Introduction
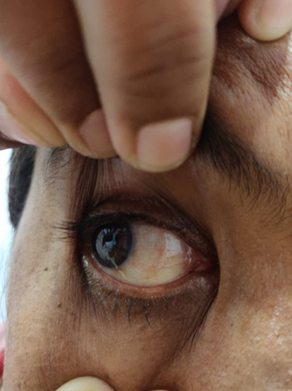
Pterygium is a growth onto the cornea, usually nasally, of fibrovascular tissue that is continuous with th e conjunctiva. It occurs in the palpebral fissure area, much more often nasally than temporally, although either or both (“ double ” pterygium) occur.1 Pterygium is associated with ultraviolet light exposure. It occurs at highest prevalence and most severely in tropical areas near the equator and to a lesser and milder degrees in cooler climates.2,3 Both blue and ultraviolet light have been implicated in its causation, as demonstrated in watermen.2 Pterygium needs to be treated when they encroach upon the visual axis, induce significant regular or irregular astigmatism, or become cosmetically bothersome. The primary aim of pterygium surgery is to excise the pterygium and prevent its recurrence. For small pterygium simple excision of the pterygium on the cornea and sclera is sufficient but for the large pterygium the goal of treatment is to prevent recurrence. Surgeries such as autologous conjunctival graft, amniotic membrane or the advancement flap are well established but the recurrence remains to be the problem. Recurrence after simple excision with bare sclera is high and that of with graft is minimal so several studies showed minimal recurrence with autoconjunctival graft and amniotic membrane graft but amniotic membrane is not cost effective and autoconjunctival graft done at the cost of excision and grafting of a considerable portion of normal healthy conjunctiva and limbal cells which is retrieved usually from the superior part of bulbar conjunctiva which is the preferred site of glaucoma filtration surgery like trabeculectomy and the presence of a normal superior conjunctiva is a very important factor determining the success of a glaucoma a filtration surgery.4 There were radical surgeries with a purported recurrence rate near 0 %, such as “ Pterygium Extended Removal Followed by Extended Conjunctival Transplant ” (PERFECT), have recently been introduced.5,6 However, these radical procedures have not been popularized due to the extensive labor involved and the complexity of the technique.5,6 The aim of our study is to find the effectiveness of the conjunctival advancement flap with sutures, a technique to treat the Pterygium, saving the normal conjunctiva for the future glaucoma surgery if needed and compare the surgical outcome with graft on autologous serum.
Aim
To study the stability, recurrence rate and inflammation of the extended conjunctiva following subconjunctival excision of pterygium by conjunctival advancement flap with sutures technique and compare these results with conjunctival graft on autologous serum.
To compare the results of above 2 techniques, in terms of efficacy, coast effectiveness and structural stability.
Materials and Methods
This was a prospective study to compare and analyse 114 cases of nasal pterygium at the Department of Ophthalmology of Shri Bhausaheb Hire Government Medical College Dhule, during a period of June 2018 to June 2019
A pproval from the institutional ethical committee was obtained prior to study. Patients with primary progressive nasal pterygium from grade 1 to 4 were included and patients with Conjunctival masses mimicking pterygium such as ocular surface squamous neoplasia (OSSN), pseudopterygium and recurrent pterygium were excluded from our study. The clinical characteristics of the pterygium were classified using a modified classification system7. It considers the length of corneal involvement (stage), vascularity and tissue thickness (corneal and conjunctival part) of pterygium.
Table 1
Clinical classification of pterygium
Patients were explained about the procedure and an informed written consent was obtained from the patients. After a thorough history examination was done, which included visual acuity (BCVA), slit lamp examination of pterygium along with grading and remaining anterior segment, posterior segment, m easurement of intraocular tension. Base line investigations such as Hemogram, random blood sugar, HIV, HBsAg, ECG were done and a fitness for surgery was obtained. All surgeries were performed with specific technique.
In advancement flap procedure local subconjunctival infiltration anesthesia was given. The eye was painted, draped and eye speculum inserted. The body of Pterygium was meticulously excised taking care of the underlying medial rectus muscle. The pterygium head was meticulously separated from the underlying cornea using a Cresent blade or No. 15 Bard-Parker blade. After the entire pterygium was freed from the ocular surface, the pterygium body and conjunctiva were excised. Haemostasis was obtained. The overlying conjunctiva was then dragged over the bare sclera and was secured at the limbus with pref erably single 10-0 nylon suture, double sutures if needed. Following the procedure, patients were advised to administer antibiotic and prednisolone eye drop 6 times daily in the first week tapered gradually over 4 weeks. Lubricating eye drops (Hydroxypropyl methylcellulose) 4 times daily and Lubricating eye ointment two times a day for 1month.
In conjunctival graft on autologous serum the peribulbar block given, graft was taken from superior or superotemporal quadrant of conjunctiva, limbus to limbus graft placement was done, graft is then secured with the help of autologous serum and blood. Post operative m edication and follow up was same as that of advancement flap with suture.
Patient was followed up at 1 week, 1month, 3 months and 6 months, during follow up visits, Sta bility of overlying conjunctiva, inflammation and evidence of recurrence were recorded. Recurrence of pterygium was monitored, Grade 1 to 3 (Table 1) were considered as “ no-recurrence ” and grade 4 (Table 1) was considered as “recurrence”.
Results
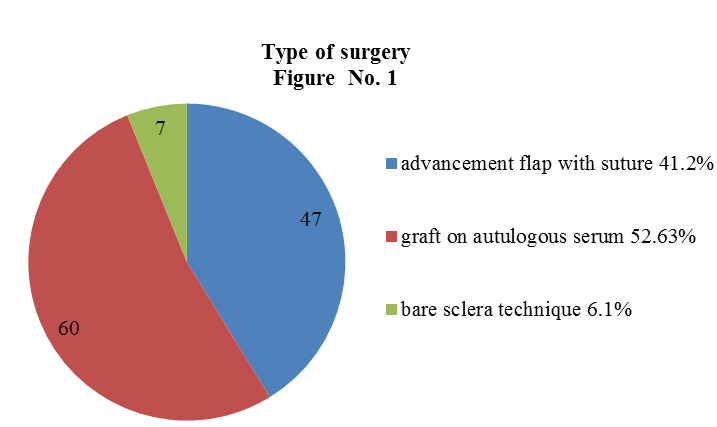
Out of 114 patients, 47 patients undergone advancement flap with sutures, 60 patient’s undergone conjunctival graft on autologous serum while 7 patients had undergone bare sclera technique.
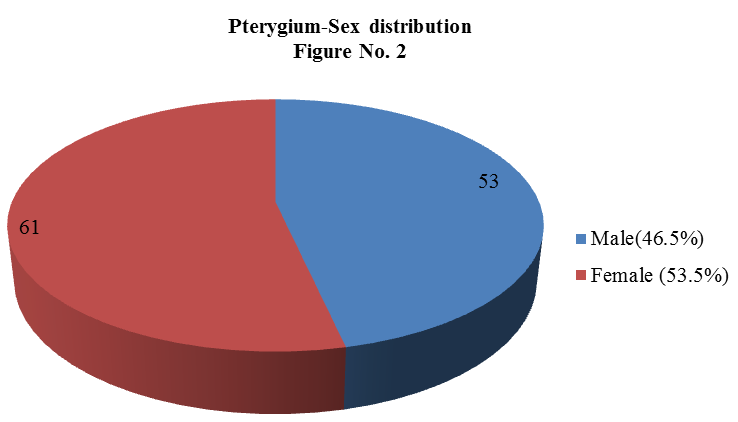
Out of 114 patients no significant difference in sex distribution 61 were females, 53 were males, as shown in figure 2.
Maximum number of the patients belonged to 40 to 60 years of age group that is 80 patients (70%), 15 patients were between 20- 40 years age group (13.15%) and 19 patients were between 60 years and above age group(16.6%). None of the patient was less than 20 years old (0%)
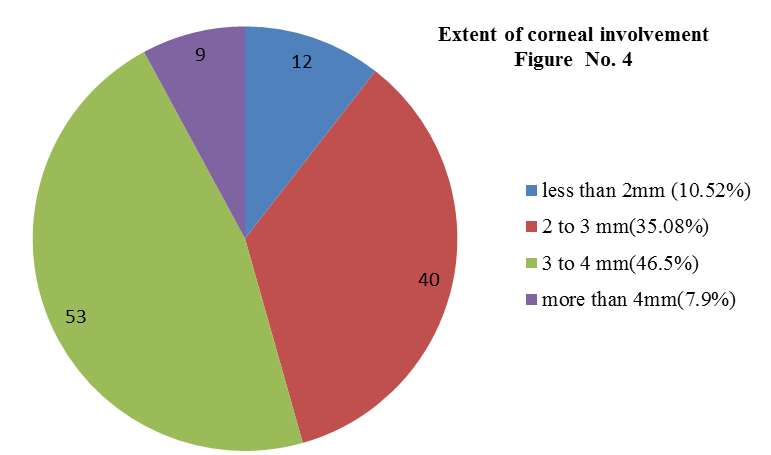
Extent of corneal involvement- Among 114 patients 12cases(10.52%) had less than 2mm corneal involvement40 cases (35.08%) had 2mm to 3mm corneal involvement 53 cases (46.5%) had 3mm to 4mm corneal involvement 9 cases (7.9%) has more than 4mm corneal involvement
During 6 month follow up of all 114 patients
Among 47 patients of advancement flap with sutures – None of the patient had displacement of the flap so the post operative stability was very good with this group of patients. Post operative Suture sight inflammation and irritation was found in 9(19.14%) patients of this group which was significant as compared to the other group and one patient (2.12%) had recurrence of pterygium following this procedure.
Table 2
| S.No | Findings | Advancement flap | Grafton Autologous Serum |
| 1 | Graft Instability | 0(0%) | 7 (11.6%) |
| 2 | Postoperative inflammation | 9(19.14%) | 2(3.33%) |
| 3 | Recurrence | 1(2.12%) | 1(1.66%) |
Showing comparison between two types of pterygium surgery
Among 60 patients of graft on autologous serum – Graft displacement was found in 7(11.60%) cases ,stability is lesser with this group. One patient had tenons cyst/granuloma fo rmation at the site from where graft was taken and one patient had recurrence (1.66%). Post operative inflammation and irritation was found in only 2 cases out of 60
Among 7 patients who had undergone bare sclera technique- 3 patients had recurrence. None had post operative inflammation and irritation
Discussion
According to our study pterygium is most common in age group of 40 to 60 years that is 80 patients (70%) and majority of patients were females-61(53.5%), While 53(46.5%) patients were males this results are comparable with the study conducted by Chen CL et al8 in their study, incidence was higher in the age group of more than 40 years and the risk increases as the age increases along with female preponderance of 64%.
In our study the recurrence rate is very comparable, following conjunctival advancement flap with suture it is 2.12% while that of following conjunctival graft on autologous serum is 1.66%. As stated in Toker E et al, none of the surgical technique is best without the risk of recurrence. Soo Hyun Kwon et al9 in their study describes the recurrence pattern of pterygium after excision with conjunctival autografting as of 12.1% with 3 different mor phologic patterns as regrowth over the epithelial defect, transformation of the conjunctival graft into the pterygial tissue, regrowth from remaining pterygial tissue. Pterygium consist of epithelium which shows minimal abnormality except at the head of pterygium where there can be stratified squamous change, the main pathology is at the level of stroma where the connective tissue shows fibrinoid changes.10 Hence to preserve the epithelium over the pterygium doesn’t contribute to recurrence as it is histologically normal and a meticulous removal of the subepithelial connective tissue and stroma almost eliminates the pathology. Similarly we suggest that the thorough dissection and excision of subconjunctival tissue will reduce the recurrence rate. Post operative suture sight inflammation and irritation was found in our study which can be eliminated with the use of soft bandage contact lens es as it was done in Kim et al11
In conjunctival autografting mainly superior conjunctival graft is harvested which is the site for glaucoma filtration surgery if needed in future. It is a major disadvantage, so in glaucoma suspected patients advancement flap can be a choice of surgery. Shrestha A et al12 and Syam PP et al.9 also suggested the same findings as of our study.
However the other drawback of obtaining healthy conjunctiva from elsewhere can lead to conjunctival scarring, risk of symblepharon, tenons cyst formation, granuloma formation at the site of removal of normal conjunctiva etc. subconjunctival excision of pterygium with conjunctival advancement flap prevents such donor site related complications and moreover the superior conjunctiva is left intact so as to preserve the glaucoma filtration site. In our study graft instability was found in graft on autologous serum of 7 cases (11.6%) and it was comparable with the study performed by Sumita Karandikar et al, they have three cases (15%) of graft on autologous serum, showing graft retraction and needed secondary intervention, also they stated that. graft stability was least in autologous serum group.13
Conclusion
Pterygium excision by Conjunctival advancement flap with sutures is indicated in glaucoma patients and glaucoma suspects, it is cost effective and less time consuming technique to treat pterygium. Technical ly it is easier as compared to graft on autologous serum. It is a good technique where incidence of pteygium is more. However persistent redness, inflammation, itching following surgery are limitations of the study. It saves the normal superior conjunctiva for glaucoma filtration surgery. The recurrence rates are comparable to the current management methods like conjunctival autografting. Post operative stability is good, no graft displacement seen.