Introduction
Diabetes mellitus is one of the common systemic problems affecting a variety of people worldwide. Epidemiological data suggests that there is an increasing incidence of diabetes mellitus in developing countries. By 2030, it is estimated that global prevalence of diabetes would reach approximately 4.4%.1 Cataract is the second most common ocular complication of diabetes mellitus after diabetic retinopathy. Diabetes mellitus is a risk factor for development of cataract. Approximately two third of the diabetic population shows evidence of cataract. Diabetes mellitus influences the function and morphology of the lens. Cataracts occur at an early age in diabetics compared to non- diabetics2 and 2-5 times more common in diabetic patients. So cataract surgery in diabetics is often done earlier. Apart from visual improvement, diabetic patients need cataract surgery for the assessment and treatment of posterior segment pathology. In India approximately 20% of all cataract surgery is done in diabetics.3
Poor visual outcome after cataract surgery in diabetics associated with the severity of pre-existing retinopathy and diabetic maculopathy prior to the surgery. In diabetics, there is increased incidence of pigment dispersion and fibrinous reaction in the anterior chamber, development of posterior synechiae, increased risk of capsule rupture and vitreous loss. Diabetic patients are more prone to postoperative complications such as rubeosis iridis, neovascular glaucoma, macular edema (Diabetic and cystoid), severe inflammation, (Iritis, uveitis, endophthalmitis) vitreous hemorrhage, synechiae to IOL, retinal detachment and corneal decompensation. Diabetic are more prone to develop posterior capsule opacification postoperatively.
Higher incidence of diabetes in developing countries such as India necessitates an assessment of the outcome of cataract surgery in diabetic patients. Hence this study is planned to asses and compare outcome of cataract surgery in diabetics.
Materials and Methods
Source of data
The present study was done in the department of Ophthalmology of B.L.D.E.U’S Shri B.M. Patil Medical College, Hospital and Research Centre, Vijayapura.
Pre-operative evaluation
All patients were admitted to the hospital one day prior to surgery. Consent was obtained from patients after explaining about the study in detail and institutional ethical committee approval was taken All these patients underwent pre-operative evaluation and complete ophthalmic examination, including a thorough history with required demographic data. Systemic evaluation was also carried out.
Ophthalmic examination included
Best corrected visual acuity.
Slit lamp examination and grading of cataract done according to LOCS III
IOL calculation using srk ii/t formula.
Posterior segment evaluation using indirect ophthalmoscopy, b- scan and oct if required.
Blood investigations: Rbs, Fbs, Ppbs, HbA1c, HIV and HBsAg was done.
Surgery
In all patients small incision cataract surgery with posterior chamber intraocular lens implantation under peri-bulbar anaesthesia was done.
Manual small incision cataract surgery technique
Under aseptic precautions eye was draped, a wire speculum was placed and superior rectus bridle suture was passed and clamped on to the towel. A fornix based conjunctival flap was made. Superficial sclera vessels were cauterized. A 6mm straight incision was made on the scleral 1.5 to 2mm away from the limbus. Sclero-corneal tunnel was made. A side port entry was made with paracentesis knife. Capsule is stained using trypan blue dye through the side port. A continuous curvilinear capsulorhexis was performed. Anterior chamber was entered with angled keratome
Hydro-dissection was performed. Nucleus prolapsed into the anterior chamber and delivered out using either sandwich technique. Cortical matter aspired with simcoe cannula, a PMMA IOL was implanted in the capsular bag. Anterior chamber was formed with ringer lactate, side port opening was sealed by stromal hydration. Sub-conjunctival 0.2ml (40mg/ml) Gentamycin and 0.3ml (4mg/ml) Dexamethasone, total 0.5CC was given at end of procedure. Pressure pad was applied at end of surgery.
At all subsequent visits, patients were subjected to the slit-lamp examination, fundus examination and visual acuity recording. All data were analyzed using SPSS software v.23.0 and Microsoft office 2007. Chi-square (χ2) test was used for association between two categorical variables. The difference of the means of analysis variables between two independent groups was tested by unpaired t test. If the p-value was < 0.05, then the results were considered to be statistically significant.
Post-operative evaluation
On the first post-operative day, all the patients were subjected to detailed slit lamp examination and fundus examination. Visual acuity was assessed. On discharge all patients were put on corticosteroid and antibiotic combination eye drops 6 times per day, which was then tapered over a period of 6 weeks. The patients were asked to review at 1 week and 1 month from the date of surgery. At all subsequent visits, patients were subjected to the slit-lamp examination, fundus examination and visual acuity recording. At all subsequent visits, patients were subjected to the slit-lamp examination, fundus examination and visual acuity recording Standardization Uveitis Nomenclature (SUN) working group. Posterior capsular opacification (PCO) was done by EPCO(Evaluation of PCO) grading. The final visual outcome was recorded using snellen’s visual acuity chart and the values were converted to log MAR units for statistical analysis
Results
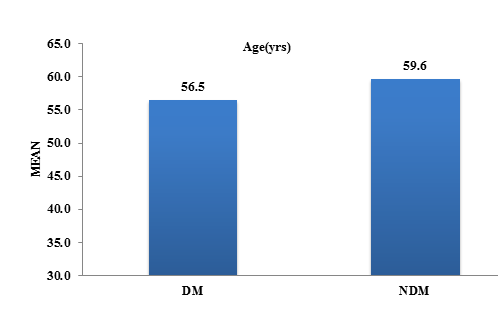
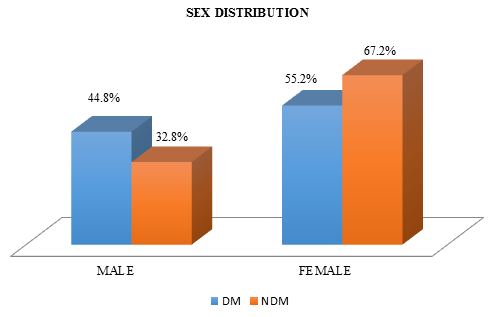
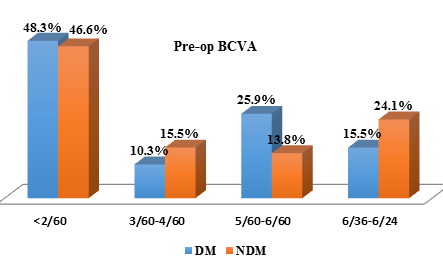
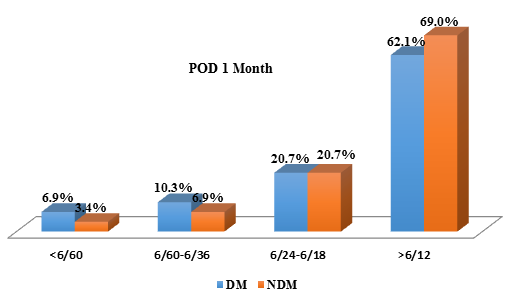
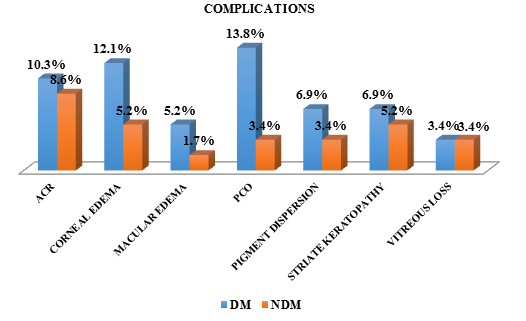
The study group consists of 58 eyes of diabetics and 58 eyes of non-diabetics that underwent small incision cataract surgery with posterior chamber intraocular lens implantation under peri- bulbar block. The mean age group of patients in diabetic group was 56.5±7.4 and 59.6±5.2 in non-diabetic group (Figure 1). In this study, in diabetic group 26 (44.8%) were males and 32 (55.2%) were females. Among non-diabetic 19 (32.8%) were males and 39 (67.2%) were females (Figure 2). Out of 58 patients in the diabetic group, 34 (58.6%) had good glycaemic control (FBS:70-100mg/dl). Remaining 24 (41.4%) patients had high blood sugar levels (>100mg). Their blood sugar levels controlled eventually and they were operated (Table 1). Majority of patients 32 (55.2%) were recently diagnosed diabetics with duration of disease being less than 3 years. There were about 8 (13.8%) patients with duration of disease being more than 10 years (Table 2). Hypertension though the most frequent co-morbid disease in both the groups, its more frequent amongst diabetics as seen in this study, that is 20 (34.5%) compared with 12(20.7%) of the non- diabetic patients. The mean best corrected pre-operative visual acuity in both the groups was calculated in logMAR units. The mean preoperative best corrected visual acuity in the diabetic group was 1.60±0.81 and in non-diabetic group was 1.62±0.87 (Figure 3. The final visual outcome was recorded using snellen’s visual acuity chart and the values were converted to log MAR units for statistical analysis. Majority of the patients 36 (62.1%) in the diabetic group and 40 (69%) in the non-diabetic group had visual acuity of 6/12 or better at the end of 4 weeks of follow up (Figure 4). The mean post-operative best corrected visual acuity in log MAR units in the diabetic group was 0.39±0.32 and in the non-diabetic group was 0.32±0.27 on comparing the post op values in both the groups the p value was (0.23) which was not statistically significant. On comparing the pre-operative and post-operative visual acuity in both the groups the p value (<0.001) was statistically significant. Posterior capsular opacification (13.8%) was the most common complication seen in diabetic group, followed by corneal edema and anterior chamber reaction (Figure 5). Pigments over IOL were seen in 4 (6.9%) of the cases in diabetics as compared to 2 (3.4%) in the Non-diabetic group. Cystoid macular edema was seen in 3 (5.2%) diabetic and 1 (1.7%) non-diabetic patients.
Table 1
Distribution of cases according to FBS
| FBS | N | % |
| Normal (70-100) | 34 | 58.6 |
| High(>100) | 24 | 41.4 |
| Total | 58 | 100 |
Table 2
Distribution of complications between study groups
Discussion
In this study, highest number of patients were in the age group of 51-60 years that is in diabetic 26 (44.8%) & 32 (55.2%) in non-diabetic group. The mean age group of the patients in diabetic group was 56.5±7.4 and 59.6±5.2 years in control group. Framingham and other eye studies indicate a 3-4 fold increased prevalence of cataract in patients with diabetes under 65 years and up-to a two-fold excess prevalence in patients above 65 years. In this study, in diabetic group 32 (55.2%) were females and 26 (44.8%) were males. Among the non-diabetics, 19 (32.8%) were males & 39 (67.2%) were females. Various studies have proven the prevalence of cataract itself is more common in females than males. In the Framingham eye study also senile lens changes were more common in women. Age related cataract is a bilateral condition, one eye affected earlier than the other.4
Glycemic control was assessed using fasting blood sugar levels at the time of admission. Of the 58 patients in the diabetic group, 24 (41.4%) had high blood glucose level (FBS: >100mg/dl). Their blood sugar was controlled and they were operated. 34 (58.6%) patients had normal blood sugar levels at the time of examination (70-100mg/dl). All 58 diabetic patients were on treatment for type 2 diabetes mellitus with either injection insulin or oral hypo-glycemic agents.
We also looked at the duration of disease among our diabetic group. Majority of patients 32 (55.2%) were recently diagnosed diabetics with duration of disease being less than 3 years. There were about 8 (13.8%) patients with duration of disease being more than 10 years The risk for cataract formation and diabetic retinopathy is more in patients with longer duration of diabetes and in those with poor metabolic control.5 The pathways by which hyperglycemia leads to cataract are still uncertain but they are probably due to modification of the lens proteins leading to advanced glycation end products (AGEs) formation or modification of the AT Pase pumps, leading to osmotic stress, or both.
Hypertension though the most frequent co-morbid disease in both the groups, its more frequent amongst diabetics as seen in this study, that is 20 (34.5%) compared with 12(20.7%) of the non- diabetic patients. A similar high incidence was seen in study by Onakpoya H Oluwatoyin et al,6 in which hypertension was seen in 60.9% compared with 26.1% in non-diabetic group.
The other systemic co-morbidities in our study were ischemic heart disease in 2 (3.4%) in diabetics and 3 (5.2%) in the non-diabetic group. Asthma another comorbid disease seen in 2 (3.2%) diabetic and in 3 (5.2%) non-diabetic patients. Hypothyroid was another comorbid disease which was seen in one diabetic patient.
In this study, majority of the patients had poor pre-operative visual acuity. The mean best corrected pre-operative visual acuity in both the groups was calculated in logMAR units. The mean preoperative best corrected visual acuity in the diabetic group was 1.60±0.81 and that in non-diabetic group was 1.62±0.87.
In this study all the patients in both the groups had various grades of immature cataract. In our study, we found that the prevalence of mixed cataract was higher, more than two times of monotype cataract. In the mixed types, the most common type was a combination of nuclear cataract(NC), cortical cataract (CC), and posterior sub-capsular cataract (PSC), followed by the combination of CC and PSC. In the monotype cataracts, the most common cataract CC followed by NC and PSC. The methodology adopted was that of Lens Opacification Classification System (LOCS) III grading.
All patients underwent cataract extraction by SICS with PCIOL implantation, and all the procedures were done by the same surgeon. On examination of the patients on post-operative day one, corneal edema was found in 7 (12.1%) and 3 (5.2%) of the cases in diabetic and non-diabetic groups respectively which was considerably higher in diabetics compared to non-diabetics. Striate keratopathy was found in 4 (6.9%) of the diabetics compared to 3 (5.2%) in nondiabetics.
In this study corneal edema was found in 7 (12.1%) and 3 (5.2%) of the cases in diabetic and non-diabetic groups respectively. Larsson et al.7 have shown that diabetes has been associated with structural changes in corneal endothelial cells such as polymegathism and pleomorphism. The cornea has been reported to be thicker in eyes of diabetic patients than in eyes of non-diabetic subjects.8 Cataract extraction and IOL implantation causes trauma to the already compromised corneal endothelium and causes corneal edema. Hence compared with non-diabetic patients, eyes of diabetic patients showed more damage in corneal endothelial cells after cataract surgery and a delay in the post-operative recovery of corneal edema.
In this study the development of PCO in diabetics was 8 (13.8%) compared to 2 (3.4%) in non- diabetics, at the end of 4 weeks, confirming the finding of increase in incidence of PCO in diabetics as shown in previous studies. Study by Ebihara Y et al.9 also showed significant increase in PCO in diabetic compared to non- diabetic patients. A study by Hyashi K et al. also showed significant increase in PCO in diabetics after cataract extraction compared to nondiabetics.
Pigments over IOL were seen in 4 (6.9%) of the cases in diabetics as compared to 2 (3.4%) in the Non-diabetic group. Previous studies it has been shown that, there is increased pigment dispersion in diabetic patients undergoing cataract extraction and IOL implantation. This may be comparable with: Onakpoya H Oluwatoyin et al5 showed increase amount of pigment dispersion occurring in diabetic patients i.e 6 in diabetics and 1 in non-diabetic patient.
In this study, total 6 (10.3%) eyes in the diabetic group and 5 (8.6%) eyes in the non-diabetic group had anterior chamber reaction. Diabetic patients had more anterior chamber reaction compared to non-diabetics. Similar observations were made in following studies “Onakpoya H Oluwatoyin et al.,5 N D George et al. and Mechini et al. reported intraocular inflammation and its sequelae as the most common complication of their study”.
Ivancic et al.1 reported inflammatory reaction fibrinous uveitis & PCO as the most common complications of cataract surgery among diabetics.
Longer duration of surgery is associated with increased post-operative inflammation. Fibrinous exudates & posterior synaechiae was not found in our study compared to previous study. None of the patients in our study had anterior segment neovascularization, as reported in previous studies.
In this study cystoid macular edema is seen in 3 (5.2%) diabetic and 1 (1.7%) non-diabetic patients. In diabetics with or without evidence of diabetic retinopathy the blood-aqueous barrier is impaired, it leads to inflammation and development of a cystoid macular edema, a process that is exacerbated by cataract surgery.10
The final visual outcome was recorded using snellen’s visual acuity chart and the values were converted to logMAR units for statistical analysis. Majority of the patients 36 (62.1%) in the diabetic group and 40 (69%) in the non-diabetic group had visual acuity of 6/12 or better at the end of 4 weeks of follow up. The mean post-operative best corrected visual acuity in log MAR units in the diabetic group was 0.39±0.32 and in the non-diabetic group was 0.32±0.27. Similar study done by Raj Kumar Gupta et al. consisting of 50 diabetics and 50 non-diabetics, the post-surgical visual acuity in the diabetic and non-diabetic group was found to be 0.30 and 0.37 respectively at one month post-op.11 On comparing the post op values in both the groups the p value was 0.23 which was not statistically significant. On comparing the pre-operative and post-operative visual acuity in both the groups the p value (<0.001) was statistically significant indicating that both the groups had good visual outcomes following surgery. This indicate that cataract surgery in diabetics without retinopathy led to favorable and comparable visual outcomes to that of non-diabetics.
Conclusion
In this comparative study, the pre-operative best corrected visual acuity was compared to the post-operative best corrected visual acuity in both the groups and the P value was statistically significant (p=0.01). The post-operative complications that were observed during the period of this study were posterior capsular opacification, corneal edema, striate keratopathy, anterior chamber reaction, pigment dispersion over IOL, cystoid macular edema and vitreous loss. These were significantly more in the diabetic group when compared to the non- diabetics. Therefore, we concluded that small incision cataract surgery in diabetics without diabetic retinopathy yields similar visual outcomes as non-diabetics. There is a higher incidence of post-operative complications among diabetics, so extra care should be taken intra-operatively and during post-op follow up.