- Visibility 111 Views
- Downloads 15 Downloads
- DOI 10.18231/j.ijceo.2020.052
-
CrossMark
- Citation
Outcome of double headed pterygium surgeries with conjunctival autograft adhered by autologous blood: a retrospective study
- Author Details:
-
Sharda Punjabi *
-
Nishant Patel
-
Komal Bhutna
Introduction
The term ‘pterygium’ is derived from a Greek word ‘Pterygos’ meaning ‘wing’.[1] It is a non-malignant, slow growing, wing shaped proliferation of the fibrovascular tissue, arising from the subconjunctival tissue, and encroaching over the cornea.[2] Histopathologically, it is an elastotic degeneration of the conjunctival collagen.[3] A pterygium may cause tear film instability, corneal astigmatism, and obscuration of visual axis apart from poor cosmesis. [4] Prevalence of pterygium varies in different races and geographical locations. It is maximum in between 30° North and 30° south of the Equator, which is known as the ‘pterygium belt’. A higher rate of double headed pterygium was also found in these locations. Prevalence of pterygium among Indians was found to be 7%.[5], [6] The incidence of double headed pterygium was found to be 2.5% in a study.[7]
Various surgical techniques are employed for pterygium excision. Conjunctival autografting has been proved to be superior to other grafting techniques.[8] Aim of this study was to evaluate the post-operative outcome of double headed pterygium excision followed by superior and inferior sutureless conjunctival autografts.
Materials and Methods
A retrospective study of the patients operated for double headed pterygium was done between 1st June 2018 and 30th June 2019 at a tertiary care hospital of southern Rajasthan.
Inclusion criteria
All the patients operated for a double headed pterygium within above mentioned time period were included in the study
Exclusion criteria
Patients with history of ocular trauma or chemical injuries.
Patients with recurrent pterygium.
Patients with pseudopterygium.
Patients with a follow-up period of <6 months.
Patients with conjunctival and lid abnormalities like symblepharon, entropion and ectropion.
A detailed history was taken including age, sex, occupation, duration of pterygium, history of chemical injuries, medical and surgical history. Unaided visual acuity was noted with a Snellen’s distant vision chart. Depending on the extent of corneal involvement the pterygium was graded as follows: Grade I-crossing the limbus, Grade II-midway between the limbus and pupil, and Grade III-crossing the pupillary margin. Routine blood investigations along with bleeding time(BT) and clotting time(CT) were accessed. All the surgeries were done by a single surgeon.
Surgical technique
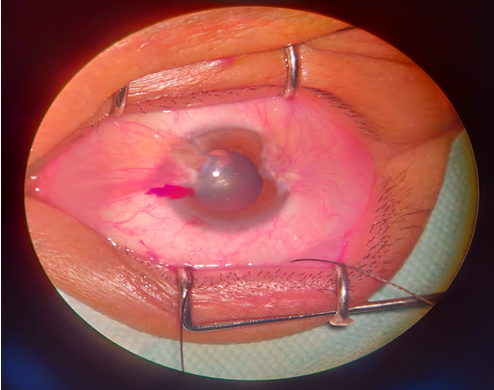
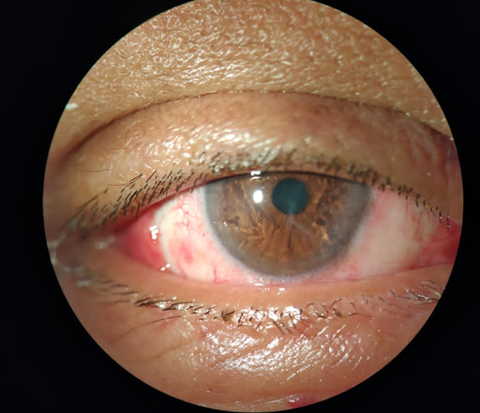
After giving peribulbar anaesthesia, painting and draping was done. Lids were separated by a wire speculum. A bridle suture for superior rectus was taken using 4-0 silk ([Figure 6]). According to the grading of pterygium, the larger pterygium was excised first. Careful small conjunctival incision was made parallel to the limbus, avoiding damage to the head of pterygium. The corneal epithelium 2mm beyond the head of pterygium was scraped off with crescent knife. The head was then removed by a combination of blunt dissection and traction. The pterygium affected conjunctiva (body of pterygium) was dissected carefully by avoiding damage to extraocular muscles. The residual tissue from cornea and limbus was scraped with crescent knife. Similar procedure was done for the other side. Size of the graft was measured in three directions over the bare sclera- (1) extent across limbus, (2) maximum circumferential extent and (3)distance from limbus on both nasal and temporal sides. 1 mm larger than the measured dimensions of the bigger bare sclera were marked on the superior conjunctiva with a gentian violet marker. Bridle suture was used to expose the superior conjunctiva. Xylocaine 2% was injected beneath conjunctiva to ensure good conjunctival separation from tenon’s capsule. The conjunctival graft was excised starting from the forniceal end; once the limbus was reached the graft was flipped over the cornea and Tenon′s attachments were dissected. The conjunctival graft was dissected on the limbal side with the help of crescent knife to include maximum limbal stem cells. It was then cut with the Vannas scissors. Graft was then placed over bare sclera with limbus-limbus orientation and epithelial side facing upwards. The graft is then allowed to set with autologous blood. Bridle suture was then released to expose inferior conjunctiva. The graft for the smaller bare sclera was then obtained from inferior conjunctiva following similar method and allowed to set for 10 minutes. Eye was then patched for 1 day. Post-operative assessment was done on next day. Patients were prescribed an eyedrop combination of moxifloxacin and dexamethasone starting with 6 times daily and then tapered over 4 weeks. Carboxymethylcellulose 0.5% drops were also prescribed for 4 times daily for 4 weeks. Patients were reviewed at 1 week, 1 month ([Figure 7]), 3 months and 6 months post-operatively. A fibrovascular tissue crossing the corneo-scleral limbus onto the clear cornea was considered as a recurrence.
Results
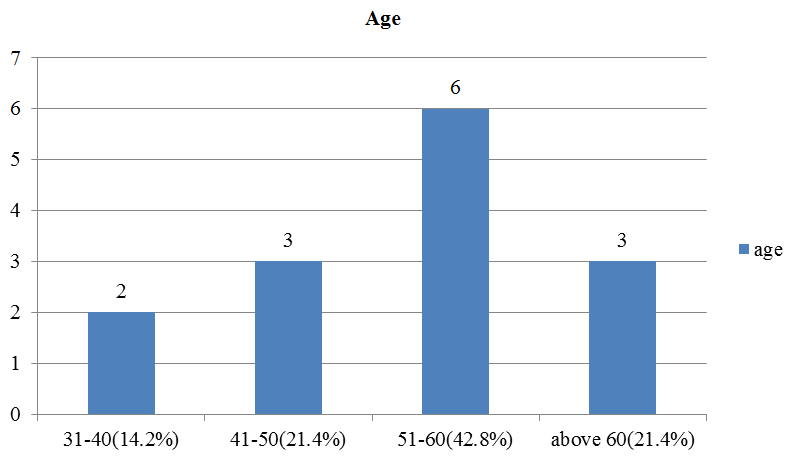
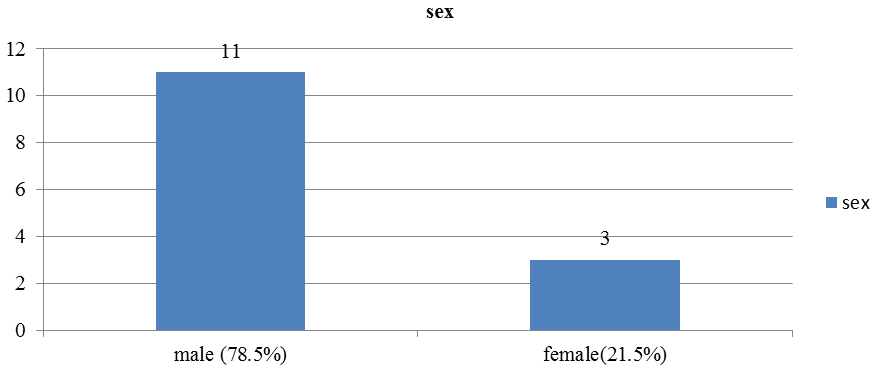
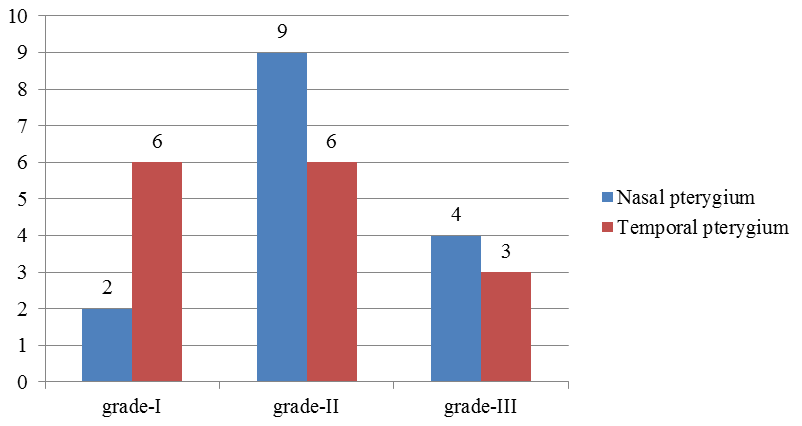
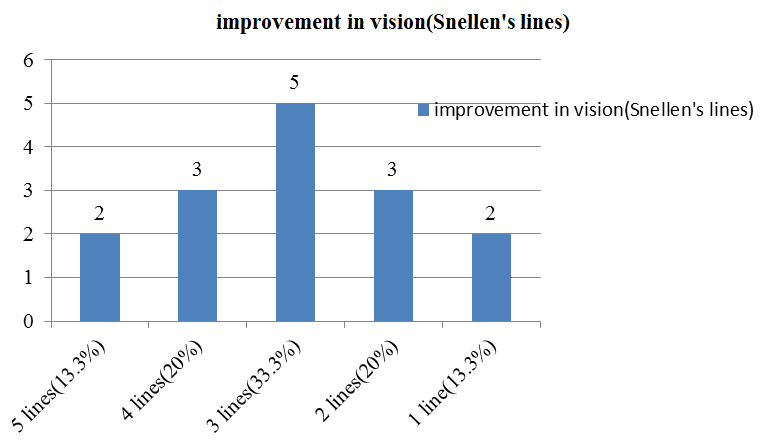
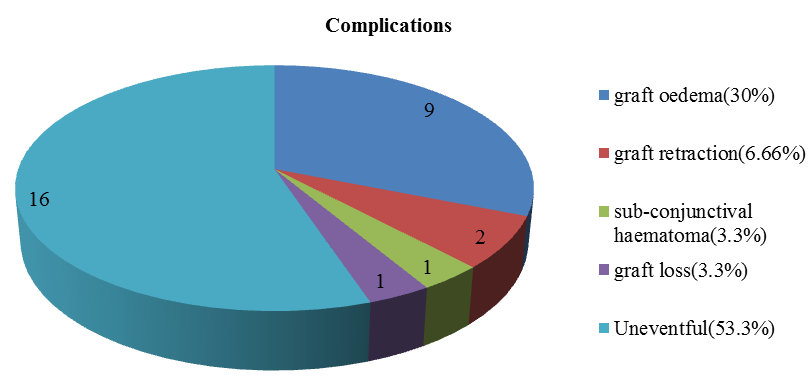
A total of 14 patients with primary double headed pterygium were operated by a single surgeon using the above mentioned technique. Retrospective analysis was done. 13(92.86%) patients were affected unilaterally and 1(7.14%) patient had bilateral double headed pterygium. 11(78.5%) out of 14 were male and 3(21.5%) were female. Mean age of patients was 46.5 ± 15.5 years. Out of 15 nasal pterygia, 2(13.3%) were grade-I, 9(60%) were grade-II and 4(26.6%) were grade-III. Out of 15 temporal pterygia, 6(40%) were grade-I, 6(40%) were grade-II and 3(20%) were grade-III. Mean follow-up was 12 ± 6 months. No significant intra-operative complications were noted. Post-operative vision improvement was recorded at 3 month follow-up with a Snellen’s distant vision chart. An average of 3 ± 2 Snellen’s lines improvement was noted in unaided vision. Most common post-operative complication was graft oedema in 9 grafts out of 30 (30%). Graft retraction was found in 2 grafts (6.66%). Sub-conjunctival haematoma was found in 1 graft (3.3%). Graft loss was found in 1 graft (3.3%).
Discussion
Double headed pterygium is a rare occurrence, but southern Rajasthan has a relatively high prevalence being located in the ‘pterygium belt’ at 24° north of equator and the occupations practised here involve prolonged exposure to sunlight. Various surgical techniques are available for pterygium but amniotic membrane grafts are costly and have a limited availability, mitomycin C includes hazardous complications like scleral thinning and melting. Use of sutures for grafts includes post-operative irritation and granuloma formation. Fibrin glue is also costly and chances of transmitting infections are high. Currently employed vertically split graft technique does not ensure limbus-limbus orientation on both bare sclera which may increase the chances of recurrence. Suture-less, glue-less conjunctival autograft is widely accepted and preffered technique because of the cost effectiveness, lesser surgical time and low rates of complications. The purpose of taking inferior conjunctival grafts was to maintain the limbus-limbus orientation of both the bare sclera defects which would lead to lesser recurrences. No recurrences were found in our study within 6 months of follow up, which shows the effectiveness of this technique. Graft oedema and sub-conjunctival hematoma were medically managed by topical moxifloxacin and dexamethasone eyedrops and resolved over further follow up. Graft retractions are subject to smaller grafts and incomplete separation of Tenon’s from the conjunctival graft. Graft loss may be due to thick graft and weak adhesion to bare sclera but even after 6 months of follow up there was no recurrence noted.
Conclusion
Double headed pterygium surgery with a superior and an inferior bulbar conjunctival autograft with autologous blood is a safe, cost effective and well tolerated surgery. It is relatively less time consuming and has promising results in our study. The limitations of this study might be lesser number of subjects and shorter duration of follow-up.
Source of Funding
None.
Conflicts of Interest
There are no conflicts of interest.
References
- S Duke-Elder, A G Leigh, S Duke-Elder. . System of Ophthalmology 1965. [Google Scholar]
- Ashok Garg, E L Essam, Toukhy. Surgical and medical management of Pterygium. gium 2009. [Google Scholar]
- W H Spencer. . Ophthalmic pathology. An atlas and textbook 1985. [Google Scholar]
- Patricia A. Jaros, Vincent P. DeLuise. Pingueculae and pterygia. Surv Ophthalmol 1988. [Google Scholar]
- M E Cameron. . Pterygium throughout the world 1965. [Google Scholar]
- Marcus Ang, Xiang Li, Wanling Wong, Yingfeng Zheng, Daniel Chua, Ainur Rahman. Prevalence of and Racial Differences in Pterygium. Ophthalmol 2012. [Google Scholar]
- V Dolezalová. Is the occurrence of a temporal pterygium really so rare?. Ophthalmol 1977. [Google Scholar]
- A Alpay, S H Uğurbaş, B Erdoğan. Comparing techniques for pterygium surgery. Clin Ophthalmol 2009. [Google Scholar]
How to Cite This Article
Vancouver
Punjabi S, Patel N, Bhutna K. Outcome of double headed pterygium surgeries with conjunctival autograft adhered by autologous blood: a retrospective study [Internet]. Indian J Clin Exp Ophthalmol. 2025 [cited 2025 Sep 08];6(2):240-243. Available from: https://doi.org/10.18231/j.ijceo.2020.052
APA
Punjabi, S., Patel, N., Bhutna, K. (2025). Outcome of double headed pterygium surgeries with conjunctival autograft adhered by autologous blood: a retrospective study. Indian J Clin Exp Ophthalmol, 6(2), 240-243. https://doi.org/10.18231/j.ijceo.2020.052
MLA
Punjabi, Sharda, Patel, Nishant, Bhutna, Komal. "Outcome of double headed pterygium surgeries with conjunctival autograft adhered by autologous blood: a retrospective study." Indian J Clin Exp Ophthalmol, vol. 6, no. 2, 2025, pp. 240-243. https://doi.org/10.18231/j.ijceo.2020.052
Chicago
Punjabi, S., Patel, N., Bhutna, K.. "Outcome of double headed pterygium surgeries with conjunctival autograft adhered by autologous blood: a retrospective study." Indian J Clin Exp Ophthalmol 6, no. 2 (2025): 240-243. https://doi.org/10.18231/j.ijceo.2020.052
