPH was significantly improved to 10mm and at 3 months, vertical IPH were normal and equal in both eyes.
Figure 2
Coronal view of contrast enhance CT scan showing superior rectus muscle mass with hypodense lesion
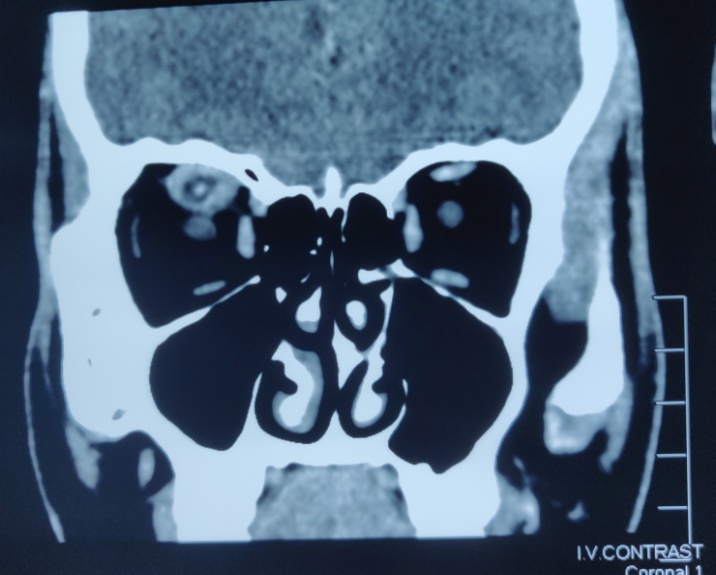
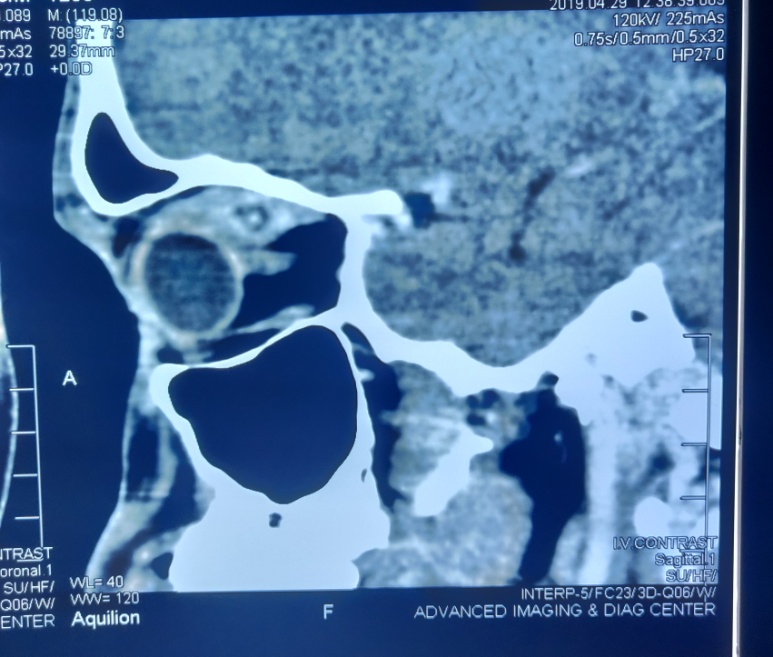
Figure 3
Axial view of contrast enhance CT scan showing the measurement of hypodense lesion (6.4x6.4mm)
Discussion
Ocular cysticercosis can involve intraocular (involving either anterior or posterior segment) or extraocular (orbital and adnexal cysticercosis). Extraocular cysticercosis showed predilection for children and young adults with no sex predilection.2 Kruger-Leite et al reported that 35% of the cysts were found in the subretinal space, 22% in the vitreous, 22% in the subconjunctival space, 5% in the anterior segment, and only 1% in the orbit.3 Unlike western countries, the ocular adnexa have been reported to be the most common site of disease in India.4, 5 When the extraocular muscles are involved, the superior rectus is the most common (33.3%).4 If the cyst is found in the subconjunctival space, it is thought to be spread from the adjacent muscles. Despite of uncommon association with orbital and systemic cysticercosis, systemic involvement especially neurocysticercosis should be ruled out.
Ocular cysticercosis can result in a number of manifestations depending on the location of the cysts. The common manifestations are periocular swelling, proptosis, ptosis, pain, diplopia, restriction of eye movement, decreased vision, lid oedema and orbital cellulitis.6 Few cases of ocular myocysticercosis presenting with ptosis similar to our case were reported in the literature.7, 8, 9
The diagnosis of orbital and adnexal cysticercosis is mainly based on radiological findings because sometimes clinical findings may be non-specific or serological tests may show false positive.6 Sahu et al. reported that 32.5% and 45% cases were positive for ELISA using larval somatic and excretory (ES) antigens respectively. Antibodies of the latter one were found more frequently in cases of extraocular cyst than intraocular cases and may be more useful in post treatment follow ups.10 Stool examination is usually done only in suspected cases of cysticercosis.
Once the diagnosis is confirmed, oral albendazole (15mg/kg) body weight per day for 4 weeks and oral steroid (prednisolone 1mg/kg) body weight tapered over 4 to 6 weeks is the standard treatment for extraocular cysticercosis. 4 Rath et al. reported that clinical resolution was achieved in 92.8% of patients at 1 month and in 95.3% of patients at 3 months by implying this standard medical management.4 Therefore, medical therapy alone is recommended for extraocular muscle form and retro-orbital form and surgical removal is needed for subconjunctival and eyelid cysticercosis.11